NYS Medicaid Telehealth
NYS Medicaid Telehealth News:



What is telehealth?
Telehealth is defined as the use of electronic information and communication technologies to deliver health care to patients at a distance. Medicaid covered services provided via telehealth include assessment, diagnosis, consultation, treatment, education, care management and/or self-management of a Medicaid member.
The NYS Medicaid program covers four types of telehealth modalities: audio only, audio/visual, remote patient monitoring, and store-and-forward.
General Information FAQs
1: Does NYS Medicaid cover services offered via telehealth?
NYS Medicaid covers services a broad range of services when delivered via telehealth. Comprehensive guidance outlining coverage policies can be in the June 2021 edition of Medicaid Update.2: Is there additional guidance for Article 31 clinics, Article 32 clinics, and Article 16 clinics?
Yes, the Office of Mental Health, the Office for People with Developmental Disabilities, and the Office of Addiction Services and Supports publish separate guidance on telehealth and regulations that will align with state law and Medicaid payment policy for Medicaid enrollees being served under their authority. Facilities that integrate services must follow the respective agency regulations that would apply.3: Which regulations apply if an Article 31 clinic or Article 32 clinic is integrated with an Article 28 clinic?
If an Article 28 clinic is integrated with an Article 31 clinic or an Article 32 clinic, the regulatory authority will depend on where the patient is located. If the patient is located in an Article 31 clinic, then the Office of Mental Health's telehealth regulations will prevail, and if the patient is located in an Article 32 clinic, then the Office of Addiction Services and Supports telehealth regulations will determine payment and the provision of services.4: Do Medicaid Managed Care Plans cover telehealth?
Medicaid managed care plans are required to cover telehealth in accordance with the provisions described in the June 2021 Medicaid Update.5: Are all Medicaid enrollees eligible to receive services via telehealth?
All Medicaid enrollees are eligible to receive services via telehealth provided that there is no reduction to the quality of care provided.6: What is an originating site?
The originating site is where the member is located at the time health care services are delivered to him/her by means of telehealth.7: Can a patient's home be an originating site?
The member's place of residence can be an originating site.8: What measures need to be taken to ensure the enrollee is truly located in their home?
If the patient has attested that their location (the originating site) is their home and their location is reflected in the medical record, that would satisfy due diligence.9: What would be considered a "temporary location" for an originating site?
A temporary location may include a momentary, non-permanent residence such as college housing, a homeless shelter, a camp or other transitional housing, vacation housing, or the home of family or non-relatives that is limited in time and not considered permanent. Temporary locations do not need to be within the state of New York.10: What is a distant site?
The distant site is any secure location within the United State or United States' territories where the telehealth provider is located while delivering health care services by means of telehealth. Any provider who is authorized to deliver Medicaid billable services, is eligible to provide services via telehealth, but services shall be appropriate for telehealth and shall be within the provider’s scope of practice.11: How is secure location defined?
Services provided by means of telehealth must be in compliance with the Health Insurance Portability and Accountability Act (HIPAA) and all other relevant laws and regulations governing confidentiality, privacy, and consent (including, but not limited to 45 CFR Parts 160 and 164 [HIPAA Security Rules]; 42 CFR Part 2; PHL Article 27-F; and MHL Section 33.13).12: Could a provider use their home office to provide telehealth services?
A provider can use their home office to provide telehealth services if the home office is a secure location.13: Are there any time requirements for telehealth encounters?
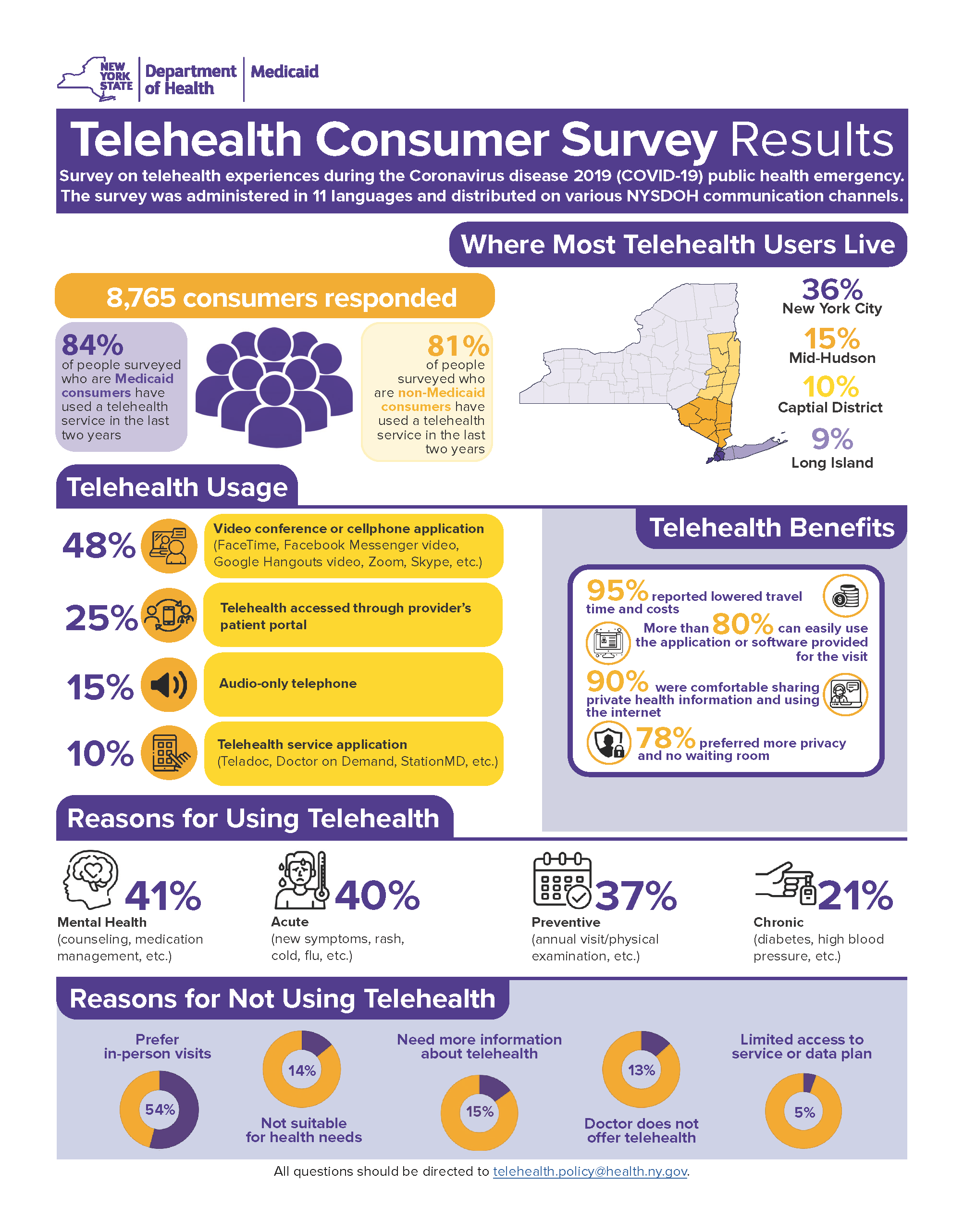
The totality of the communication of information exchanged between the physician or other qualified health care practitioner and the patient during the course of synchronous telehealth service must be of an amount and nature that would be sufficient to meet the key components and/or requirements of the same service when rendered via face-to-face interaction.Telehealth Consumer Survey
Telehealth Consumer Survey Results Infographic
The Telehealth Consumer Survey Results Infographic is also available in:
عربى (Arabic) (PDF)
Bেঙলি (Bengali) (PDF)
简体中文 (Simplified Chinese) (PDF)
Kreyòl Ayisyen (Haitian Creole) (PDF)
Italiano (Italian) (PDF)
한국어 (Korean) (PDF)
Polskie (Polish) (PDF)
русский (Russian) (PDF)
Español (Spanish) (PDF)
יידיש (Yiddish) (PDF)2022 Telehealth Consumer Survey QR Code Flyer
عربى (Arabic) (PDF)
Bেঙলি (Bengali) (PDF)
简体中文 (Simplified Chinese) (PDF)
English (PDF)
Kreyòl Ayisyen (Haitian Creole) (PDF)
Italiano (Italian) (PDF)
한국어 (Korean) (PDF)
Polskie (Polish) (PDF)
русский (Russian) (PDF)
Español (Spanish) (PDF)
יידיש (Yiddish) (PDF)The Telehealth Consumer Survey is closed and QR code shown on all flyers is no longer active.
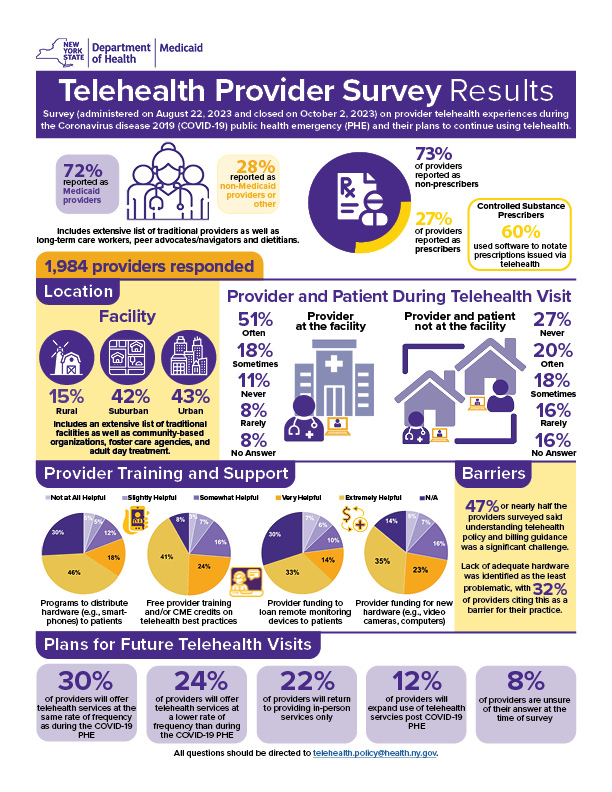
Telehealth Provider Survey
Telehealth Modalities
- Audio Only
- Audio/Visual
- Remote Patient Monitoring
- Store-and-Forward
Telehealth Modalities FAQs
1: What is Audio Only?
Audio-only uses two-way electronic audio-only communications to deliver services to a patient at an originating site by a telehealth provider located at a distant site.2: What is Audio/Visual?
Audio/Visual is the use of synchronous, two-way electronic audio-visual communications to deliver clinical health care services, which shall include the assessment, diagnosis, and treatment of a patient, while such patient is at the originating site and a telehealth provider is at a distant site.3: What is remote patient monitoring?
Remote patient monitoring uses digital technologies to collect medical data and other personal health information from members in one location and electronically transmit that information securely to health care providers in a different location for assessment and recommendations. Monitoring programs can collect a wide range of health data from the point of care, such as vital signs, blood pressure, health rate, weight, blood sugar, blood oxygen levels, and electrocardiogram readings.
4: What is store-and-forward?
Store-and-forward involves the asynchronous, electronic transmission of a member's health information in the form of patient-specific pre-recorded videos and/or digital images from a provider at an originating site to a telehealth provider at a distant site.
New York State Medicaid Medicaid Coverage of Telehealth
- DOH Medicaid Update
- NYS DOH Medicaid Telehealth Services During the Coronavirus Emergency Factsheet (PDF)
Current Telehealth Guidance
- NYS Medicaid Telehealth Provider Manual - Published 5/13/2024
Previous Telehealth Guidance - Medicaid Update Special Editions
- February 2023 Special Edition Medicaid Update Volume 39 Number 3 - Comprehensive Guidance on Telehealth Services After the COVID-19 Public Health Emergency - Updated 8/11/2023
- June 2021 Special Edition Volume 37 Number 7 - Telehealth Guidance - New York State Medicaid Update
- 2019 Special Edition Medicaid Update on Telehealth Coverage replaced with June 2021 Special Edition.
Eligibility for Medicaid Enrollees
All Medicaid enrollees are eligible to receive services via telehealth provided the services can effectively be delivered remotely and is not inconsistent with guidance issued by the Department.
Locations Where a Medicaid Member Can Receive Telehealth Services
Anywhere the member is located, including but not limited to the sites below. Reminder: the site must be Health Insurance Portability and Accountability Act (HIPAA) compliant and in agreement with current policies.
- Facilities licensed under Article 28 of the PHL (general hospitals, nursing homes, and diagnostic and treatment clinics);
- Facilities licensed under Article 40 of the PHL (hospice programs);
- Facilities as defined in Subdivision 6 of Section 1.03 of the Mental Hygiene Law (MHL) (includes clinics certified under Articles 16, 31 and 32);
- Certified and non-certified day and residential programs funded or operated by OPWDD;
- Private physician's or dentist's offices located within the state of New York;
- Any type of adult care facility licensed under Title 2 of Article 7 of the SSL;
- Public, private and charter elementary and secondary schools located within the state of New York;
- School-age child care programs located within the state of New York;
- Child daycare centers located within the state of New York; and
- The member's place of residence located within the state of New York or other temporary location within or outside the state of New York.
Locations Where Eligible Practitioners Can Provide Telehealth Services
Practitioners can provide telehealth services in any secure location within the fifty United States or United States' territories where the telehealth provider is located while delivering health care services by means of telehealth. Services provided by means of telehealth must be in compliance with the HIPAA and all other relevant laws and regulations governing confidentiality, privacy, and consent (including, but not limited to 45 CFR Parts 160 and 164 [HIPAA Security Rules]; 42 CFR, Part 2; PHL Article 27-F; and MHL Section 33.13). The medical record must document the physical location of the patient as well and the physical location of the telehealth provider.
Confidentiality
1: How is confidentiality maintained for telehealth encounters?
All services must be performed on dedicated secure transmission linkages that meet the minimum federal and state requirements. HIPAA requires that a written business associate agreement (BAA) or contract that provides for privacy and security of protected health information be in place between the telehealth provider and the supporting telehealth vendor. All confidentiality requirements that apply to medical records apply to services delivered by telehealth. The medical record must document the physical location of the patient as well as the physical location of the distant site practitioner.Patient Rights and Consents
1: What patient rights and consents need to be communicated to Medicaid enrollees?
The practitioner shall provide the Medicaid enrollee with basic information about the services they will be receiving via telehealth and the enrollee shall provide their consent to participate in services utilizing the telehealth technology. Telehealth sessions/services shall not be recorded without the member's consent. Culturally competent translation and/or interpretation services must be provided when the enrollee and the distant practitioners do not speak the same language.2: Where is the consent documented?
Documentation in the medical record must reflect that the enrollee was made aware of the patient rights policies.Failure of Transmission FAQs
1: What happens if there are technical issues, and the telehealth encounter is disrupted?
All telehealth providers must have a written procedure detailing a contingency plan in the case of a failure of transmission or other technical difficulty that renders the service undeliverable via telehealth. The policies and procedures must be made available upon audit.
2: Is partial payment available for a telehealth encounter that is disrupted?
No partial payment is available for disrupted telehealth encounters. If the service is undeliverable due to a failure of transmission or other technical difficulty, a claim should not be submitted to Medicaid.
Eligible Providers
Telehealth can be provided by Medicaid-enrolled providers and providers employed by Medicaid facilities or provider agencies who are authorized to provide in-person services. Telehealth provider is defined in Public Health Law § 2999-cc(2) and shall also include:
- Voluntary foster care agencies certified by the New York State Office of Children and Family Services and licensed pursuant to article twenty-nine-I of Public Health Law, and providers employed by those agencies.
- Providers licensed or certified by the New York State Department of Education to provide Applied Behavioral Analysis therapy.
- Radiologists licensed pursuant to Article 131 of the Education Law and credentialed by the site from which the radiologist practices;
- All Medicaid providers and providers employed by Medicaid facilities or provider agencies who are authorized to provide in-person services are authorized to provide such services via telehealth as long as such telehealth services are appropriate to meet a patient's needs and are within a provider's scope of practice.
Telehealth Providers FAQs
1: What are the licensure requirements for Article 28 facilities and private practitioners?
Practitioners providing services via telehealth must be New York State licensed and currently registered in accordance with NYS Education Law or other applicable law and enrolled in NYS Medicaid.
2: Are providers required to be credentialed and privileged at both the originating site and the distant in order to provide services via telehealth.
Providers must be credentialed and privileged at both the originating site and the distant site in order to provide telehealth services.
3: Can an out-of-state provider be a telehealth practitioner and provide services to a NYS Medicaid enrollee?
If the out-of-state provider is NYS licensed, enrolled in the Medicaid program and appropriately privileged and credentialled by the originating site, then they can provide services via telehealth.
Billing Rules for Telehealth Services
Billing Rules for Telehealth Services FAQs
1: Are there different fees for telehealth services?
There are no different fees for telemedicine services provided in Medicaid Fee-For-Service; they are paid the same fee as if they were delivered in-person. However, reimbursement for consultations provided via store and forward technology will be paid at 75% of the Medicaid fee for the service provided.
2: Are there different billable codes for teledentistry?
Teledentistry billing is explained the June 2020 issue of Medicaid Update: https://www.health.ny.gov/health_care/medicaid/program/update/2020/docs/mu_no11_jun20.pdf
3: If the originating site provider and the distant site provider belong to the same billing entity/network, can they both submit a claim?
Only one clinic payment will be made when both the originating site and the distant site are part of the same provider network/billing entity. In such cases, only the originating site can bill Medicaid for the telemedicine encounter.
4: If the Article 28 facility bills under APGs, is acting as the originating site, is there a way for the facility to recoup the administrative expenses if it only provides the telehealth encounter?
The Article 28 facility can bill Q3014 in order to recoup administrative expenses associated with the telehealth encounter.
5: Can a claim be submitted if the distant site practitioner is not located in the facility when they are providing telehealth services?
If the distant site practitioner is not located in the facility when they are providing telehealth services, the practitioner can submit a professional claim, and the facility can submit an institutional claim for Q3014.
6: Can an Article 28 provider be reimbursed for providing both a telehealth encounter and a face-to-face visit in the same day?
If the separate and distinct service by the same physician or other qualified health care professional occurs on the same day as the telehealth encounter, then the CPT code billed for the separate and distinct services must be appended with the 25 modifier.
7: Under what circumstances can a distant site provider delivering a telemedicine consult to a Medicaid enrollee who is a hospital inpatient be able to submit a claim?
A professional claim can be submitted only if the distant site provider is a physician. All other practitioner services are included in the APR-DRG payment to the facility. An Article 28 clinic, including FQHCs, cannot bill Medicaid for telehealth services provided to a hospital inpatient.Specific Billing Rules for Dual Eligibles FAQs
1: Will Medicaid reimburse for services not normally available under Medicare?
If the service provided is one that is not within the scope of services covered by Medicare (e.g., dental, store-and-forward) but it is an eligible telehealth service under Medicaid, then the telehealth encounter may be billed to Medicaid. If the service is normally covered by Medicare but only as a face-to-face encounter, then the telehealth encounter cannot be billed to Medicaid.
2: Will claims for dual eligibles follow the existing crossover process?
Claims for dually eligible individuals will follow the existing crossover process. The FQHC will bill Medicare first. A crossover claim will then be crossed over to Medicaid. Medicaid will pay the difference between the Medicare payment and the FQHC's PPS rate (4013).
Resources and Definitions
New York State Agencies: Telehealth Guidance
- Department of Financial Services (DFS)
- Office of Addiction Services and Supports (OASAS) - OASAS Laws, Regulations and Guidance (scroll to Legal section and search by keywords "telehealth" or "telepractice")
- Office of Children and Family Services (OCFS)
- Office of Mental Health (OMH)
- Office for People with Developmental Disabilities (OPWDD)
Additional Information
- NYSDOH and NYSDFS: 2023 Telehealth Report
- Telehealth Utilization in NYS Medicaid (PDF)
- General Overview of the Expansion of Medicaid Coverage of Telehealth - Archived
- Specific Guidance for Federally Qualified Health Centers - Archived
Contact
- Telehealth coverage and policy questions may be directed to the Office of Health Insurance Programs (OHIP) Division of Program Development and Management at (518) 473-2160 or emailed to Telehealth.Policy@health.ny.gov
- FFS general coverage and policy questions may be directed to the Office of Health Insurance Programs (OHIP) Division of Program Development and Management at (518) 473-2160 or emailed to FFSMedicaidPolicy@health.ny.gov
- MMC general coverage questions may directed to the Division of Healthcare Planning Contracting and Oversight (DHPCO) at covques@health.ny.gov or (518) 473-1134.
- Questions regarding MMC reimbursement and/or documentation requirements should be directed to the enrollee's MMC plan.
Follow Us