Transitioning Office of Mental Health
- Slides also available in Portable Document Format (PDF, 1.7MB)

Transitioning Office of Mental Health Children´s Targeted Case Management (TCM) Program to Health Homes
Webinar #1: Overview of Health Homes and Important Transition Information
June 8, 2015
2:00 PM–3:30 PM
Introductions
- Lana I. Earle, Deputy Director, Division of Program Development and Management, Office of Health Insurance Programs, NYS DOH
- Angela Keller, LMSW, Director, Bureau of Children´s Program Design, Policy & Planning Division of Managed Care, OMH
- Michelle Wagner, Division of Integrated Community Services for Children and Families, OMH
Today´s Discussion
- Overview of the Health Home program and how its requirements are being tailored to better serve children
- Health Home standards and requirements for providing care management
- Next Steps for OMH TCM providers
What is a Health Home?
- Health Home is an optional State Plan benefit authorized under Section 2703 of the Affordable Care Act (ACA) to coordinate care for people with Medicaid who have chronic conditions
- Health Home is a Care Management model that provides:
- Enhanced care coordination and integration of primary, acute, behavioral health (mental health and substance abuse) services, and
- Linkages to community services and supports, housing, social services, and family services for persons with chronic conditions
- In New York State, the Health Home model has been a central feature of the Medicaid Redesign Team (MRT) initiatives to integrate behavioral and physical health and social supports, transition the behavioral health benefit to managed care, provide ´Care Management for All,´ and reduce avoidable hospitalizations under the Delivery System Reform Incentive Payment (DSRIP) Program through the creation of Performing Provider Systems
New York´s Health Home Model
- The New York State Health Home Model was designed through by a collaborative process that included multiple State agencies (DOH, OMH, OASAS and NYCDOHMH). For the children´s model, OCFS is also involved.
- In New York State, Health Homes are led by one provider which is required to create a comprehensive network of providers to help members connect with:
- Existing care management providers and targeted case management (TCM) programs that now operate under the Health Home program
- One or more hospital systems;
- Multiple ambulatory care sites that include both physical and behavioral health;
- Community and social supports, e.g., housing and vocational services; and
- Managed care plans.
- Health Homes were implemented across the State beginning January 2012
- Currently, 33 Health Homes have been designated by the State, primarily serving adults
- Not all of these Health Homes will be designated to serve Children and there may be newly designated Health Homes that will just serve children
Health Homes Provide an Important Opportunity to Improve Health and Outcomes for Children with Chronic Conditions and Behavioral Health Needs
- Health Homes provide person–centered comprehensive care management to individuals with chronic conditions
- The care management expertise of OMH TCM agencies and other care managers that serve children will play an important role in the Health Home model for children
- Health Homes will expand the availability of care management from the limited population of children served by ´waivers´ (e.g., OMH SED Waiver) and targeted case management programs (˜ 12,000 children) to potentially 150,000 to 200,000 children across the Medicaid population that have unique needs and may qualify and be appropriate for Health Home
- Health Homes provide an opportunity to establish critical linkages and help break down silos of care by linking systems and programs (education, child welfare, early intervention) to comprehensive care planning
Principles for Serving Children in Health Homes and Managed Care
- Ensure managed care and care coordination networks provide comprehensive, integrated physical and behavioral health care that recognizes the unique needs of children and their families
- Provide care coordination and planning that is family–and–youth driven, supports a system of care that builds upon the strengths of the child and family
- Ensure managed care staff and systems care coordinators are trained in working with families and children with unique, complex health needs
- Ensure continuity of care and comprehensive transitional care from service to service (education, foster care, juvenile justice, child to adult)
- Incorporate a child/family specific assent/consent process that recognizes the legal right of a child to seek specific care without parental/guardian consent
- Track clinical and functional outcomes using standardized pediatric tools that are validated for the screening and assessing of children
- Adopt child–specific and nationally recognized measures to monitor quality and outcomes
- Ensure smooth transition from current care management models to Health Home, including transition plan for care management payments
New York State Health Home Model for Children
Managed Care Organizations (MCOs)
Health Home
Administrative Services, Network Management, HIT Support/Data Exchange
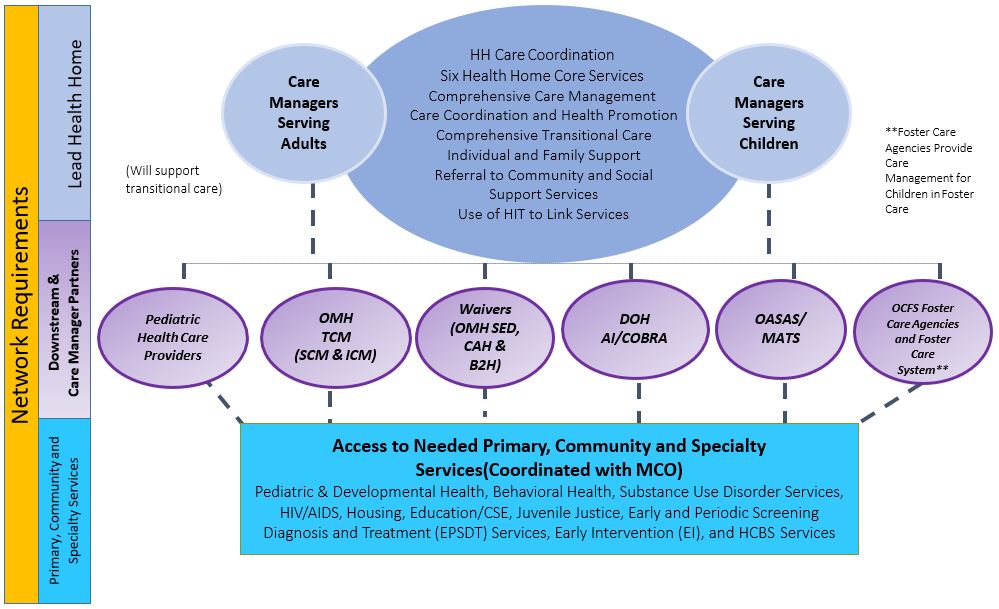
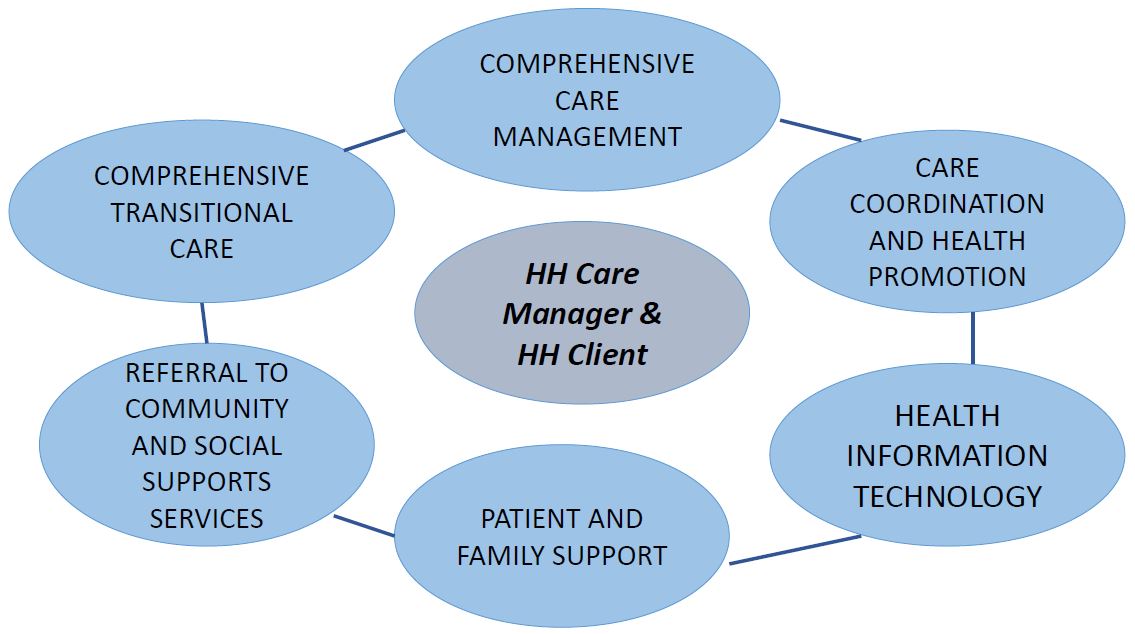
Health Homes Provide Six Core Care Management Functions
Health Home care management is "whole–person" and "person–centered" and integrates a care philosophy that includes both physical/behavioral care and family and social supports
Six Core Services of Health Home
Health Home must have planning and policies and procedures in place to ensure care managers create, document, execute and update an individualized, patient centered plan of care for each individual
- Comprehensive Care Management
- A comprehensive health assessment that identifies medical, mental health, chemical dependency and social service needs is developed.
- Care Coordination and Health Promotion
- The Health Home provider is accountable for engaging and retaining Health Home enrollees in care; coordinating and arranging for the provision of services; supporting adherence to treatment recommendations; and monitoring and evaluating a patient´s needs, including prevention, wellness, medical, specialist and behavioral health treatment, care transitions, and social and community services where appropriate through the creation of an individual plan of care.
- Comprehensive Transitional Care
- The Health Home provider has a system in place with hospitals and residential/rehabilitation facilities in their network to provide the Health Home prompt notification of an individual´s admission and/or discharge to/from an emergency room, inpatient, or residential/rehabilitation setting.
- Patient and Family Support
- Patient´s individualized plan of care reflects patient and family or caregiver preferences, education and support for self–management, self–help recovery, and other resources as appropriate.
- Referral to Community Supports
- The Health Home provider identifies available community–based resources and actively manages appropriate referrals, access, engagement, follow–up and coordination of services.
- Use of Health Information Technology (HIT) to Link Services
- Health Home providers will make use of available HIT and access data through the regional health information organization/qualified entities to conduct these processes as feasible, to comply with the initial standards cited in items 6a.–6d for implementation of Health Homes. In order to be approved as Health Home provider, applicants must provide a plan to achieve the final standards cited in items 6e.–6i. within eighteen (18) months of program initiation.
Tailoring Health Homes to Serve Children ~ Collaborative Effort of State Agency Partners and Stakeholders
State Agency Partners
- Office of Mental Health (OMH)
- Office of Alcoholism and Substance Abuse Services (OASAS)
- Office of Children and Family Services (OCFS)
- Department of Health (DOH) including Office of Health Insurance Programs, Center for Health– Division of Family Health, AIDS Institute
- New York State Education Department
Stakeholders
- Health Homes, Managed Care Plans and Care Managers
- Trade Associations
- Provider Organizations
- Advocates
- Local Government Partners (LDSS, LGU, SPOA, NYCDOHMH)
Tailoring New York´s Health Home Model to Better Serve Children
- Health Home initially implemented by enrolling adults and established the Health Home infrastructure
- In recognition of the differences between children and adults, the model was tailored to accommodate the needs of children by:
- ✓ Tailoring the eligibility criteria
- ✓ Expanding the networks of existing Health Homes and potentially creating new children´s Health Homes to ensure Health Homes and their provider networks accommodate the special needs of children including:
- Care managers with expertise in serving children – including OMH TCM Programs (October 2015) and Children´s Waiver Programs (January 2017)
- Networks include providers that meet special needs of children with chronic and complex conditions (pediatricians, children´s specialty providers)
- Linkages to systems and programs that care for or interface with children (education, child welfare, juvenile justice)
- ✓ Tailoring the delivery of the six core Health Home services to the needs of children and their families
Health Home Eligibility Criteria – Current and Proposed
(Modifications for Children in Bold)
Person must be enrolled in Medicaid and have:
- Two or more chronic conditions or
- One single qualifying condition of
- ✓ HIV/AIDS or
- ✓ Serious Mental Illness (SMI) / Serious Emotional Disturbance (SED)
- Trauma at risk for another condition (Requires Centers for Medicare and Medicaid Services (CMS) Approval)
Visit here for more information.
Chronic Conditions (Modifications for children in bold)
- ✓ Alcohol and Substance Abuse
- ✓ Mental Health Condition
- ✓ Cardiovascular Disease (e.g., Hypertension)
- ✓ Metabolic Disease (e.g., Diabetes)
- ✓ Respiratory Disease (e.g., Asthma)
- ✓ Obesity BMI >25 (BMI at or above 25 for adults or at or above the 85th percentile for children of the same age and sex)
- ✓ Other
Health Home Appropriateness Criteria
Persons meeting criteria must be appropriate for Heath Homes Care Management:
- ✓ At risk for adverse event, e.g., death, disability, inpatient or nursing home admission, mandated preventive services or out of home placement
- ✓ Inadequate social/family/housing support; or serious disruptions in family relationships
- ✓ Inadequate connectivity with healthcare system
- ✓ Non–adherence to treatments or difficulty managing medications
- ✓ Recent release from incarceration, placement, detention or psychiatric hospitalization
- ✓ Deficits in activities of daily living
- ✓ Learning or cognition issues
- ✓ Concurrent eligibility or enrollment of a child and the family/caregiver in Health Home
Tailoring Health Homes to Better Serve Children
- Health Home eligibility criteria must be condition based (i.e., not population based)
- To achieve the goal of ensuring eligibility condition–based criteria captures high needs children´s populations, including Medically Fragile Children with complex health issues, children in foster care, children with Serious Emotional Disturbance (children complement to adult SMI), children enrolled in ´Waiver´ programs and other case management programs the State is proposing to Centers for Medicare and Medicaid Services (CMS) to modify Health Home eligibility criteria to include trauma
Proposed Trauma Definition
- Definition of Trauma: Exposure to a single severely distressing event, or multiple or chronic or prolonged traumatic events as a child or adolescent, which is often invasive and interpersonal in nature. Trauma includes complex trauma exposure which involves the simultaneous or sequential occurrence of child maltreatment, including psychological maltreatment, neglect, exposure to violence and physical and sexual abuse.
- A child or adolescent who has experienced trauma would be defined to be at risk for another chronic condition if they have one or more functional limitations that interferes with their ability to function in family, school, or community activities, or they have been placed outside the home.
- ✓ Functional limitations are defined as difficulties that substantially interfere with or limit the child in achieving or maintaining developmentally appropriate social, behavioral, cognitive, communicative, or adaptive skills, or for a child who experienced trauma due to child maltreatment, a functional limitation is defined as a serious disruption in family relationships necessary for normal childhood growth and development
Health Home Application to Serve Children Health Home Designation Process for Children
- Application for existing Health Homes and other providers interested in becoming lead Health Homes to serve children was developed in consultation with State Agency Partners and stakeholders
- Final Application was released on November 3, 2014, Applications were due March 2, 2015
- State Agency Partners reviewing Final Applications – Designations expected to be announced next week
- Final Application includes significant amount of detail regarding the structure and requirements for Health Homes serving children and is an excellent source of information
- List of OMH TCM children´s providers was posted with draft and Final Application
- List of entities that submitted applications has been posted to DOH website
- OMH TCM children´s providers that have not already established relationships with potential Health Homes should immediately begin to do so
| Anticipated Schedule of Activities for Expanding Health Homes to Better Serve Children | Due Date |
|---|---|
| Draft Health Home Application to Serve Children Release | June 30, 2014 –Completed |
| Due Date to Submit Comments on Draft Health Home Application to Serve Children | July 30, 2014 –Completed |
| Due Date to Submit Letter of Interest | July 30, 2014 –Completed |
| Final Health Home Application to Serve Children Released | November 3, 2014 –Completed |
| Due Date to Submit Health Home Application to Serve Children | March 2, 2015 –Completed |
| Review and Approval of Health Home Applications to Serve Children by the State | March 2, 2015 to June 15, 2015 Review Process Underway |
| HH and Network Partner Readiness Activities | June 15, 2015 to September 30,2015 |
| State Webinars, Training and Other Readiness Activities | Through September 30, 2015 |
| Begin Phasing–in the Enrollment of Children in Health Homes | October 2015 |
| Children´s Behavioral Health Services and other Children´s Populations Transition to Managed Care | January 2017 (NYC/LI) July 2017(ROS) |
Other Health Home Standards and Requirements
- Health Home for children case load sizes
- Case load sizes are not mandated but have been reflected in the rate build for the per member per month (PMPM) Health Home rates for children – the goal is to keep case load ratios as low as practical and to provide Health Homes and care managers flexibility in assigning children with various levels of needs/acuities
- Case load sizes in the rate build – High 1:12, Medium 1:20 and Low 1:40
- Care Managers serving children with high acuity will be required to keep their case load mix predominantly to children in high acuity level (1:12)
- Health Home services must meet the standards for delivery defined by the six core services
- At least one Health Home service must be delivered every month in order to bill the Per Member Per Month rate
- Care managers serving children with medium and high acuity will be required to provide at least two Health Home services per month, one of which must be a face–to–face encounter with the child
- Qualifications of Health Home Care Managers Serving Children
- Qualifications for care managers serving low and medium acuity is left up to the discretion of the Health Home to provide flexibility to make operational decisions that best reflect the mix of children served by individual Health Homes
- Qualifications for care managers serving children with high acuity:
- Bachelors of Arts or Science, 2 years of relevant experience, or
- A licensed Registered Nurse with two years of relevant experience, or
- A Masters with one year of relevant experience
Questions?
OMH Community TCM Transition to Health Home Care Management October 1, 2015
- OMH TCM children´s providers transition to Health Home as downstream care management providers of Health Homes
- In addition to providing care management to OMH TCM children in Health Home, OMH TCM providers may engage in agreements with designated Health Homes to serve other children eligible for Health Homes
- As Health Home care managers, OMH TCM providers will be required to deliver the six core Health Home services required by the program and tailored for children
- TCM regulations are no longer applicable to OMH TCM providers that transition to the Health Home program and bill Health Home rate codes
- Flex Funds – will continue to be granted for legacy slots via State Aid funding
- State Aid funding will continue to support non–Medicaid eligible children
Today – June 2015
I am an OMH designated TCM Provider.
My agency hires ICMs, SCMs and/or BCMs to serve children.
Case managers serve children eligible for TCM Services as per SPOA and other referrals.
My agency might also provide other Medicaid and community services.
My agency is beginning to get to know the lead Health Homes in my area that will be designated serve children
Principles in my agency have read the Health Home application for Serving Children.
Agency staff is listening to relevant Health Home Webinars.
My agency is deciding whether to serve other Health Home eligible children, beyond our current TCM service capacity.
My agency will enter into a subcontract with a Lead Health Home designated to serve children by October 2015.
June– September 2015
My agency will continue to provide TCM services to children who are eligible in the manner it has done for many years.
My supervisor and I will continue to be trained in preparation for the transition to Health Home.
I will ask questions and participate proactively in solution focused planning in my agency.
Future – October 2015
We are a community based agency.
We used to be a designated TCM program.
The federal authority to operate a TCM Program is being phased out.
We are now a designated Health Home downstream provider of care management services.
We are under subcontract with one or more of the area´s lead Health Homes.
My agency´s case managers are now called Health Home Care Managers and operate under Health Home guidelines.
I no longer have to have 4 contacts a month with each client. I do not have to track my billing by 15 minute increments.
My agency has converted children enrolled in the TCM Program into Health Homes.
Health Home Rates for Children (under 21)
| Per Member Per Month HH Care Management Rates | ||
|---|---|---|
| Acuity (CANS Algorithm) Case Load Ratios Not Mandated | Upstate | Downstate |
| HFW (1:10 – Pilot Demo) | $900 | 958 |
| High (1:12) | 750 | 799 |
| Medium (1:20) | 450 | 479 |
| Low (1:40) | 225 | 240 |
| Outreach | 135 | 135 |
| CANS–NY Assessment | 185 | 185 |
TCM Current Rates and Slot Authority
Upstate Range now $349 to $664 per month
Downstate Range now $419 to $700 per month
Slots authorized range from 12 to 352
State Aid funding for non–Medicaid children
Role of SPOA with TCM Legacy Programs
Until legacy slots are phased out, SPOA will continue to manage and triage OMH HHCM legacy slots to be filled with the most needy children
Determined by SPOA to need care coordination services, a direct referral to the TCM provider is made
The TCM provider process the referral into the Medicaid Analytic Performance Portal (MAPP) as per protocols
OMH Guidance document currently being drafted
If Legacy Slots are full SPOA will make referral through MAPP for HHCM
Use of the Child and Adolescent Needs and Strengths Assessment of New York (CANS–NY)
The State is working to modify and test the CANS–NY to:
- Include modules specific to the 0–5 and 6–21 age groups
- Include a module related to sexuality and sexual orientation
- Include modules relating to Activities of Daily Living and Instruction on Activities of Daily Living to be in compliance with the Balancing Incentive Program;
- Make enhancements to better assess medically fragile children
- Modify the tool to determine functional limitations as provided by SED and Trauma eligibility criteria
- Develop an algorithm that will determine acuity tier (i.e., High, Medium, Low) for children´s Health Home rates
Questions?
Future Webinars to Facilitate TCM Transition to Health Home
- OMH TCM Webinar #2 will provide information on Health Home Legacy Rates, Medicaid Analytics Performance Portal (MAPP), Enrollment of TCM Children into Health Homes, other Agency Preparedness & Administrative Processes
- DOH Statewide Webinars regarding the implementation of Health Homes for Children
- Some Webinars have been conducted and are recorded and
- available now – Health Home for Children Design and Implementation Updates–April 29 Webinar, Consent, Assignment Process, Health Information Technology)
- Other Webinars and Updates will be scheduled:
- CANS–NY Training, Medicaid Analytics Performance Portal
- Consent for Health Home enrollment and information sharing, Medicaid Analytics Performance Portal, Health Home Rates for Children, CANS–NY training)
- OMH Office Hours Call to review today´s highlights and allow more informal dialogue and clarification.
Next Steps for TCM Children´s Providers
- Reach out to adult TCM providers that have transitioned to Health Home for learning and sharing.
- Establish Relationships with Health Homes and entities that will be designated to serve children
- Actively participate in webinars, and review information
- Consider how you can maximize your expertise and the opportunities provided by the new Health Home model
- Consider serving a broader children´s population than you currently serve
- Completion of CANS training and certification for all program staff
Resources for Updates
- DOH Health Homes and Children Website
- DOH Medicaid Health Homes Listserv
- OMH TCM Listserv
Email Michelle Wagner– Michelle.Wagner@omh.ny.gov
Contact Information
OMH Community TCM for Children
Michelle Wagner: Michelle.Wagner@omh.ny.gov
Phone– 518–474–8394
DOH Health Home for Children
Alexis Harrington
Phone– 518–473–5569
Email– hhsc@health.ny.gov