Archives

Tailoring Health Home Model to Serve Children: Design and Implementation Updates
- Slides also available in Portable Document Format (PDF)
April 29, 2015
Introductions
Children´s Leadership Team
- Donna Bradbury Associate Commissioner, Division Of Integrated Community Services For Children & Families, NYS Office of Mental Health (OMH)
- Lana I. Earle, Deputy Director, Division of Program Development and Management, Office of Health Insurance Programs, NYS Department of Health (DOH)
- Steve Hanson, Associate Commissioner, NYS Office of Alcoholism and Substance Abuse Services (OASAS)
- Laura Velez, Deputy Commissioner, Child Welfare & Community Services, NYS Office of Children and Family Services (OCFS)
Agenda
Health Home Schedule and Managed Care Transitions
| Anticipated Schedule of Activities for Expanding Health Homes to Better Serve Children | Due Date |
|---|---|
| Draft Health Home Application to Serve Children Release | June 30, 2014 –Completed |
| Due Date to Submit Comments on Draft Health Home Application to Serve Children | July 30, 2014 –Completed |
| Due Date to Submit Letter of Interest | July 30, 2014 –Completed |
| Final Health Home Application to Serve Children Released | November 3, 2014 –Completed |
| Due Date to Submit Health Home Application to Serve Children | March 2, 2015 –Completed |
| Review and Approval of Health Home Applications to Serve Children by the State | March 2, 2015 to June 15, 2015 Review Process Underway |
| HH and Network Partner Readiness Activities | June 15, 2015 to September 30,2015 |
| State Webinars, Training and Other Readiness Activities | Through September 30, 2015 |
| Begin Phasing–in the Enrollment of Children in Health Homes | October 2015 |
| Children´s Behavioral Health Services and other Children´s Populations Transition to Managed Care | January 2017 (NYC/LI) July 2017 (ROS) |
Health Homes and Behavioral Health Transition Timeline
| Date | Health Home Enrollment | Expanded Medicaid Services for Development of Health Home Plan of Care |
|---|---|---|
| October 1, 2015 | Enrollment of Children in Health Home begins Health Home eligible children and OMH Targeted Case Management (TCM) (Early Intervention (EI) children when CMS EI SPA approved) | Expanded State Plan Services (See Appendix) – Require SPA approval, State Partners moving forward to make available asap |
| January 1, 2017 | NYC and Long Island Behavioral Health Transition to Managed Care NYC and Long Island Foster Care population to Managed Care NYC Waiver Providers* [six 1915c children´s Waivers (OMH SED, DOH Care at Home (CAH) I/II, OCFS Bridges to Health (B2H) transition to Health Home] | Home and Community Based Services (HCBS) (see Appendix) in NYC and Long Island, most Health Home eligible children will likely qualify |
| July 1, 2017 | Rest of State (ROS) Behavioral Health Transition to Managed Care ROS Foster Care population to Managed Care ROS Waiver Providers* [six 1915c children´s Waivers (OMH SED, DOH CAH I/II, OCFS B2H) transition to Health Home] | HCBS Services (See Appendix) in ROS Available, most Health Home eligible children will likely qualify |
| OMH TCM care managers and all Waiver providers should work with Health Homes now to establish relationships. OMH TCM care managers and Waiver providers will provide the care management for their TCM and Waiver children that transition to Health Home. Waiver providers should bring their care management expertise to Health Homes now . Waiver providers can provide Health Home Care Management to children not enrolled in waiver program. | ||
Status of Health Home Applications to Serve Children
Update on Health Home Applications to Serve Children
- Applications were due March 2, 2015
- The State received 22 Applications
- List has been posted to web site
- List includes organization name, proposed counties of service, primary contact information and status (all under review)
- To assist the team in reviewing Applications and to facilitate the design, build and modifications of Medicaid systems (i.e., Medicaid Analytics Performance Portal (MAPP), Medicaid provider enrollment) the State has requested:
- Each Applicant to identify which providers it intends to contract with to provide care management services
- This information is due to the Department on or before Monday, May 4, 2015
- As indicated in the Application, Health Homes should be planning to contract with care managers that have expertise in providing care management to the broad array of children that will be eligible for Health Homes (foster care, medically complex)
- Health Homes are required to contract with Volunteer Foster Care Agency to be the downstream care manager for children enrolled in Health Homes
- Voluntary foster care agencies provide the State information on which counties they serve and if they intend to be Health Home care managers or to delegate this role to another agency or Health Home
- Each Applicant to identify which providers it intends to contract with to provide care management services
- Multi–state agency team review process underway (DOH, OMH, OASAS, OCFS, NYC DOHMH)
- The conclusion of review process will result in the issuance of a status letter, which may either:
- Designate the entity to operate as Health Home Serving Children
- Contingently designate the entity, (i.e., approval contingent upon the satisfaction and documentation of the completion of certain state team requirements)
- Reject the application as not meeting minimum standards (including comprehensiveness of network) for operating a Health Home serving children.
Resources for Children´s Health Homes
Resources for Children´s Health Home
Health Home Development Funds (HHDFs)
Rate add on
applied to claims
with the following
dates of paymentRate
Add–on
Payment
DateAmount of
Payment
Authorized
Under the SPA8/1/14 to 2/28/15 March 2015 $80 million 3/1/15 to 5/31/15 June 2015 $22.2 million 6/1/15 to 8/31/15 September 2015 $22.2 million 9/1/15 to 11/30/15 December 2015 $22.3 million 12/1/15 to 2/29/16 March 2016 $10.9 million 3/1/16 to 5/31/16 June 2016 $10.9 million 6/1/16 to 8/31/16 September 2016 $10.9 million 9/1/16 to 11/30/16 December 2016 $11.2 million
- On March 10, 2015 the Centers for Medicare and Medicaid (CMS) approved the State Plan Amendment (SPA) to implement the $190.6 million of Health Home Development Funds authorized in the MRT 1115 Waiver amendment.
- As authorized by the Special Terms and Conditions (STCs) of the Waiver, the Funds will be paid through a rate add on to the Health Home PMPM and will apply to claims for outreach and engagement which have a corresponding segment in
- Payments began in March 2015 and will be paid quarterly through 2016
- Must be used for one or more of the following four authorized purposes:
- ✓ Member Engagement and Health Home Promotion
- ✓ Workforce Training and Retraining
- ✓ Clinical Connectivity and Health Information Technology (HIT) Implementation
- ✓ Joint Governance Technical Assistance
- All HHDF must advance the directives and requirements of the Health Home Program.
- Health Homes must consult with their downstream network partners (downstream partners may include care management agencies and providers of both health and administrative services) to identify appropriate uses of HHDF
- Health Homes must submit a preliminary report and semi–annual reports using forms provided by the Department
- Enacted Budget includes:
- $45 million in 2015–16 and $90 million in 2016–17 for the enrollment of children in Health Homes (i.e., PMPM costs)
- Technical amendment to provide a total of $20 million in Managed Care and Health Home Readiness resources to Foster Care agencies, including Health Home training for Volunteer Foster Care providers
Update on State Plan Amendments (SPAs)
Update/Status of Discussions with CMS and State Plan Approval (SPA) Submission Process
- In September 2014, the State had initial discussions with CMS and submitted an informal, draft Health Home SPA for children
- In November 2014, the State discussed Health Home model for children with Substance Abuse and Mental Health Services Administration (SAMHSA) (a requirement for submitting Health Home SPAs)
- Discussions to date with CMS and SAMHSA have been positive and supportive
- CMS requested the State sequence the submission of Health Home SPA´s, i.e., formally submit the SPA to tailor Health Homes for children after the approval of the Health Home Development SPA
- The HH Development Funds SPA was submitted in the Fall of 2014 and approved on March 10, 2015
- State formally submitted the Health Home Children´s SPA on April 28, 2015
- The SPA includes the following amendments:
- ✓ Amends the Health Home eligibility criteria to:
- Include trauma and at risk for another condition
- Amend the BMI > 25 to BMI at or above 25 for adults and to include comparable definition for children of BMI at or above the 85 percentile for children
- ✓ Reflects the use of the CANS–NY assessment (as opposed to CRGs) to determine level of acuity in the Per Member Per Month Rate structure
- ✓ Reflects a referral (rather than list assignment process) for making Health Home assignments
- ✓ Converts OMH TCM children´s program to Health Home and establishes legacy rates for two year period (October 1, 2015 – October 1, 2017)
- ✓ Amends the Health Home eligibility criteria to:
Children Eligible for Early Intervention Program and Health Home
- Some Medicaid children who meet the Early Intervention criteria will also meet Health Home eligibility criteria and be appropriate for Health Home
- Child would benefit from a care management plan that goes beyond the management of Early Intervention Services
- State cannot make duplicate payments for care management (i.e., Health Home care management PMPM and Early Intervention service coordination payment)
- Maximize the expertise of the EI service coordinator and HH care managers by having the EI initial service coordinator continue to facilitate initial enrollment and the Health Home care manager provide ongoing care management, including the integration of EI services in the child´s comprehensive care plan
- Approach would require:
- CMS Approval – State team has drafted Early Intervention SPA to authorize Health Home care manager to fulfill the requirements of the on–going service coordinator
- State plans to submit the SPA by end of May and schedule meeting with CMS to discuss general approach
- Clear, documented guidance regarding the roles of the EI initial service coordinator and the Health Home care manager to allow the EI initial service coordinator to bill for its role when a child is already enrolled in Health Home and is referred for EI services
- Health Home care managers will be required to ensure EI program requirements are met
- Training on the roles and responsibilities of EI service coordinator and HH Care Management, including procedures for transitioning from initial EI coordination to HH Care Management, EI program requirements, HH program requirements will be provided
- CMS Approval – State team has drafted Early Intervention SPA to authorize Health Home care manager to fulfill the requirements of the on–going service coordinator
- Timing of enrollment of Early Intervention children eligible for Health Home will depend on CMS approval and the completion of training
Definition of Serious Emotional Disturbance
Serious Emotional Disturbance Eligibility Criteria for Health Homes
Definition of Serious Emotional Disturbance
- In the process of reviewing the Draft Health Home Application to Serve Children, stakeholders requested the State clarify how Serious Emotional Disturbance (SED) will be defined for Health Home eligibility. The definition has been clarified to reference Diagnostic and Statistical Manual of Mental Disorders (DSM) categories which would be an SED for Health Home eligibility
- SED is a single qualifying chronic condition for Health Home and is defined as a child or adolescent (under the age of 21) that has a designated mental illness diagnosis in the following (see next page) DSM categories* as defined by the most recent version of the DSM of Mental Disorders AND has experienced the following (see next page) functional limitations due to emotional disturbance over the past 12 months (from the date of assessment) on a continuous or intermittent basis
SED Eligibility Criteria for Health Homes – Qualifying DSM Categories
| SED Definition for Health Home – DSM Qualifying Mental Health Categories* |
|---|
|
| Functional Limitations Requirements for SED Definition of Health Home |
|---|
To meet definition of SED for Health Home the child must have experienced the following functional limitations due to emotional disturbance over the past 12 months (from the date of assessment) on a continuous or intermittent basis
|
*Any diagnosis in these categories can be used when evaluating a child for SED. However, any diagnosis that is secondary to another medical condition is excluded.
Children with Developmental Disabilities
- Children in Health Homes that have a developmental delay diagnosis and one other Health Home chronic condition or a single qualifying Health Home chronic condition and who are not currently receiving services from the Office for People with Developmental Disabilities (OPWDD) may be enrolled in Health Home
- Children in the Care at Home III, IV, and VI Waivers will not be included in the waivers that are transitioned to Health Home in 2017 (i.e., only OMH SED, DOH CAH I/II, OCFS B2H)
Estimates of Children Potentially Eligible for Health Home
Estimated Number of Children Potentially Eligible for Health Homes
- The State has been working to use the proposed expanded eligibility criteria for Health Homes, Medicaid claims data, clinical risk groups (CRGs), OMH, and OCFS data for Foster Care to develop a representative estimate of the number of children that are potentially eligible for Health Home.
- The estimated, potentially eligible population is:
- ✓ Based upon 2013 data from sources identified above
- ✓ Does not "screen" for Health Home appropriateness criteria
- Not everyone on the list that may meet Health Home eligibility criteria is "appropriate" for Health Home (needs the intensive level of care management provided by Health Homes). See Appendix for Health Home eligibility and appropriateness criteria.
- ✓ Is not intended to serve as an assignment roster for the purposes of enrolling children in Health Home (as discussed later, assignments for Health Home will be made through referral process). Note: the list will be used as a mechanism to cross reference actual Health Home assignments to estimated eligible population as a "point of information"
Estimated Number of Children Potentially Eligible for Health Homes by Region
| Calendar Year 2013 Data – Children Potentially Eligible for Health Home | |||||
| Region | DD | LTC | MHSA | OTHER | Grand Total |
|---|---|---|---|---|---|
| Non–Waiver Children | |||||
| NYC | 5,999 | 712 | 39,300 | 34,541 | 80,552 |
| ROS | 2,267 | 352 | 52,519 | 16,267 | 71,405 |
| No County Code | 252 | 79 | 1,989 | 1,414 | 3,734 |
| sub–total | 8,518 | 1,143 | 93,808 | 52,222 | 155,691 |
| Waiver and EI Children | |||||
| NYC | 1,361 | 488 | 2,995 | 4,998 | 9,842 |
| ROS | 869 | 510 | 3,174 | 3,472 | 8,025 |
| No County Code | 31 | 22 | 238 | 134 | 425 |
| sub–total | 2,261 | 1,020 | 6,407 | 8,604 | 18,292 |
| Total | 10,779 | 2,163 | 100,215 | 60,826 | 173,983 |
- There are almost 174,000 children potentially eligible for Health Home
- 53% NYC, 47% ROS (excluding no county indicator) DOH will post a county breakdown along with this PPT to DOH HH Website
- The DD category excludes OPWDD individuals that are in CAH III, IV, and VI, OPWDD HCBS Waivers or receiving OPWDD service coordination
- 75% of HH eligible children are enrolled in Plan. The FFS members are predominantly children in Foster Care who will move to Managed Care in 2017
Estimated Number Children Potentially Eligible for Health Homes by Health Status,
Excluding Waiver and EI Children
| Calendar Year 2013 Data – Children Potentially Eligible for Health Home Excluding Waiver and EI Children | |||||
|---|---|---|---|---|---|
| Base Health Status | DD | LTC | MHSA | OTHER | Total |
| Pairs Chronic | 5,474 | 499 | 30,025 | 30,263 | 66,261 |
| Minor Conditions | 597 | 37 | 27,759 | 540 | 28,933 |
| Single SMI/SED | 600 | 61 | 25,076 | 25,737 | |
| Acute | 250 | 26 | 895 | 17,433 | 18,604 |
| Single Chronic | 489 | 34 | 8,612 | 1,237 | 10,372 |
| Triples Chronic | 1,018 | 359 | 1,057 | 1,477 | 3,911 |
| HIV/AIDS | 87 | 126 | 384 | 1,253 | 1,850 |
| Catastrophic | 3 | 16 | 19 | ||
| Malignancies | 1 | 3 | 4 | ||
| Total non–Waiver Children | 8,518 | 1,143 | 93,808 | 52,222 | 155,691 |
- About 63% of the children are in Pairs, SED, Triple, and HIV status
- 60% fall in the MHSA Category
Estimated Number of Waiver and EI Children Potentially Eligible for Health Homes
| Calendar Year 2013 Data – Waiver and EI Children Potentially Eligible for Health Home | |||||
|---|---|---|---|---|---|
| Base Health Status | DD | LTC | MHSA | OTHER | Total |
| Pairs Chronic | 1,200 | 538 | 2,534 | 5,838 | 10,110 |
| Single Chronic | 347 | 122 | 939 | 773 | 2,181 |
| Single SMI/SED | 105 | 38 | 1,908 | 2,051 | |
| Acute | 118 | 20 | 57 | 1,315 | 1,510 |
| Triples Chronic | 416 | 255 | 250 | 462 | 1,383 |
| Minor Conditions | 65 | 23 | 698 | 172 | 958 |
| HIV/AIDS | 6 | 15 | 21 | 23 | 65 |
| Catastrophic | 4 | 9 | 13 | 26 | |
| Malignancies | 8 | 8 | |||
| Total Waiver and EI Children | 2,261 | 1,020 | 6,407 | 8,604 | 18,292 |
- 74% of the children are in Pairs, SED, Triple and HIV status
- 35% fall in the MHSA Category
Estimated Number of Potentially Eligible Health Home Children by Population Group
| 2013 Data Population* | DD | LTC | MHSA | OTHER | Total |
|---|---|---|---|---|---|
| Foster Care | 1,262 | 121 | 8,518 | 20,887 | 30,788 |
| SSHSP | 2,388 | 400 | 7,460 | 2,238 | 12,486 |
| Early Intervention | 928 | 395 | 1,317 | 7,420 | 10,060 |
| B2H Waiver | 801 | 30 | 2,685 | 839 | 4,355 |
| OMH HCBS | 105 | 87 | 2,385 | 188 | 2,765 |
| CAH | 405 | 531 | 35 | 245 | 1,216 |
| *Members are not mutually exclusive (i.e., can be in more than one category) | |||||
Integrating High Fidelity Wraparound in Health Home – Pilot
Integrating High Fidelity Wraparound in the Health Home Model
- Wraparound is a planning process that follows a series of prescribed steps to help children and their families realize a life that reflects their hopes and dreams
- The HFW approach to care management is consistent with the goals and structure of the Health Home care management model
- Stakeholders were in general agreement the State should explore incorporating the HFW approach in the Health Home model for a small subset of eligible youth that meet the Health Home eligibility criteria and can benefit from the specialized and intensive care management approach
Health Home High Fidelity Wraparound Pilot
- To test the integration of the HFW approach in the Health Home model, the State will initiate a Health Home, High Fidelity Wraparound pilot
- The pilot is designed to expand and complement the System of Care technical assistance and training activities provided by the New York State Success Initiative, via a multi–year SAMHSA grant.
- The objectives of the proposed pilot are to:
- Inform how a high quality Wraparound care management model can be incorporated into New York´s Health Home model, including criteria for developing and identifying Health Home eligibles with serious behavioral health challenges that could be benefit from the HFW approach
- Assess resources required to implement the HFW
- Identify the effectiveness of using the HFW model within the Health Home model to improving health and well being and meeting the person centered, family and youth driven goals of the care plan
Structure of High Fidelity Wraparound Pilot
- Challenge: Launching a pilot at the same time we launch the enrollment of children in Health Homes
- Structure of the pilot is under development, preliminary elements include:
- Training HFW staff about the Health Home for Children Care Management model and requirements; training Health Home staff in wraparound philosophy, facilitation and practice; and developing approaches for integrating HFW in Health Home
- Using SAMSHA grant funds to support: training and mentoring in the HFW and Health Home model; payment of the rate differential between the Health Home Per Member, Per Month Rates for HFW and High Acuity Rates (Rate structure discussion to follow) and flexible services dollars
- Pilot funding may only be used outside of New York City and Long Island
- Participation by Health Homes will be optional, but a pilot site must be Health Home designated to serve children
CANS–NY Assessment Tool
CANS–NY and Health Home (CANS–NY Child and Adolescent Needs and Strengths Assessment–NY)
- The CANS–NY assessment (as modified for New York) will be used:
- ✓ To assist in the development of the person centered care plan
- ✓ Determine acuity for Health Home rate tiers
- ✓ Provide information that may help determine if children meet the Health Home eligibility functional criteria for Serious Emotional Disturbance (SED) and Trauma
- ✓ CANS–NY by itself will not determine Health Home eligibility
- CANS will also be used to determine the eligibility for Home and Community Based Services (HCBS) that will be made available with the behavioral health and health benefit transitions to Managed Care in 2017
- The CANS–NY assessment tool is:
- A multi–purpose tool to support decision making, including level of care and service planning, to facilitate quality improvement initiatives, and to allow for the monitoring of outcomes of services.
- Developed from a communication perspective so as to facilitate the linkage between the assessment process and the design of individualized service plans including the application of evidence–based practices.
- Provides the care coordinator, the family, and service providers with a common language to use in the development, review, and update of the child´s care plan.
- Designed to give a profile of the current functioning, needs, and strengths of the child and the child´s parent(s) and/or parent substitute.
Modifying CANS–NY for Health Homes
(Child and Adolescent Needs and Strengths Assessment–NY)
- The State Agency Partners, in consultation and under the guidance of Dr. John Lyons, author of the CANS have been working to:
- ✓ Modify the tool to better reflect the population of children that are expected to be eligible for Health Home, resulting in revisions made in 2014–15 which include:
- Broad array of target populations
- Separate tools for 0–5 and 6–21 age groups
- Addition of more modules for the 14 and older youth population (e.g., independent activities of daily living, transition to adulthood)
- Make enhancements to better assess medically fragile children
- Modify the tool to determine functional limitations required to meet the SED and Trauma Health Home eligibility criteria
- ✓ Develop algorithms to determine acuity for assignment to a Health Home per member per month rate tier (i.e., High, Medium, Low) and HCBS eligibility (Level of Care, Level of Need)
- ✓ Modify the tool to better reflect the population of children that are expected to be eligible for Health Home, resulting in revisions made in 2014–15 which include:
CANS–NY Testing Now Underway
- The draft revised tools have been posted to the Department´s website
- The modifications to the CANS–NY are being tested
- Testing began in March 2015 and includes:
- ✓ The following providers, working with newly assessed or currently served children:
- OMH TCM
- OMH Waiver,
- LGU/SPOA
- OCFS Waiver
- CAH I/II Waiver
- OASAS providers
- Providers working with medically fragile children
- ✓ Databases available to Dr. John Lyons will test the NY algorithms for medically fragile and Early Intervention populations in Ontario, Canada and Indiana
- ✓ Existing OCFS and OMH databases
- ✓ The following providers, working with newly assessed or currently served children:
- Chapin Hall of the University of Chicago will be collecting and assisting the State in analyzing and evaluating the test data and algorithms
High Level Overview of Modified CANS–NY and Health Home (Child and Adolescent Needs and Strengths Assessment–NY)
- The modified CANS–NY has a set of needs and strength domains for each tool (0–5 and 6– 21) and a series of modules (completed if necessary based on screening questions for modules)
- Unless otherwise specified, CANS–NY ratings are based on the prior 30 days.
- Care managers will be given 30 days from the date of enrollment to conduct the CANS–NY
- Each item suggests different pathways for service planning
- There are four levels of each item with anchored definitions
- The definitions are designed to translate into the following action levels for either needs or strengths as applicable
- For needs:
- 0 = No evidence
- 1 = Watchful waiting/prevention
- 2 = Action
- 3 = Immediate/Intensive Action
- For strengths:
- 0 = Centerpiece strength
- 1 = Strength that you can use in planning
- 2 = Strength has been identified–must be built
- 3 = No strength identified
| Modified CANS–NY (Age 0–5) Domains, Modules, Items | Modified CANS–NY (Age 6–21) Domains, Modules, Items |
|---|---|
| Caregiver Strengths and Needs (1–27) | Caregiver Strengths and Needs (1–26) |
| Child Strengths (28–36) | Child Strengths (27–39) |
| Child Needs and Functioning (37–44) | Child Needs and Functioning (40–48) |
| Child Development (45–62) | School/Academic Function (49–53) |
| Child Risk Factors (63–69) | Risk Factors and Behaviors (54–64) |
| Child Risk Behaviors (70–73) | Adverse Childhood Experiences (65–81) |
| Adverse Childhood Experiences (74–90) | Modules (Based on Screening Questions) |
| Modules (Based on Screening Questions) | Trauma Symptoms |
| Trauma Symptoms | Behavioral Health |
| Behavioral Health | Substance Use |
| Medical Health | Developmental |
| Preschool/Child Care Functioning | Medical Health |
| Activities of Daily Living | |
| Transition to Adulthood | |
| Independent Activities of Daily Living |
Example: Modified CANS–NY and Health Home
(Child and Adolescent Needs and Strengths Assessment–NY)
| Example of Item from the Child Needs and Function Domain C | |
|---|---|
| Item 43: Decision Making/ Judgment: This item describes the child´s ability to comprehend and anticipate the consequences of decisions; to plan, implement, and monitor a course of action; and to judge and self–regulate behavior according to anticipated outcomes, in a developmentally appropriate manner. | |
| 0 | The child has no evidence of problems with decision making |
| 1 | The child has mild or occasional problems thinking through problems or situations but decisions making abilities do not interfere with functioning |
| 2 | The child has problems thinking through problems or situations and decision making ability interfere with functioning |
| 3 | The child has severe problems with decision making and judgement. Poor decision making places child at risk |
CANS–NY Training
- No cost training and certification will be available on–line starting in July for those who will be using the CANS–NY in Health Homes
- Four two–day in–person training sessions to be held
- On–line training is a prerequisite to the in–person training sessions
- Day 1: All, Day 2: Supervisors, Mentors, Inside Agency Trainers
- Scheduling is underway, more details to come
| Date | Location |
|---|---|
| Last week of July | Albany |
| Second week of August | Rochester |
| Fourth week of August | New York City |
| Fourth week of September | New York City |
CANS–NY Technical Assistance "Institute"
- Request For Proposal (RFP) for release in the Fall
- Awardee(s) to be selected to impact CANS–NY implementation and ongoing operationalization within care management
- State´s goals to provide:
- Intensive technical assistance in consistent use of the CANS–NY tool
- Support and mentoring in actively using the information on the CANS–NY tool for person–centered planning and outcome monitoring
- Supervisory instruction in best practices to support staff in using the CANS– NY tool
Health Home Per Member Per Month Rates for Children
Framework for Development of Health Home Per Member Per Month Rates for Children
- The framework for the development of Per Member Per Month rates for children reflects the following considerations:
- ✓ Tiered Per Member Per Month (PMPM) rate structure (High, Medium, Low) based on acuity of child and the development of an algorithm using the modified CANS–NY for Health Home care management services
- ✓ Case load considerations:
- The goal of keeping case load ratios as low as practicable and to provide Health Homes and care managers flexibility in assigning children with various levels of needs/acuities
- Standards for care management and engagement which require care managers providing services to children:
- With HFW or High acuity (per CANS) to keep their caseload mix predominantly to children of HFW or High acuity level
- Medium and high acuity children to provide two Health Home services per month, one of which must be a face–to–face encounter with the child
- Case load assumptions reflected in the rate build:
- HFW: 1:10
- High: 1:12
- Medium: 1:20
- Low: 1:40
Other than the case load requirements for high acuity children (or HFW) described above, the case loads described above are not "mandated"
- ✓ Upstate and downstate rates
- ✓ Upstate and downstate salary assumptions
- ✓ A rural (upstate) adjustment of 8%
- ✓ Reflect assumptions made in adult High, Medium and Low with clinical and functional rate adjustments
- ✓ Flat PMPM rate for "outreach" activities
- Outreach activities anticipated to be related to educating and informing parents and children, preliminary review of eligibility (re: there is no assignment list for children)
- Outreach PMPM and Care Management PMPM may not both be billed in the same month
- The Care management PMPM (and not the PMPM outreach) should be billed for the month enrollment occurs
- ✓ A fee ($185) for conducting the CANS–NY Assessment
- Fee will be one time at first assessment
- Assessment will be conducted every six months, with appropriate adjustments made to the HML rate that is billed
- ✓ State will issue detailed billing guidance
- ✓ Tiered rate structure would take effect October 2015 and would be the mandated government rates in effect in the first two years of Managed Care (2017 and 2018)
- ✓ Legacy care management payments will be developed for OMH TCM providers that will transition to Health Homes on October 1, 2015
- Legacy payments will remain in effect for two years
- ✓ Legacy care management payments will be also be developed for children´s waiver programs (B2H, CAH I/II, OMH Waiver Programs) when they transition to Health Home in 2017
Health Home Rates for Children (under 21)
| Per Member Per Month HH Care Management Rates for Children under 21 (non–Legacy Providers) (does not include HHDF rate add that may be applicable through November 2016) | ||
|---|---|---|
| Acuity (CANS Algorithm) | Upstate | Downstate |
| HFW | $900 | $958 |
| High | 750 | 799 |
| Medium | 450 | 479 |
| Low | 225 | 240 |
| Outreach | 135 | 135 |
| Assessment | 185 | 185 |
Medicaid Analytics Performance Portal (MAPP) and MAPP modifications for Children
Medicaid Analytics Performance Portal (MAPP)
Long Term Vision (Developed in Phased through 2016)
Medicaid Analytics Performance Portal
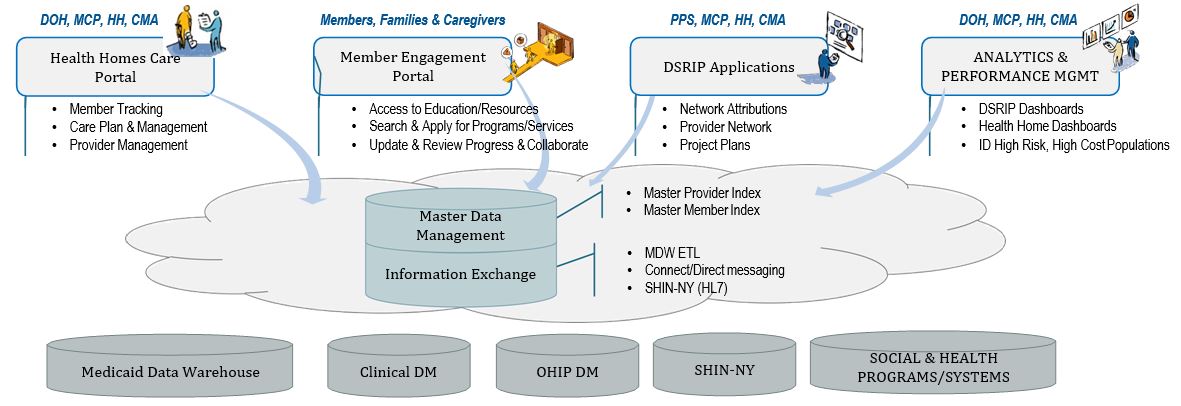
- MAPP supports both Health Homes and DSRIP management and technology needs
- A team of experts (DOH–HH Team, NYSTEC, Salient, IBM, CMA, State UAS, State Agency Partners) have been working to launch the first phase of the MAPP design
- Over several phases of development that will run through 2016, MAPP functionality will grow and expand to be a comprehensive performance management system (data management and analytics, and robust dashboard capabilities)
- MAPP will provide transparent data and tools to Health Home, Plans, care managers, and eventually to consumers and other providers to support providing effective and comprehensive care management to the Health Home population and manage to performance
- At "Go Live" – MAPP will:
- Replace the current Health Home Tracking System, which is accessed now by Health Homes and Plans to track members (e.g., management of Assignment lists and assignments, outreach, enrollment, billing information)
- Provide new and improved functionality
- Extend access to MAPP to downstream care managers
MAPP Functionality at "Go Live"
- Identification of Health Home eligible population
- Assigning eligible individuals to Health Homes
- Outreach of Care Management Agencies (CMA) and Health Homes to potential members
- Enrolling an individual into a Health Home once outreach is complete
- Billing Support (Members´ MCO, HH, and CMA and Diagnosis information)
- Transfer of individuals between Health Homes
- Referrals of potential members (expanded for children)
- Ability to check on member´s connection to Health Home
- Member Batch lookup and export
- Dashboards to assist care managers, Plans and Health Homes to manage performance, identify and evaluate best practices
MAPP Functionality for Children´s Health Homes
- CANS–NY Assessment tool will be integrated into MAPP
- Billing, rate information and CANS–NY algorithms (High, Medium, Low)
- Referral Portal for Children (under 21)
- Community Referral (by LGU/SPOA and LDSS, and eventually others – discussed later) for Assignment
- Assignment and Enrollment by Health Homes, Plans and Care Managers
- Consent Management
- Consent to Refer
- Consent to Enroll
- Consent to Share Information (Protected Services)
CANS–NY Assessment Will be Integrated into MAPP
- Initial implementation of CANS–NY will be in MAPP
- CANS Assessments for ages 0–5 and 6–21 will be conducted using MAPP via HCS
- Access to CANS will be limited to providers that have completed CANS training and certified through the Praed Foundation training program housed through Learner Nation (will be verified by MAPP)
- Billing support functionality will be based on the CANS–NY
- Algorithm to determine acuity from the CANS–NY for High, Medium, Low Health Home rates for children will be automated in MAPP
- The CANS assessment will be accessible through the member record in MAPP to support ongoing care planning
- In future phases, the CANS–NY assessment will be linked to the Care Plan and CANS–NY automation and data will eventually be warehoused on the Uniform Assessment System on DOH´s Health Commerce System and linked to the MAPP
Referral and Health Home Assignments Process for Children will be Housed in MAPP
- The consent of the parent/guardian to make a referral or enroll a child in Health Home makes the use of Department generated Health Home assignment lists for members that are children impractical
- Referrals for assignment and enrollment will be made through the MAPP Referral Portal for Children (members under 21)
- MAPP will accommodate "Community" Referrals for Assignment and Enrollment and "Direct" Referrals for Assignment and Enrollment
- The State is now working with MAPP builders to develop use cases for referral and assignment algorithms – design needs to be complete by middle of May
- Today: Overview of Draft/Preliminary Concepts and Process
- Follow up Webinar to provide more detail on Use Cases scheduled for May 11
Draft Community and Provider Referral and Assignment Process
- "Community" Referrals:
- Made by an entity or provider that is not a Health Home, care manager or a Managed Care Plan
- In the short term, State will pilot the use of the Portal by authorizing LGU/SPOAs and LDSS to access the Community Referral portion of MAPP to make referrals that will identify children for assignment and enrollment to a Health Home
- Over time, the State will expand access to the Community Referral portal by identifying and authorizing other entities that are natural points of contact in the systems of care that impact children to make referrals through the Community Referral portal (LGU/SPOA, LDSS, School Districts, county probation departments, pediatricians, emergency rooms, Early Intervention initial care coordinators)
- In addition, towards the end of this year, the State intends to expand the Community Referral portal to provide a second avenue for making referrals for adults – will help facilitate referrals from ER´s and DSRIP Performing Provider Systems
- "Community" Referrals will:
- Require referee to provide information including: affirmatively indicating they have parent/guardian consent to make a referral to a Health Home, will require Medicaid CIN number, will require parent/guardian contact information, and whether a member is receiving preventive services and by which entity (if the information is provided),
- Provide "feedback" to the referring entity including: if the member is already enrolled in a Health Home and which one, confirmation the referral was made
- Community referrals made by LDSS for foster care children will reflect the parent/guardian role of the LDSS, and the requirement that the voluntary foster care agency that the LDSS assigns the child for care management will be the Health Home care manager for that child
- MAPP will use the information provided by the referring entity to make an assignment
- The MAPP logic for making an assignment from a community referral to a Health Home will take into account connectivity (i.e., loyalty match) to the network of Health Homes designated to serve children, including whether a member is enrolled in preventative services (if the information is provided by the referring entity) and for members enrolled in Plans, contractual relationships between the Plan and Health Homes
Draft Direct Referrals for Assignment and Enrollment
- Direct referrals are made by Health Homes and care managers
- Health Homes and care managers/voluntary foster care providers for foster care children, with parent/guardian and LDSS consent in the case of foster care, may make direct referrals to a Health Home
- Health Homes and care managers making direct referrals will be provided information regarding contractual relationships between the member´s Plan and Health Homes
- Assignments cannot be made to Health Homes where there is no contractual relationship with the Plan (there will be exceptions and procedures developed for foster care assignments that involve relocation of a child to an area outside of the plan´s network)
- Health Homes and care managers will make direct assignments – enter child in outreach segment (if consent to enroll has not been obtained) or care management enrollment segment (if consent has been obtained)
- Plans can identify eligible children and make assignments to Health Homes
- Within this overall structure the State is working with the MAPP builders to identify various use cases to determine assignment algorithms under various scenarios (including for children in Foster Care)
- May 11 Webinar will review various use cases and provide time for questions, answers and feedback
Consent for Children Enrollment in Health Home and Health Information Sharing
Consent for Enrolling Children in Health Home and Sharing Health Information
- The State Agency Partners and their Legal Departments developed draft consent forms
- The State Team consulted with a group (3 meetings) of Health Homes and others that requested to be involved in development of draft forms
- Draft forms and FAQ are posted to the DOH Website
- As discussed in more detail, the drafts contemplate, with limited exceptions parental consent for enrollment and sharing of health information
Laws and Regulations Regarding Consent and Confidentiality for Health Services to Minors
- HIPAA
- The New York State Department of Health
- Public Health Law (PHL) 2504
- Article 27–f
- Social Services Law (SSL) 365–l
- The Office of Mental Health
- Mental Hygiene Law(MHL) 33.21, 33.16, 9.13
- The Office of Alcoholism and Substance Abuse Services
- MHL 22.11
- 42 Code of Federal Regulations (CFR) 2.14
- The Office of Children and Family Services
- SSL 383–b and 398(6); FCA 355.4
- 18 New York Codes, Rules and Regulations 441.22
Under Current Law and Regulations, Parental Consent, with only Limited Exceptions, is Required for Children to be Enrolled in Health Home
- The PHL defines Health Home care management as a health service, and as such requires the consent of a parent, guardian or legally authorized representative to enroll minors in a Health Home and authorize information sharing among the minors´ providers.
- Exception: A minor who is married, pregnant, or a parent can consent to enrollment into a Health Home and provide authorization to have their health information shared (the current consent form DOH 5055 would be used in these circumstances)
Defining Legally Authorized Representative
- Legally authorized representative for the purpose of enrollment in a Health Home is defined as: "a person or agency authorized by state, tribal, military or other applicable law, court order or consent to act on behalf of a person in making health care decisions".
- Legally authorized representative for the purpose of sharing health information is defined as "a person or agency authorized by state, tribal, military or other applicable law, court order or consent to act on behalf of a person for the release of medical information".
- For certain categories of foster care children (e.g., abused/neglected children), a legally authorized representative for enrollment is a commissioner/or designee of a local department of social services.
Exceptions within the Laws and Regulations
- Minors may consent to receive certain Health Care services (other than Health Home services), including:
- Family Planning
- Emergency Contraception
- Abortion
- Sexually Transmitted Infection Testing and Treatment
- HIV Testing
- Prenatal Care, Labor/Delivery
- Chemical Dependency
- Drug and Alcohol Treatment
- Sexual Assault Services
- Mental Health Services: For minors over the age of twelve, their clinician may consult with them prior to releasing information
- A minor who consented to receive these services or treatment can also consent to the sharing of information regarding those services or treatment
Development of Draft Consent Forms
- Based on this information five Consent Forms have been drafted:
- One Form to enroll the child in Health Homes (Form A)
- One Form to allow for health Information to be shared among Health Home Partners (Form B)
- One Form to allow for educational documents for Individualized Education Program (IEP) to be shared among Health Home Partners (Form C)
- One Form to withdraw Health Home Enrollment and Information Sharing
- One Form to withdraw release of educational records
- The Department has also made available Frequently Asked Questions (FAQ)
- Training Webinar on Forms May 18, 2015
MAPP Will Help Manage Health Home Consent for Children
- Consent to Refer: MAPP will require a user to indicate if consent to refer was received. If consent is not received, the user will be prevented from submitting a referral in MAPP.
- Consent to Enroll: MAPP will require a user to indicate if consent to enroll was received. If consent is not received, the user will be prevented from recording enrollment services in MAPP.
- Consent to Share Information: MAPP will allow a user to indicate if a minor has declined consent to share information for protected services described on slide 56 with a parent/guardian. If consent is declined, the system will warn users. The warning message will advise the user that the minor has declined consent to share information for protected services and procedures.
*In future phases of MAPP, consent management will be expanded to enable individuals to identify consent to sharing WHAT INFORMATION with WHOM for WHAT PURPOSE (i.e., the information included on the draft consent form)
Next Steps
- Training and Webinar Schedule
- Activities Post Health Home Designation
| Health Homes (HH) For Children Training Schedule (As of April 29, 2015, See DOH Website for Updates) |
|
|---|---|
| Training Session (Webinars unless noted) | Date |
| Early Intervention Coordinating Council | September 19, 2014 |
| Overview of HH Application and Design Updates | November 5, 2014 |
| Commissioner´s Advisory Panel for Special Education Services | February 27, 2015 |
| Health Information Technology | March 4, 2015 |
| Updates Design and Implementation | April 29, 2015 |
| Referral Enrollment Process for Children in MAPP | May 11, 2015 |
| Transition of Children´s OMH TCM Providers to Health Home | TBD |
| Health Home Consent Forms for Children | May 18, 2015 |
| Data Exchange Application and Agreements | May 27, 2015 |
| Webinar for CAH and Waiver Providers (Health Home and Managed Care Transition) | June 10, 2015 |
| Implementation and Post Designation Activities of Children´s Health Home | June 18, 2015 |
| CANS–NY On Line Training Begins | July 2015 |
| CANS–NY 2 – Day In Person Training by John Lyons– Albany | Last Week July 2015 |
| MAPP Training (Series of Sessions) | Begins July 2015 |
| State Education Department Training for Health Homes | July 29, 2015 |
| CANS–NY 2 – Day In Person Training by John Lyons– Rochester | Second Week August 2015 |
| CANS–NY 2 – Day In Person Training by John Lyons– New York City | Fourth Week August 2015 |
| CANS–NY 2 – Day In Person Training by John Lyons – New York City | Fourth Week of September 2015 |
| Early Intervention Training for Health Homes | Fall 2015 |
| Health Home Training for Early Intervention Providers | Fall 2015 |
| Training for Pediatricians – Overview HH and Referrals | Fall 2015 |
| Commissioners Advisory Panel for Special Education – Follow Up Session | Fall 2015 |
| Training for School Districts (TBD/ School Nurses) | Fall 2015 |
| Training for Local Probation Offices – Overview HH and Referrals | Fall 2015 |
| Training for HH Juvenile Justice / Probation Offices | Fall 2015 |
| Health Homes (HH) For Children Training Schedule For Voluntary Foster Care Providers As of April 29, 2015 – See DOH Website for Updates Webinars unless Noted |
|
|---|---|
| Training Session | Date |
| Overview of Health Homes | May 14, 2015 |
| Administrator Track | |
| What it Means to Be Downstream Provider | May 26, 2015 |
| Outcomes and Quality Assurance | June 23, 2015 |
| Finances and Billing | July 21, 2015 |
| Policies and Procedures for NYS Children´s Health Homes | August 18, 2015 |
| Care Manager Track | |
| Roles of Care Managers, Case Managers and Case Planners | June 18, 2015 |
| Enrollment, Consent and Confidentiality | July 16, 2015 |
| Developing the Care Plan – In Person 9 sessions across the State | July 27 – September 17 |
| Supervision – Care Manager Supervisors | July 20, 2015 |
| Final Wrap–up | October 15, 2015 |
| Implementing and Re–evaluating the Care Plan | November 5, 2015 |
| Overview of Motivational Interviewing | December 3, 2015 |
Post Designation Activities (June 15th)
- Health Homes and Plans enter into contracts/Administrative Services Agreements (ASA)
- Newly designated Health Homes must enter into Data Exchange Application Agreements (DEAAs) with Department of Health
- Existing Health Homes with no change in governance structure do not need to amend the DEAAs
- New and existing Health Homes need to execute Business Associate Agreements (BAAs) with downstream care managers and new network partners
- May 27, 2015 Webinar will provide additional details
- New Health Homes and downstream care managers need to acquire access to HCS
- Required to access MAPP and CANS–NY
- HCS access is not required to access CANS–NY training (note: training is a prerequisite to accessing the CANS–NY tool in MAPP)
- Entities, initially LGUs and LDSSs will need to acquire access to make community referrals for children only
- Required to access MAPP and CANS–NY
- Finalize list of network providers, including care managers for MAPP
- Existing Health Homes are encouraged to secure a new NPI for their children‘s Health Home program
- DOH Website information for Children´s Health Homes (referral contacts)
Updates, Resources, Training Schedule and Questions
- Please send any questions, comments or feedback on Health Homes Serving Children to: hhsc@health.ny.gov or contact the Health Home Program at the Department of Health at 518.473.5569
- Stay current by visiting our website
Appendix
Appendix
Current and Proposed Health Home Eligibility Criteria
Children´s HCBS Services
- Care Coordination (for children who do not meet HH criteria)
- Habilitative Skill Building
- Family/Caregiver Supports & Services
- Crisis Respite
- Planned Respite
- Prevocational Services
- Supported Employment
- Community Advocacy & Support
- Non–Medical Transportation
- Day Habilitation
- Adaptive & Assistive Equipment
- Accessibility Modifications
- Palliative Care
Children´s State Plan Services
- Crisis Intervention
- Psychosocial Rehabilitation
- Community Psychiatric Support & Treatment (CPST)
- Other Licensed Practitioners
- Family Peer Support Services
- Youth Peer Support and Training
| Current Health Home Eligibility Criteria and Proposal to Modify Health Home Eligibility Criteria (Modifications in Bold) |
|---|
Person must be enrolled in Medicaid and have:
|
Chronic Conditions Include:
|
Health Home Eligibility Criteria
| Appropriateness Criteria for Health Home Eligibility |
|---|
Appropriateness Criteria: Individuals meeting the Health Home eligibility criteria must be appropriate for Health Home care management. Assessing whether an individual is appropriate for Health Homes includes determining if the person is:
|
SED Definition for Health Home – SED is a single qualifying chronic condition for Health Home and is defined as a child or adolescent (under the age of 21) that has a designated mental illness diagnosis in the following Diagnostic and Statistical Manual (DSM) categories* as defined by the most recent version of the DSM of Mental Health Disorders AND has experienced the following functional limitations due to emotional disturbance over the past 12 months (from the date of assessment) on a continuous or intermittent basis
| SED Definition for Health Home – DSM Qualifying Mental Health Categories* |
|---|
|
| Functional Limitations Requirements for SED Definition of Health Home |
|---|
To meet definition of SED for Health Home the child must have experienced the following functional limitations due to emotional disturbance over the past 12 months (from the date of assessment) on a continuous or intermittent basis
|
*Any diagnosis in these categories can be used when evaluating a child for SED. However, any diagnosis that is secondary to another medical condition is excluded.
Health Home Eligibility Criteria
| Trauma at Risk for Another Chronic Condition |
|---|
| Trauma is defined as exposure to a single severely distressing event, or multiple or chronic or prolonged traumatic events as a child or adolescent, which is often invasive and interpersonal in nature. Trauma includes complex trauma exposure which involves the simultaneous or sequential occurrence of child maltreatment, including psychological maltreatment, neglect, exposure to violence, and physical and sexual abuse. A child or adolescent who has experienced trauma would be defined to be at risk for another chronic condition if they have one or more functional limitations that interfere with their ability to function in family, school, or community activities, or they have been placed outside the home. Functional limitations are defined as difficulties that substantially interfere with or limit the child in achieving or maintaining developmentally appropriate social, behavioral, cognitive, communicative, or adaptive skills, or for a child who experienced trauma due to child maltreatment, a functional limitation is defined as a serious disruption in family relationships necessary for normal childhood growth and development. |