Children's Managed Care Design Update
- Presentation is also available in Portable Document Format (PDF, 888KB)
The Children´s MRT Behavioral Health Subcommittee
October 27, 2014
New York City
Agenda
- Welcome & Introductions
- Design Updates
- Quality & Performance Measurement
Children´s Leadership Team
- Donna Bradbury, Associate Commissioner, Division Of Integrated Community Services For Children & Families, NYSOMH
- Lana I. Earle, Deputy Director, Division of Program Development and Management, Office of Health Insurance Programs, NYS DOH
- Steve Hanson, Associate Commissioner, NYS OASAS
- Linda Kelly, Project Director, Behavioral Health Transition, NYS DOH
- Laura Velez, Deputy Commissioner, Child Welfare & Community Services, NYS OCFS
DESIGN UPDATES
BENEFIT PACKAGE: SPA & HCBS
- Further polishing, particularly around qualifications of staff
- Review of package by OMH´s Multi-cultural Advisory Committee
- Package will serve as the foundation for developing Provider Manual
DRAFT STATE PLAN AMENDMENT
- Mercer completed draft in late August
- Interagency review of SPA application in progress
- Prioritization of submission of SPA to CMS, to build new services early in transition
- Tribal & Public Notices to be posted within next month
TARGET & ELIGIBILITY CRITERIA
- Children from birth to age 21 who have:
- A Psychiatric Diagnosis from the DSM V
- Alcohol or Drug Disorders (291.xx.292.xx.303.xx.305.xx.) or
- Developmental Disorders (299.xx.315.xx.319.xx.) or
- Organic Brain Syndrome (290.xx.293.xx.294xx);
- OR
- Are Medically Fragile;
- OR
- Have been impacted by Physical, Emotional, or Sexual Abuse, Neglect, or Maltreatment;
- AND
- Have Extended Impairment in Functioning
CANS-NY REVISION
- Dr. John Lyons has revised the CANS-NY which is under interagency review:
- Inclusion of 0-5 age group, with an early development module
- Inclusion of 18-21 age group, including modules on transition to adulthood and sexuality
- Addition of modules to: increase tool´s sensitivity to medically fragile children; include additional modules on activities of daily living and independent activities of daily living to comply with BIP requirements; and enhancement of trauma related items
- Interagency team is proposing additional language revisions, instrument flow suggestions, and clarity on scoring.
- The CANS-NY algorithm has been revised to account for distinction between Level of Need and Level of Care, including Health Home acuity levels
- CANS-NY data will eventually be warehoused on the Uniform Assessment System on DOH´s Health Commerce System
HCBS ELIGIBILITY PROCESS
- Proposed flow chart for enrollment process into HCBS benefits
- Clear roles and responsibilities for eligibility screening, LON/LOC determination, initial/provisional service plan, full assessment, service plan development and approval
- Intersection with Health Home Care Coordination and Health Home referral process
- Brainstorming with local government representatives from Mental Hygiene, Social Services and Health Departments along with CLMHD, NYPWA and NYSACHO
- Plan and State Workgroup on October 31
FLEXIBLE SERVICE FUNDS
- OMH will continue to support through State Aid funding flexible service funds for TCM (Medicaid and non-Medicaid) and HCBS Waiver for SFY 2015-2016
- Interagency support for continuing availability of these funds
- Draft guidelines in progress, with projections on numbers of children to be eligible for this support
- Potential for interagency budget request for SFY 2016-2017
HEALTH HOME
- Anticipated release of Final Health Home Application to Serve Children - November 1, 2014
- Health Home Webinar on Final Health Home Application to Serve Children - November 5, 2014 at 10:00 AM - 12:00 PM
- Reserve your seat https://www1.gotomeeting.com/register/403958673
PROPOSED FISCAL ANALYSIS & MODEL BUILDING
- Managed Care Plans will be given a list of designated OMH, OCFS, DOH and OASAS HCBS providers with which to contract for 24 months in order to meet the network adequacy standards
- Plans will be required to pay designated providers fee for service rates for 24 months
- We are proposing a non-risk arrangement for the new HCBS Services and new SPA benefits for 24 months (funding for these services will be outside the Plan premium), but these services will be paid through the Mainstream MMC Plans
- The Plan PMPM will likely increase as a result of the new State Plan services and HCBS Benefits being added to the scope of benefits. This would be similar to PMPM calculations being made for the Adult BH design.
- Mercer to use tested methodology to assist NY in projecting the number of children who may meet the Level of Need criteria
- Cost projections will be developed for LON and LOC populations
- Voluntary foster care agencies will receive a residual Medicaid per diem for some existing services, yet to be developed
PROPOSED PHASE-IN OF HCBS BENEFITS
Year One (2016) - Phase In of Populations
- Children enrolled in 1915c Waivers on 12/31/15 will continue to receive HCBS benefits as transition is implemented in 2016
- Children meeting LOC eligibility (newly identified on and after 1/1/16), including HCBS Expansion Group that are Medicaid eligible by ´family of one´ methodology
- Children who were receiving benefits at LOC intensity, who are ready to step down to LON intensity
Year Two (2017) - Second Phase In
- Children with community Medicaid who meet LON criteria
Year Three (2018) - Last Phase In
- Allow HCBS Expansion Group that meets LON criteria and can be determined Medicaid eligible by ´family of one´ methodology to receive HCBS benefits
QUALITY & PERFORMANCE MANAGEMENT AND EVALUATION
- QARR Overview
- CAHPS Overview
- Adult managed care performance management
- Children´s MRT BH Subcommittee performance recommendations
- Children´s Q&PME Workgroup
- Children´s Network Adequacy Subgroup
Quality Assurance Reporting Requirements (QARR) Overview
Anne Schettine
Office of Quality and Patient Safety
NYS Department of Health
WHAT IS QARR?
- QARR = Quality Assurance Reporting Requirements
- Measurement set for the health care delivery system
- Healthcare Effectiveness Data & Information Set (HEDIS®) measures which are developed by the National Committee for Quality Assurance (NCQA) AND
- New York State-Specific Measures
- CAHPS® - Consumer Assessment of Healthcare Providers and Systems-Satisfaction
- Primary Purpose - comparison of quality performance by health plans using standardized measures from national programs
HISTORY OF QARR
- Public Health Law, Article 29 D, Section 2995
- 1997
- CMS approved 1115 Waiver for New York - the Partnership Plan begins to roll out
- First QARR report completed (1994 data)
- 2001
- Major growth in Medicaid managed care (NYC phases completed and disaster relief enrollment)
- Population changes from Moms and kids
- 2007: Mandatory enrollment of SSI begins
- 2012: Benefit package changes and mandatory enrollment of populations traditionally excluded from Medicaid managed care
- 2013: Health insurance marketplace begins enrollment
- 2015: Mental Health and Substance benefit changes and HARPS
QARR THEN AND NOW
1994
- 43 plans
- 2 payers
- 13 measures
- Areas of measures - prenatal, pediatric, women´s preventive, utilization
2014
- 26 plans
- 4 payers
- 76+ measures
- Areas of measures - children and adolescents, prenatal care, women´s health, chronic diseases, behavioral health, satisfaction, access and utilization
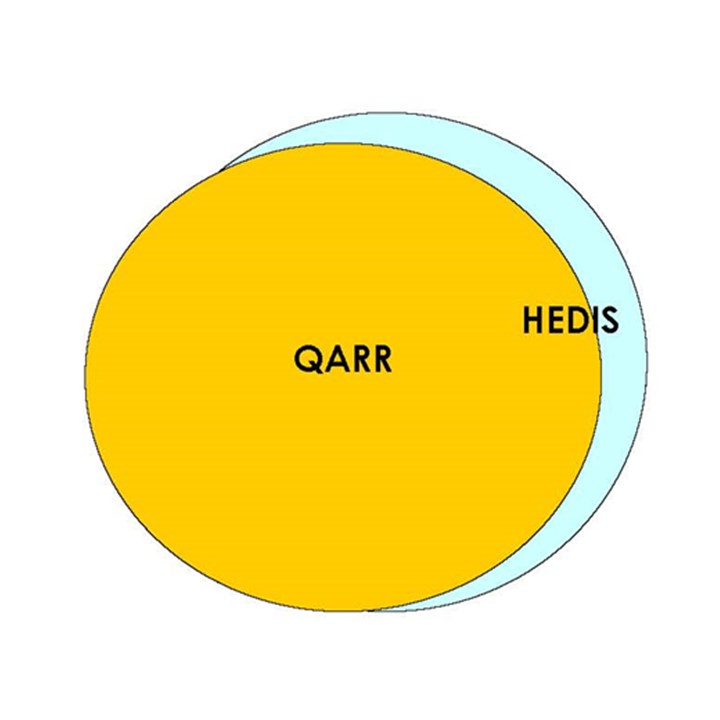
RELATIONSHIP BETWEEN HEDIS & QARR
WHAT ARE WE MEASURING?
- Standardized national measurement set for the ambulatory health care delivery system
- Measures are developed to reflect the quality of care being given in a certain population, condition, or event
- Generally based on recommendations from national organizations or experts in designated areas
- Required for Commercial HMO, Commercial PPO, Medicaid, Child Health Plus and Qualified Health Plans
QARR MEASURES RELATED TO CHILDREN
| Measures | |
|---|---|
| Preventive Care | Adolescent Preventive Care (assessment or counseling for sexual activity, depression, tobacco and alcohol/drug use), Childhood immunization, Adolescent immunization, Lead screening, Weight Assessment and Counseling for Nutrition and Physical Activity |
| Caring For Illness | Appropriate Treatment for URI, Appropriate Testing for Pharyngitis, Asthma medication management and medication ratio |
| Women´s Health | Non-recommended cervical cancer screening for teens, Chlamydia Testing, HPV Vaccination for Adolescent Females |
| Use of Services and Access to Care | Children´s Access to PCPs, Annual Dental Visits, Well care visits for 15 month olds, 3-6 year olds and Adolescents |
| Behavioral Health | Follow Up Care for Children Prescribed ADHD Medication, Follow Up After Hospitalization for Mental Illness |
NEW HEDIS MEASURES FOR 2015
- Use of Multiple Concurrent Antipsychotics in Children and Adolescents
- Use of First-Line Psychosocial Care for Children and Adolescents on Antipsychotics
- Metabolic Monitoring for Children and Adolescents on Antipsychotics
CHILD CAHPS® 5.0 WITH CHILDREN WITH CHRONIC CONDITION MODULE
SATISFACTION SURVEY FOR CHILDREN IN MEDICAID AND CHILD HEALTH PLUS HEALTH PLANS
Office of Quality and Patient Safety
PURPOSE OF SATISFACTION SURVEY
- Measure satisfaction with care for parents of children in Medicaid Managed Care and Child Health Plus programs:
- Comparing health plans
- Comparing experiences for children with chronic conditions to those without chronic conditions
- Reporting for Child Health Insurance Program Reauthorization Act (CHIPRA)
CHILD CAHPS SURVEY CONTENT
- Access to Care - getting tests, routine/urgent/specialist visits
- Experience with Care- doctor communication, collaborative decision making, ratings of doctor and specialist seen most often
- Health Plan Support - customer service, care coordination, specialty services
- Chronic Condition Module - family centered care, access to specialized services, care coordination
Chronic Condition Screen Positive
- Determined by responses from parent/guardian to a series of five sets of questions (self-reported)
- Prescription medicine (other than vitamins)
- Use more than usual medical care, mental health or educational services
- Limited or prevented in ability to do things most children of same age can do
- Special therapy (physical, occupational or speech)
- Emotional, developmental or behavioral problems which needs or gets treatment
- Each screener item has three pieces. In addition to the service needs above, follow up questions relating service to health conditions and expectation that condition will last 12 months must also be ´Yes´ to be considered ´screened positive´ for any item.
Screener Q + due to health condition + lasting 12 months = ´Screened Positive´ - ´CC Positive´ indicates children with one or more positive screeners
USES FOR QARR DATA
- Publications - eQARR, Regional Consumer Guides, Access and Utilization report
- Quality Ratings for QHP´s in Marketplace and Health Plans
- Financial Rewards - Quality Incentive for Medicaid plans based on performance in quality, satisfaction and preventable hospitalization rates
- Quality Improvement Activities - performance matrix and action plans, plan-specific reports, improvement projects and focus studies
- Research - disparity analyses in the demographic report, linking process measures to outcomes, newsletters
WHERE TO FIND QARR DATA AND REPORTS
- Annual Quality Performance Reports (DOH)
- QARR Data (Open Data New York)
- QARR Quality Connection newsletter (HCS)
- Public Health Priority Areas (DOH)
MANAGED CARE QUALITY & PERFORMANCE MEASUREMENT
ADRIENNE RONSANI OMH, QUALITY & PERFORMANCE MEASUREMENT
ADULT OVERVIEW - PERFORMANCE MEASUREMENT
- Performance Measures
- Existing HEDIS/QARR measures for physical and behavioral health for HARP and MCO product lines
- Development of a limited number of new behavioral health measures
- New measures will be derived from claims and encounter data
- First year in QARR will be reported in aggregate only
- Measures include MH outpatient engagement, MH and SUD readmission, linkages to ambulatory care for SUD, and medicated assisted treatment for SUD. Specifics are under development.
- BHO Phase One measures will continue to be run administratively
- Measures are also being proposed for HARPs that are based on data collected from HCBS eligibility assessments. These measures are related to social outcomes - employment, housing, criminal justice, social connectedness, etc.
- Member Satisfaction - all are existing QARR measures
- Based on CAHPS survey
- A recovery focused survey for HARP members is also being developed. Measures derived from this survey may be created in the future.
CHILDREN´S MRT BEHAVIORAL HEALTH SUBCOMMITTEE: PERFORMANCE MEASURE RECOMMENDATIONS, 2011
- Outcomes of behavioral health services for children and their families should be clearly articulated, measured, reported and used to inform policy, services, reimbursement and practice quality.
- Accountability mechanisms should focus on achieving specific child outcomes.
- Accountability should occur at the BH provider level and occur across relevant child serving systems. BH outcomes for children are often achieved by services that extend beyond the BH system.
- Outcome data should be used to improve the quality of services and be linked to performance incentives. Outcomes measures should be reported at the child, provider, system and population levels.
Outcome measures should be developed and applied to appraise performance and improve quality. Critical outcomes are:
- Improvement in psychiatric symptoms for which treatment is sought
- Improvement in functional status (e.g., social, school function)
- Consumer satisfaction/involvement
- Critical incidents
- Success/failure at transition to less intensive level of care
- Access to care
- Medication management
- Cross-systems communication/case planning
- Network adequacy
KIDS LEADERSHIP VISION FOR PERFORMANCE METRICS
- Ensuring that children have needed access to services (in relation to capacity, outcomes of denials and transitions between levels of care)
- Correlation between identified needs and approved service plan
- Child and family functioning improves
- Consumer perception of care
- Patterns of issues with complaints and appeals
- Change in out of state placement rates
- Early screening and service access
- Degree to which providers are in networks that are trauma sensitive
- Medication management related to psychotropic use
CHILDREN´S Q&PME WORKGROUP
- The workgroup reviewed measures currently in use for youth in managed care (QARR, PSYCKES, BHO Phase I).
- Focused on using stakeholder and MRT feedback to identify gaps in current measures.
- A gap identified was measures related to social and resiliency outcomes such as school functioning and social skills.
- Issues around managed care plan accountability and an appropriate data source were challenges to formulating social and resiliency measures.
- Adults are using HCBS eligibility assessment for a data source for these types of measures.
NETWORK ADEQUACY
- A subgroup of the Q&PME group drafted partial recommendations for minimum network standards and appointment availability.
- Used adult recommendations as a foundation, however children´s system is more focused on services.
- Reviewed number of mental health and SUD programs in each county to ensure realistic standards.
- Next steps:
- gather more information on current waiver service availability;
- add Care at Home and Palliative Care standards;
- finalize recommendations.
QUESTIONS?
Angela Keller, LMSW
Medicaid Managed Care Transition Consultant
Angela.Keller@omh.ny.gov
Follow Us