MRT Demonstration Section 1115 Quarterly Report and Annual Report
- Report also available in Portable Document Format (PDF)
Demonstration Year: 23 (4/1/2021 - 3/31/2022) Federal Fiscal Quarter: 4 (7/01/2021 - 9/30/2021)
I. Introduction
In July 1997, New York State received approval from the Centers for Medicare and Medicaid Services (CMS) for its Partnership Plan Medicaid Section 1115 Demonstration. In implementing the Partnership Plan Demonstration, it was the State's goal to:
- Improve access to health care for the Medicaid population;
- Improve the quality of health services delivered;
- Expand access to family planning services; and
- Expand coverage to additional low-income New Yorkers with resources generated through managed care efficiencies.
The primary purpose of the Demonstration was to enroll a majority of the State's Medicaid population into managed care, and to use a managed care delivery system to deliver benefits to Medicaid recipients, create efficiencies in the Medicaid program and enable the extension of coverage to certain individuals who would otherwise be without health insurance.
The Partnership Plan Demonstration was originally authorized for a five-year period and has been extended several times. CMS had approved an extension of the 1115 waiver on September 29, 2006 for the period beginning October 1, 2006 and ending September 30, 2010. CMS subsequently approved a series of short-term extensions while negotiations continued on renewing the waiver into 2016.
There have been several amendments to the Partnership Plan Demonstration since its initial approval in 1997. CMS approved three waiver amendments on September 30, 2011, March 30, 2012 and August 31, 2012, incorporating changes resulting from the recommendations of Governor Cuomo's Medicaid Redesign Team (MRT). CMS recently approved the DSRIP and Behavioral Health amendments to the Partnership Plan Demonstration on April 14, 2014 and July 29, 2015, respectively.
New York State's Federal-State Health Reform Partnership (F-SHRP) Medicaid Section 1115 Demonstration expired on March 31, 2014. Populations in the F-SHRP were transitioned into the 1115 Partnership Plan Waiver. A final draft evaluation report was submitted to CMS on February 11, 2015 and was approved by CMS on May 24, 2016.
On May 28, 2014, New York State submitted an application requesting an extension of the Partnership Plan 1115 Demonstration for five years. On May 30, 2014, CMS accepted New York's application as complete and posted the application for a 30-day public comment period. A temporary extension was granted on December 31, 2014 which extended the waiver through March 31, 2015. Subsequent temporary extensions were granted through December 7, 2016. New York's 1115 Demonstration was renewed by CMS on December 7, 2016 through March 31, 2021. At the time of renewal, the Partnership Plan was renamed New York Medicaid Redesign Team (MRT) Waiver. On April 19, 2021 CMS approved New York's request to exempt MMMC enrollees from cost sharing by waiving comparability requirements to align with the New York's social services law, except for applicable pharmacy co-payments described in the STCs. On August 2, 2021 CMS approved New York's request to create a streamlined children's model of care for children and youth under 21 years of age with behavioral health (BH) and HCBS needs, including medically fragile children, children with a BH diagnosis, children with medical fragility and developmental disabilities, and children in foster care with developmental disabilities. On August 2, 2021 CMS approved New York's request to create a streamlined children's model of care for children and youth under 21 years of age with behavioral health (BH) and HCBS needs, including medically fragile children, children with a BH diagnosis, children with medical fragility and developmental disabilities, and children in foster care with developmental disabilities. On December 19, 2021 CMS approved New York's request to limit the nursing home benefit in the partially capitated Managed Long Term Care (MLTC) plans to three months for enrollees who have been designated as "long-term nursing home stays" (LTNHS) in a skilled nursing or residential health care facility. The amendment also implements a lock-in policy that allows enrollees of partially capitated MLTC plans to transfer to another partially capitated MLTC plan without cause during the first 90 days of a 12-month period and with good cause during the remainder of the 12-month period.
New York submitted a three-year waiver extension request to CMS on March 5, 2021. CMS granted a temporary extension of the 1115 waiver through March 31, 2022.
New York is well positioned to lead the nation in Medicaid reform. Governor Cuomo's Medicaid Redesign Team (MRT) has developed a multi-year action plan (Plan to Transform the Empire State 's Medicaid Program) that when fully implemented will not only improve health outcomes for more than five million New Yorkers but also bend the state's Medicaid cost curve.
Significant federal savings have already been realized through New York's MRT process and substantial savings will also accrue as part of the 1115 waiver.
New York is well positioned to lead the nation in Medicaid reform. Governor Cuomo's Medicaid Redesign Team (MRT) has developed a multi-year action plan (A Plan to Transform the Empire State's Medicaid Program) that when fully implemented will not only improve health outcomes for more than five million New Yorkers but also bend the state's Medicaid cost curve. Significant federal savings have already been realized through New York's MRT process and substantial savings will also accrue as part of the 1115 waiver.
II. Enrollment: Fourth Quarter
MRT Waiver - Enrollment as of September 2021
| Demonstration Populations (as hard coded in the CMS 64) |
Current Enrollees (to date) |
# Voluntary Disenrolled in Current Quarter |
# Involuntary Disenrolled in Current Quarter |
|---|---|---|---|
| Population 1 - TANF Child 1 - 20 years in Mandatory Counties as of 10/1/06 | 469,920 | 6,106 | 33,858 |
| Population 2 - TANF Adults aged 21 through 64 in mandatory MC counties as of 10/1/06 | 55,983 | 1,207 | 1,165 |
| Population 3 - TANF Child 1 - 20 ('new' MC Enrollment) | 19,859 | 233 | 3,391 |
| Population 4 - TANF Adults 21 - 64 ('new' MC Enrollment) | 37,681 | 592 | 890 |
| Population 5 - Safety Net Adults | 237,331 | 5,405 | 94,153 |
| Population 6 - Family Health Plus Adults with Children | 0 | 0 | 0 |
| Population 7 - Family Health Plus Adults without Children | 0 | 0 | 0 |
| Population 8 - Disabled Adults and Children 0 - 64 (SSI 0-64 Current MC) | 143,568 | 1,642 | 66 |
| Population 9 - Disabled Adults and Children 0 - 64 (SSI 0-64 New MC) | 66,497 | 3,212 | 152 |
| Population 10 - Aged or Disabled Elderly (SSI 65+ Current MC) | 62,044 | 275 | 12 |
| Population 11 - Aged or Disabled Elderly (SSI 65+ New MC) | 9,290 | 1,860 | 64 |
MRT Waiver - Voluntary and Involuntary Disenrollment
| Voluntary Disenrollments | |
|---|---|
| Total # Voluntary Disenrollments in Current Demonstration Year | 20,532 or an approximate 20.5% decrease from last Q |
Reasons for voluntary disenrollment's: Enrollment in another plan; approved enrollee request to qualify as either exempt or excluded; relocation to residence outside county of enrollment; and Local Department of Social Services (LDSS) approval to disenroll based upon appropriate cause.
WMS continues to send select closed cases to New York State of Health. Consequently, the disenrollment numbers now draw on a smaller WMS population contributing to an overall general decline in voluntary disenrollment.
Voluntary disenrollment declined due to a decline in the number of disenrollments due to incarceration and to a decline in the disenrollment category "Enrolled in Other Plan."
| Involuntary Disenrollments | |
|---|---|
| Total # Involuntary Disenrollments in Current Demonstration Year | 133,751 or an approximate 30.2% increase from last Q |
Reasons for involuntary disenrollment's: Loss of Medicaid eligibility including death, plan termination, and retro disenrollment.
WMS continues to send select closed cases to New York State of Health. Consequently, the disenrollment numbers now draw on a smaller WMS population contributing to an overall general decline in involuntary disenrollment.
Involuntary disenrollment increased due to an increase in MAGI case closures that were subsequently sent to NYSoH for redetermination.
MRT Waiver-Affirmative Choices
| Mainstream Medicaid Managed Care | ||||
|---|---|---|---|---|
| Region | Roster Enrollment | New Enrollment | Auto-assigned | Affirmative Choices |
| July 2021 | ||||
| New York City | 771,533 | 18,627 | 1,826 | 16,801 |
| Rest of State | 347,448 | 9,489 | 718 | 8,771 |
| Statewide | 1,118,981 | 28,116 | 2,544 | 25,572 |
| August 2021 | ||||
| New York City | 710,611 | 12,469 | 2,084 | 10,385 |
| Rest of State | 348,961 | 7,171 | 949 | 6,222 |
| Statewide | 1,059,572 | 19,640 | 3,033 | 16,607 |
| September 2021 | ||||
| New York City | 713,901 | 12,495 | 2,161 | 10,334 |
| Rest of State | 351,031 | 6,382 | 722 | 5,660 |
| Statewide | 1,064,932 | 18,877 | 2,883 | 15,994 |
| Fourth Quarter | ||||
| Region | Total Affirmative Choices | |||
| New York City | 37,520 | |||
| Rest of State | 20,653 | |||
| Statewide | 58,173 | |||
| HIV SNP Plans | ||||
|---|---|---|---|---|
| Region | Roster Enrollment | New Enrollment | Auto-assigned | Affirmative Choices |
| July 2021 | ||||
| New York City | 12,871 | 148 | 0 | 148 |
| Rest of State | 20 | 3 | 0 | 3 |
| Statewide | 12,891 | 151 | 0 | 151 |
| August 2021 | ||||
| New York City | 12,770 | 159 | 0 | 159 |
| Rest of State | 18 | 0 | 0 | 0 |
| Statewide | 12,788 | 159 | 0 | 159 |
| September 2021 | ||||
| New York City | 12,782 | 154 | 0 | 154 |
| Rest of State | 18 | 0 | 0 | 0 |
| Statewide | 12,800 | 154 | 0 | 154 |
| Fourth Quarter | ||||
| Region | Total Affirmative Choices | |||
| New York City | 461 | |||
| Rest of State | 3 | |||
| Statewide | 464 | |||
| Health and Recovery Plans Disenrollment | ||||
|---|---|---|---|---|
| FFY 21 - Q4 | ||||
| Voluntary | Involuntary | Total | ||
| July 2021 | 556 | 1,310 | 1,866 | |
| August 2021 | 577 | 1,031 | 1,608 | |
| September 2021 | 554 | 521 | 1,075 | |
| Total: | 1,687 | 2,862 | 4,549 | |
III. Outreach/Innovative Activities
Outreach Activities
A. New York Medicaid Choice (NYMC) Field Observations Federal Fiscal Quarter: 4 (7/1/2021 - 9/30/2021) Q4 FFY 2021
As of the end of the fourth federal fiscal quarter (end of September 2021), there were 2,946,558 New York City Medicaid consumers enrolled in mainstream Medicaid Managed Care Program and 77,002 Medicaid consumers enrolled in Health and Recovery Plan (HARP). MAXIMUS, the Enrollment Broker for the New York Medicaid CHOICE program (NYMC), conducted in person outreach, education, and enrollment activities in Human Resources Administration (HRA) facilities throughout the five boroughs of New York City.
During the reporting period, MAXIMUS Field Customer Service Representatives (FCSRs) conducted personal and phone outreach in 12 HRA facilities open to the public and has suspended outreach activities at 17 HRA facilities temporarily closed due to COVID-19. MAXIMUS reported that 7,885 clients were educated about enrollment options and made an enrollment choice including 411 clients in person and 7,474 clients through phone.
Contract Monitoring Unit (CMU) is responsible for monitoring outreach activities conducted by FCSRs to ensure that approved presentation script is followed and required topics are explained. Deficiency found is reported to MAXIMUS Field operation monthly. Due to COVID-19, CMU field monitoring has been suspended since 3/23/2020; therefore, no activity was conducted for the reporting period.
B. Auto-Assignment (AA) Outreach Calls for Fee-For-Service (FFS) Consumers
In addition to face-to-face informational sessions, FCSRs make outreach calls to FFS community clients and FFS Nursing Home (NH) clients identified for plan auto-assignment. A total of 19,597 FFS community clients were reported on the regular auto-assignment list, 3,030 clients responded to the call that generated 2,870 enrollments. Of the total of 114 FFS NH clients
reported on NH auto-assignment list, 19 (17%) clients and/or authorized representatives made a Plan selection.
C. NYMC HelpLine Observations July-September 2021
CMU resumed NYMC HelpLine observations effective January 2021. CMU is responsible for observing calls made by Downstate residents, including residents enrolled in managed care, and is committed to observing all Customer Service Representatives (CSRs) answering New York City calls every month. NYMC reported that 56,900 calls were received by the Helpline and 52,658 or 93% were answered. Calls answered were handled in the following languages: English: 32,975 (62%); Spanish: 6,438 (12%); Chinese: 2,948 (5%); Russian: 421 (2%); Haitian/Creole: 108 (1%); and other: 9,768 (18%).
MAXIMUS records 100% of the calls received by the NYMC HelpLine. CMU listened to 1,842 recorded calls. The call observations were categorized in the following manner:
| CMU Monitoring of Call Center Report - 4th Quarter 2021 | ||||||
|---|---|---|---|---|---|---|
| General Information | Phone Enrollment | Phone Transfer | Public Calls | Disenrollment Calls | Dual Segment | Total |
| 1,397 (76%) | 40 (2%) | 47 (3%) | 258 (14%) | 100 (5%) | 0 (0%) | 1,842 |
A total of 1,083 (59%) recorded calls observed were unsatisfactory including 1,034 calls with single infraction and 49 calls with multiple infractions, a total of 1,132 infractions/issues reported to MAXIMUS. The following summarizes those observations:
- Process: 1,110 (98%) - CSRs did not correctly document or failed to document the issues presented; did not provide correct information to the caller; or did not repeat the issue presented by the caller to ensure the information conveyed was accurately captured or correct.
- Key Messages: 12 (1%) - CSRs incorrectly explained or omitted how to navigate a managed care plan; use of emergency room; preventative care/explanation of PCP; and, referrals for specialists.
- Customer Service: 10 (1%) - Consumers were put on hold without an explanation or were not offered additional assistance.
A total of 1,132 corrective action plans were implemented for the reporting quarter. Corrective actions include, but are not limited to, staff training and an increase in targeted CSR monitoring to ensure compliance.
Annual Outreach Activities
NYMC Field Observations
As of the end of the federal fiscal year 2021 (end of September 2021), there were 2,946,558 New York City Medicaid consumers enrolled in the mainstream Medicaid Managed Care Program and 77,002 Medicaid consumers enrolled in Health and Recovery Plan (HARP). MAXIMUS, the Enrollment Broker for the New York Medicaid CHOICE program (NYMC), conducted in person outreach, education, and enrollment activities in Human Resources Administration (HRA) facilities throughout the five boroughs of New York City
Due to COVID-19, outreach activities at 21 of the 33 HRA facilities have been temporarily closed. During the reported period Maximus Field Customer Service Representatives (FCSR's) conducted personal and phone outreach in 12 HRA facilities open to the public. Maximus reported that 41,479 clients were educated about enrollment options and made an enrollment choice including 1,574 clients in person and 39,905 clients through phone.
Contract Monitoring Unit (CMU) is responsible for monitoring outreach activities conducted by FCSRs to ensure that approved presentation script is followed and required topics are explained. Deficiencies found are reported to Maximus field operation monthly. CMU field monitoring has been suspended since 3/23/2020; therefore, no activity was conducted for the fiscal year.
Auto-Assignment (AA) Outreach Calls for Fee-For Service (FFS) Consumers
In addition to face-to-face informational sessions, FCSRs make outreach calls to FFS community clients and FFS Nursing Home (NH) clients identified for plan auto-assignment. A total of 83,400 FFS community clients was reported on the regular auto-assignment list, 12,234 (15%) clients responded to the call that generated 13,243 enrollments. Of the total of 417 FFS NH clients reported on NH auto-assignment list, 76 (18%) clients and/or authorized representatives made a plan selection.
NYMC HelpLine Observations
CMU resumed NYMC HelpLine observations effective January 2021. CMU is responsible for observing calls made by Downstate residents, including residents enrolled in managed care, and is committed to observing all Customer Service Representatives (CSRs) answering New York City calls every month. NYMC reported that 221,572 calls were received by the Helpline and 207,241 or 94% were answered. Calls answered were handled in the following languages: English: 137,044 (66%); Spanish: 25,676 (12%); Chinese: 10,845 (5%); Russian: 2,059 (1%); Haitian/Creole: 349 (1%); and other: 31,268 (15%).
MAXIMUS recorded 100% of the calls received by the NYMC HelpLine 10/1/2020 through- 9/30/2021. CMU listened to 10,103 recorded calls for the period from 1/1/2021 to 9/30/2021.
The call observations were categorized in the following manner:
| CMU Monitoring of Call Center Report – 1/1/2021 - 9/30/2021 | ||||||
|---|---|---|---|---|---|---|
| General Information | Phone Enrollment | Phone Transfer | Public Calls | Disenrollment Calls | Dual Segment | Total |
| 6,464 (64%) | 467 (5%) | 699 (7%) | 1,826 (18%) | 646 (6%) | 1 (0%) | 10,103 |
A total of 4,849 (48%) recorded calls observed was unsatisfactory including 4,442 calls with single infraction and 407 calls with multiple infractions, A total of 5,544 infractions/issues reported to MAXIMUS. The following summarizes those observations:
- Process: 5,320 (96%) - CSRs did not correctly document or failed to document the issues presented; did not provide correct information to the caller; or did not repeat the issue presented by the caller to ensure the information conveyed was accurately captured or correct.
- Key Messages: 106 (2%) - CSRs incorrectly explained or omitted how to navigate a managed care plan; use of emergency room; preventative care/explanation of PCP; and, referrals for specialists.
- Customer Service: 118 (2%) - Consumers were put on hold without an explanation or were not offered additional assistance.
A total of 5,544 corrective action plans were implemented for the reporting quarter. Corrective actions include, but are not limited to, staff training and an increase in targeted CSR monitoring to ensure compliance.
IV. Operational/Policy Developments/Issues
A. Plan Expansions, Withdrawals, and New Plans
None to report for the 4th Quarter. Several expansions and new plan application reviews are ongoing.
Annual:
1st Quarter
- The Department approved a change of control and legal name change for HealthNow New York. The Certificate of Authority has been updated to reflect a new legal name of Highmark Western and Northeastern New York Inc.
- On November 1, 2020, HealthFirst PHSP, Inc. was approved to expand its Medicaid Managed Care (MMC) and Health and Recovery Plan (HARP) service areas to include Rockland County.
2nd Quarter
- A new application was received by the Department for review and approval as an Article 44 mainstream Medicaid HMO on behalf of Integra MLTC, Inc with assumed name, Integra Managed Care.
3rd Quarter
- United Health Care of New York was approved to expand into Dutchess and Erie counties serving the Child Health Plus population.
B. Medicaid Managed Care/Family Health Plus/HIV Special Needs Plan Model Contract
The March 1, 2021 Medicaid Managed Care/HIV Special Needs Plan/Health and Recovery Plan Model Contract (Model Contract) was submitted to CMS for approval in federal fiscal year (FFY) 2018-2021. All 19 resultant contracts have been executed by New York State and have been submitted to CMS for final approval. At the close of the quarter, these executed contracts remained under review by CMS.
On June 18, 2021, New York State submitted to CMS an amendment to the March 1, 2021 Model Contract that includes emergency contract provisions related to the COVID-19 public health emergency. At the close of the quarter, this emergency amendment was still under review with CMS.
Annual:
The March 1, 2021 Medicaid Managed Care/HIV Special Needs Plan/Health and Recovery Plan Model Contract (Model Contract) was submitted to CMS for approval in federal fiscal year (FFY) 2021-2020. All 19 resultant contracts have been executed by New York State and have been submitted to CMS for final approval. At the close of the fiscal year, the Model Contract and these resultant executed contracts remained under review by CMS.
On June 18, 2021, New York State submitted to CMS an amendment to the March 1, 2021 Model Contract that includes emergency contract provisions related to the COVID-19 public health emergency. At the close of the fiscal year, this emergency amendment was still under review with CMS.
C. Health Plans/Changes to Certificates of Authority
None to report for the 4th Quarter.
Annual:
The Department updated the Certificate of Authority to reflect that for United Healthcare of New York is conditionally certified to provide Integrated Benefits for Dually Eligible Enrollees Program in the counties of Albany, Bronx, Broome, Cayuga, Chautauqua, Chemung, Chenango,
Clinton, Columbia, Dutchess, Erie, Essex, Genesee, Greene, Herkimer, Jefferson, Kings, Lewis, Livingston, Madison, Monroe, Nassau, New York, Niagara, Oneida, Onondaga, Ontario, Orange, Orleans, Oswego, Queens, Rensselaer, Richmond, Rockland, Schenectady, Seneca, Suffolk, Tioga, Ulster, Warren, Wayne, Westchester, Wyoming, and Yates are designated for the Integrated Dual Benefit Program.
The Department updated the Certificate of Authority to reflect that United Healthcare of New York is certified to provide Child Health Plus benefits in the counties of Dutchess and Erie.
The Department updated the Certificate of Authority to reflect that MetroPlus Health Plan Inc.is conditionally certified to provide Integrated Benefits for Dually Eligible Enrollees in the counties of Bronx, Kings, New York, Queens, and Richmond. Additionally, the counties of Orange and Putnam have been removed as an update to the approved service area for the Medicaid Advantage Plus line of business.
The Department updated the Certificate of Authority to reflect that New York Quality Healthcare Corporation dba Fidelis is conditionally certified to provide Integrated Benefits for Dually Eligible Enrollees in the counties of Albany, Allegany, Bronx, Broome, Cattaraugus, Cayuga, Chemung, Chenango, Clinton, Columbia, Cortland, Delaware, Dutchess, Erie, Essex, Franklin, Fulton, Greene, Hamilton, Herkimer, Kings, Lewis, Montgomery, Nassau, New York, Niagara, Oneida, Onondaga, Orange, Orleans, Oswego, Otsego, Putnam, Queens, Rensselaer, Richmond, Rockland, Saratoga, Schenectady, Schoharie, Schuyler, Seneca, St. Lawrence, Steuben, Suffolk, Sullivan, Tioga, Ulster, Warren, Washington, Westchester, Wyoming, and Yates.
The Department updated the Certificate of Authority to reflect that HealthPlus HP, LLC is conditionally certified to provide Integrated Benefits for Dually Eligible Enrollees in the counties of Bronx, Kings, Nassau, New York, Queens, and Richmond.
The Department updated the Certificate of Authority to reflect that Hamaspik, Inc. is conditionally certified to provide Medicaid Advantage Program services in the counties of Bronx, Dutchess, Kings, Nassau, New York, Orange, Putnam, Queens, Richmond, Rockland, Sullivan, Ulster, and Westchester.
The Department updated the Certificate of Authority to reflect that Health First PHSP, Inc. is certified to provide Medicaid Managed Care, Health and Recovery Plan and Child Health Plus in Rockland County.
D. CMS Certifications Processed
None to report.
E. Surveillance Activities
BMCCS Surveillance activity completed during the 4th Quarter FFY 2020-2021 includes the following:
One (1) Target Operational Survey were completed during 4th Quarter FFY 2020-2021. An SOD was issued and a POC was accepted for one (1) Plan.
Affinity Health Plan.
VNS Target Survey the Plan was found in compliance. Annual:
End of Year Report for the BMCCS Survey Unit.
BMCCS Surveillance activity completed during the 1st Quarter FFY 2020-2021 includes the following:
One Target Operational survey was completed, and the Plan was found in compliance:
- HIP/Emblem Target Operational Survey
BMCCS Surveillance activity completed during the 2nd Quarter FFY 2020-2021 includes the following:
One (1) Comprehensive Operational Survey, and one Target Operational Survey were completed during 2nd Quarter FFY 2020-2021. An SOD was issued and a POC was accepted for one (1) Plan. One Plan was found in compliance.
- CDPHP Comprehensive Operational Survey
- Molina Target Operational Survey (in compliance)
BMCCS Surveillance activity completed during the 3rd Quarter FFY 2020-2021 includes the following:
One (1) Comprehensive Operational Survey, and two (2) Target Operational Surveys were completed during 3rd Quarter FFY 2020-2021. An SOD was issued and a POC was accepted for one (1) Plan. Two Plans were found in compliance.
- MVP Comprehensive Operational Survey
- Highmark Target Operational Survey (in compliance)
- Healthfirst Target Operational survey (in compliance)
V. Waiver Deliverables
A. Medicaid Eligibility Quality Control (MEQC) Reviews
MEQC Reporting requirements under discussion with CMS
No activities were conducted during FY 2021. Final reports were previously submitted for all reviews except for the one involved in an legal matter.
- MEQC 2008 - Applications Forwarded to LDSS Offices by Enrollment Facilitators
No activities were conducted during the quarter due to a legal matter that is still. - MEQC 2009 - Review of Medicaid Eligibility Determinations and Re-Determinations for Single and Childless Couple Individuals Determined Ineligible for Temporary Assistance
The final summary report was forwarded to the regional CMS office and CMS Central Office on July 1, 2015. - MEQC 2010 - Review of Medicaid Eligibility Determinations and Redeterminations for Persons Identified as Having a Disability
The final summary report was forwarded to the regional CMS office on January 31, 2014 and CMS Central Office on December 3, 2014. - MEQC 2011 - Review of Medicaid Self Employment Calculations
The final summary report was forwarded to the regional CMS office on June 28, 2013 and CMS Central Office on December 3, 2014. - MEQC 2012 - Review of Medicaid Income Calculations and Verifications
The final summary report was forwarded to the regional CMS office on July 25, 2013 and CMS Central Office on December 3, 2014. - MEQC 2013 - Review of Documentation Used to Assess Immigration Status and Coding
The final summary report was forwarded to the regional CMS office on August 1, 2014 and CMS Central Office on December 3, 2014.
B. Benefit Changes/Other Program Changes
Transition of Behavioral Health Services into Managed Care and Development of Health and Recovery Plans (HARPs):
In October 2015 New York State began transitioning the full Medicaid behavioral health system to managed care. The goal is to create a fully integrated behavioral health (mental health and substance use disorder) and physical health service system that provides comprehensive, accessible, and recovery-oriented services. There are three components of the transition: expansion of covered behavioral health services in Medicaid Managed Care, elimination of the exclusion for Supplemental Security Income (SSI), and implementation of Health and Recovery Plans (HARPs). HARPs are specialized plans that include staff with enhanced behavioral health expertise. In addition, individuals who are enrolled in a HARP can be assessed to access additional specialty services called behavioral health Home and Community Based Services (BH HCBS). For Medicaid Managed Care (MMC), all Medicaid- funded behavioral health services for adults, except for services in Community Residences, are part of the benefit package. Services in Community Residences and the integration of children's behavioral health services will move to Medicaid Managed Care at a later date.
As part of the transition, the New York State Department of Health (DOH) began phasing in enrollment of current MMC enrollees throughout New York State into HARPs beginning with adults 21 and over in New York City in October 2015. This transition expanded to the rest of the State in July 2016. HARPs and HIV Special Needs Plans (HIV SNPs) now provide all covered services available through Medicaid Managed Care.
In Fiscal Year (FY) 2018, New York State engaged in multiple activities to enhance access to behavioral health services and improve quality of care for recipients in Medicaid Managed Care. In June of 2018, HARP became an option on the New York State of Health (Exchange). This enabled 21,000 additional individuals to gain access to the enhanced benefits offered in the HARP product line. The State identified and implemented a policy to allow State Designated Entities to assess and link HARP enrollees to BH HCBS, and allocated quality and infrastructure dollars to MCOs in effo11s to expand and accelerate access to adult BH HCBS. Additionally, the State continually offers ongoing technical assistance to the behavioral health provider community through its collaboration with the Managed Care Technical Assistance Center.
NYS continues to monitor plan-specific data in the three key areas: inpatient denials, outpatient denials, and claims payment. These activities assist with detecting system inadequacies as they occur and allow the State to initiate steps in addressing identified issues as soon as possible.
1. Inpatient Denial Report: Each month, MCOs are required to electronically submit a report to the State on all denials of inpatient behavioral health services based on medical necessity. The report includes aggregated provider level data for service authorization requests and denials, whether the denial was Pre-Service, Concurrent, or Retrospective, and the reason for the denial.
NYS Mental Health (MH) & Substance Use Disorder (SUD) authorization requests and denials for Inpatient (4/1/2021-6/30/2021)1
| Region | Total Authorization | Total Denials (Admin and Medical Necessity) | Utilization Review (Medical Necessity) Denials | Medical Necessity Denial Rate |
|---|---|---|---|---|
| NYC | 37,895 | 354 | 339 | 0.89% |
| ROS | 4,432 | 13 | 11 | 0.25% |
| Total | 42,327 | 367 | 350 | 0.83% |
NOTE: The inpatient data is for three quarters of FY 2020 (10/1/2020-6/30/2021) due to data lag.
NYS Mental Health (MH) & Substance Use Disorder (SUD) authorization requests and denials for Inpatient (10/1/2020-6/30/2021)
| Region | Total Authorization | Total Denials (Admin and Medical Necessity) | Utilization Review (Medical Necessity) Denials | Medical Necessity Denial Rate |
|---|---|---|---|---|
| NYC | 111,194 | 1,151 | 1,122 | 1.01% |
| ROS | 11,600 | 48 | 44 | 0.38% |
| Total | 122,794 | 1,199 | 1,166 | 0.95% |
2. Outpatient Denial Report: MCOs are required to submit on a quarterly basis a report to the State on ambulatory service authorization requests and denials for each behavioral health service. Submissions include counts of denials for specific service authorizations, as well as administrative denials, internal, and fair hearing appeals. In addition, HARPs are required to repo1i authorization requests and denials of BH HCBS.
NYS Mental Health (MH) & Substance Use Disorder (SUD) authorization requests and denials for Outpatient (4/1/2021-6/30/2021)2
| Region | Total Authorization | Total Denials (Admin and Medical Necessity) | Utilization Review (Medical Necessity) Denials | Medical Necessity Denial Rate |
|---|---|---|---|---|
| NYC | 8,300 | 67 | 30 | 0.36% |
| ROS | 1,516 | 23 | 19 | 1.25% |
| Total | 9,816 | 90 | 49 | 0.50% |
Note: HealthFirst data was excluded in this table due to data integrity issue.
NOTE: The outpatient data is for three quarters of FY 2020 (10/1/2020-6/30/2021) due to data lag.
NYS Mental Health (MH) & Substance Use Disorder (SUD) authorization requests and denials for Outpatient (10/1/2020-6/30/2021)
| Region | Total Authorization | Total Denials (Admin and Medical Necessity) | Utilization Review (Medical Necessity) Denials | Medical Necessity Denial Rate |
|---|---|---|---|---|
| NYC | 25,357 | 191 | 100 | 0.39% |
| ROS | 5,002 | 85 | 68 | 1.36% |
| Total | 30,359 | 276 | 168 | 0.55% |
Note: HealthFirst data was excluded in this table due to data integrity issue.
3. Monthly Claims Report: Monthly, MCOs are required to submit the following for all OMH and OASAS licensed and ce1iified services.
Mental Health (MH) & Substance Use Disorder (SUD) Claims (7/1/2021-9/30/2021)
| Region | Total Claims | Paid Claims (Percentage of total claims reported) |
Denied Claims (Percentage of total claims reported) |
|---|---|---|---|
| New York City | 1,084,162 | 91.88% | 8.12% |
| Rest of State | 946,957 | 93.80% | 6.20% |
| Statewide Total | 2,031,119 | 92.78% | 7.22% |
BH Adults HCBS Claims/Encounters 7/1/2021-9/30/2021: NYC
| BH HCBS SERV GROUP | N Claims | N Recip |
|---|---|---|
| CPST | 73 | 21 |
| Education Support Services | 549 | 138 |
| Family Support and Trainings | 32 | 10 |
| Intensive Crisis Respite | 0 | 0 |
| Intensive Supported Employment | 303 | 66 |
| Ongoing Supported Employment | 37 | 6 |
| Peer Support | 2,304 | 480 |
| Pre-vocational | 260 | 46 |
| Provider Travel Supplements | 19 | 15 |
| Psychosocial Rehab | 436 | 76 |
| Residential Supports Services | 388 | 56 |
| Short-term Crisis Respite | 5 | 2 |
| Transitional Employment | 5 | 2 |
| TOTAL | 4,411 | 802 |
Note: Total of N Recip. is by unique recipient, therefore the TOTAL might be smaller than sum of rows.
BH Adults HCBS Claims/Encounters 7/1/2021-9/30/2021: ROS
| BH HCBS SERV GROUP | N Claims | N Recip |
|---|---|---|
| CPST | 932 | 183 |
| Education Support Services | 927 | 268 |
| Family Support and Trainings | 41 | 13 |
| Intensive Crisis Respite | 0 | 0 |
| ntensive Supported Employment | 417 | 102 |
| Ongoing Supported Employment | 84 | 25 |
| Peer Support | 4,824 | 1,075 |
| Pre-vocational | 297 | 77 |
| Provider Travel Supplements | 3,571 | 934 |
| Psychosocial Rehab | 2,476 | 463 |
| Residential Supports Services | 1,957 | 347 |
| Short-term Crisis Respite | 0 | 0 |
| Transitional Employment | 1 | 1 |
| TOTAL | 15,527 | 2,161 |
Note: Total of N Recip. is by unique recipient, therefore the TOTAL might be smaller than sum of rows.
Mental Health (MH) & Substance Use Disorder (SUD) Claims (10/1/2020-9/30/2021)
| Region | Total Claims | Paid Claims (Percentage of total claims reported) |
Denied Claims (Percentage of total claims reported) |
|---|---|---|---|
| New York City | 4,398,809 | 92.22% | 7.78% |
| Rest of State | 3,835,519 | 93.58% | 6.42% |
| Statewide Total | 8,234,328 | 92.84% | 7.16% |
BH Adults HCBS Claims/Encounters 10/1/2020-9/30/2021: NYC
| BH HCBS SERV GROUP | N Claims | N Recip |
|---|---|---|
| CPST | 882 | 63 |
| Education Support Services | 3,982 | 427 |
| Family Support and Trainings | 210 | 20 |
| Intensive Crisis Respite | 0 | 0 |
| Intensive Supported Employment | 2,745 | 275 |
| Ongoing Supported Employment | 234 | 29 |
| Peer Support | 21,195 | 1,138 |
| Pre-vocational | 1,751 | 138 |
| Provider Travel Supplements | 188 | 78 |
| Psychosocial Rehab | 4,189 | 208 |
| Residential Supports Services | 2,587 | 103 |
| Short-term Crisis Respite | 530 | 76 |
| Transitional Employment | 124 | 14 |
| TOTAL | 38,617 | 1,983 |
Note: Total of N Recip. is by unique recipient, therefore the TOTAL might be smaller than sum of rows.
BH Adults HCBS Claims/Encounters 10/1/2020-9/30/2021: ROS
| BH HCBS SERV GROUP | N Claims | N Recip |
|---|---|---|
| CPST | 6,692 | 347 |
| Education Support Services | 7,937 | 760 |
| Family Support and Trainings | 371 | 34 |
| Intensive Crisis Respite | 0 | 0 |
| Intensive Supported Employment | 3,442 | 327 |
| Ongoing Supported Employment | 588 | 70 |
| Peer Support | 37,034 | 2,162 |
| Pre-vocational | 2,372 | 220 |
| Provider Travel Supplements | 16,887 | 1,685 |
| Psychosocial Rehab | 16,496 | 842 |
| Residential Supports Services | 13,304 | 681 |
| Short-term Crisis Respite | 274 | 64 |
| Transitional Employment | 50 | 14 |
| TOTAL | 105,447 | 4,198 |
Note: Total of N Recip. is by unique recipient, therefore the TOTAL might be smaller than sum of rows.
Provider Technical Assistance
Managed Care Technical Assistance Center is a partnership between the McSilver Institute for Poverty Policy and Research at New York University School of Social Work and the National Center on Addiction and Substance Abuse (CASA) at Columbia University, as well as other community and State partners. It provides tools and trainings that assist providers to improve business and clinical practices as they transition to managed care. See below for Managed Care Technical Assistance Statistics.
Quarter 4 MCTAC Attendance & Stats (7/1/2021 to 9/30/2021)
Events: MCTAC successfully executed 14 events from 7/1/2021 to 9/30/2021
All 14 were held via webinar.
Individual Participation: 603 people attended/participated in MCTAC events of which 464 are unique participants.
OMH Agency Participation
Overall: 161 of 635 (25.35%)
NYC: 121 of 331 (36.56%)
ROS: 135 of 434 (31.11%)
OASAS Agency Participation
Overall: 115 of 547 (21.02%)
NYC: 64 of 240 (26.67%)
ROS: 84 of 379 (22.16%)
MCTAC Attendance & Stats Annual Report (10/1/2020 to 9/30/2021)
Events: MCTAC successfully executed 90 events from 10/1/2020 to 9/30/2021
All 90 were held via webinar.
Individual Participation: 5,476 people attended/participated in MCTAC events of which 2,623 are unique participants.
OMH Agency Participation
Overall: 467 of 635 (73.54%)
NYC: 254 of 331 (76.74%)
ROS: 327 of 434 (75.35%)
OASAS Agency Participation
Overall: 352 of 547 (64.35%)
NYC: 157 of 240 (65.42%)
ROS: 260 of 379 (68.60%)
Efforts to Improve Access to Behavioral Health Home and Community Based Services (BH HCBS)
All HARP enrollees are eligible for individualized care management. In addition, Behavioral Health Home and Community Based Services (BH HCBS) were made available to eligible HARP and HIV SNP enrollees. These services were designed to provide enrollees with specialized supports to remain in the community and assist with rehabilitation and recovery. Enrollees were required to undergo an assessment to determine BH HCBS eligibility. Effective January 2016 in NYC and October 2016 for the rest of the state, BH HCBS were made available to eligible individuals.
As discussed with CMS, New York experienced slower than anticipated access to BH HCBS for HARP members and actively sought to determine the root cause for this delay. Following implementation of BH HCBS, the State and key stakeholders identified challenges, including: difficulty with enrolling HARP members in Health Homes (HH); locating enrollees and keeping them engaged throughout the lengthy assessment and Plan of Care development process; ensuring care managers have understanding of BH HCBS (including person-centered care planning) and capacity for care managers to effectively link members to rehab services; and difficulty launching BH HCBS due to low number of referrals to BH HCBS providers.
The State previously made efforts to ramp up utilization and improve access to BH HCBS by addressing the challenges identified. These efforts included:
- Streamlining the BH HCBS assessment process
- Effective March 7, 2017, the full portion of the New York State Community Mental Health assessment is no longer required. Only the brief portion (NYS Eligibility Assessment) is required to establish BH HCBS eligibility and provide access to these services.
- Developed training for care managers and BH HCBS providers to enhance the quality and utilization of integrated, person-centered plans of care and service provision, including developing a Health Home training guide for key core competency trainings to serving the high need SMI population.
- BH HCBS Performance - fine-tuned MCO Reporting template to improve Performance Dashboard data for the BH HCBS workflow (Nov 2018, streamlining data collection for both HH and RCAs).
- Developed required training for BH HCBS providers that the State can track in a Learning Management System.
- Implementing rates that recognize low volume during implementation to help providers ramp up to sustainable volumes.
- Enhancing Technical Assistance efforts for BH HCBS providers including workforce development and training.
- Obtained approval from CMS to provide recovery coordination services (assessments and care planning) for enrollees who are not enrolled in HH. These services are provided by State Designated Entities (SDE) through direct contracts with the MCO.
- Developed and implemented guidance to MCOs for contracting with State- designated entities to provide recovery coordination of BH HCBS for those not enrolled in Health Home.
- Developed Documentation and Claiming guidance for MCOs and contracted Recovery Coordination Agencies (RCA) for the provision of assessments and development of plans of care for BH HCBS.
- Additional efforts to support initial implementation of RCAs include
- In-person trainings (completed June 2018)
- Weekly calls with MCOs
- Ongoing technical assistance.
- Creation of statewide RCA performance dashboard-enhanced to reflect data by RCA and by HH
- Continuing efforts to increase HARP enrollment in HH including:
- Best practices for embedded care managers in ERs, Clinics, shelters, CPEPS and Inpatient units and engagement and retention strategies
- Existing quality improvement initiative within clinics to encourage HH enrollment
- Emphasis on warm hand-off to Health Home from ER and inpatient settings
- PSYCKES quality initiatives incentivizing MCOs to improve successful enrollment of high-need members in care management
- DOH approval of MCO plans for incentivizing enrollment into HH (e.g., Outreach Optimization)
- Ongoing work to strengthen the capacity of HH to serve high need SMI individuals and ensure their engagement in needed services through expansion of Health Home Plus (HH+) effective May 2018.
- Provided technical assistance to lead HHs and representation on new HH+ Subcommittee Workgroup
- Implementing Performance Management efforts, including developing enhanced oversight process for Health Homes who have not reached identified performance targets for and key quality metrics for access to BH HCBS for HARP members
- Disseminating Consumer Education materials to improve understanding of the benefits of BH HCBS and educating peer advocates to perform outreach.
- NYS Office of Mental Health has contracted with NYAPRS to conduct peer-focused outreach and training to possible eligible members for Medicaid Managed Care Health and Recovery Plans (HARPs) and Adult Behavioral Health (BH) Home and Community Based Services (BH HCBS).
- NYAPRS conducts outreach in two ways:
- Through 45-90-minute training presentations delivered by peers
- OMH approves the PowerPoint before significant changes are made
- Through direct one-to-one outreach in community spaces (such as in homeless shelters or on the street near community centers)
- Through 45-90-minute training presentations delivered by peers
- NYAPRS conducts outreach in two ways:
- NYS Office of Mental Health has contracted with NYAPRS to conduct peer-focused outreach and training to possible eligible members for Medicaid Managed Care Health and Recovery Plans (HARPs) and Adult Behavioral Health (BH) Home and Community Based Services (BH HCBS).
- Implemented Quality and Infrastructure initiative to support targeted BH HCBS workflow processes and increase in BH HCBS utilization. In-person trainings completed June 2018. The State has worked with the Managed Care Plans on an ongoing basis to further monitor and operationalize this program and increase access and utilization of BH HCBS. Infrastructure contracts have been signed and work is underway.
- 13 HARPs distributed over $34 million through 95 provider contracts to support the focused and streamlined administration of BH HCBS, including coordination of supports from assessment to service provision.
- Outreach to all MCOs was conducted to discuss best practices identified through the use of Quality and Infrastructure initiative funds that resulted in an increase of members utilizing BH HCBS; the State also shared a summary of best and promising practices with MCOs.
- Issued Terms and Conditions for BH HCBS Providers to standardize compliance and quality expectations of BH HCBS provider network and help clarify for MCOs which BH HCBS Providers are actively providing services.
- Enhancing State Adult BH HCBS Provider oversight including development of oversight tools and clarifying service standards for BH HCBS provider site reviews, including review of charts, interviews with staff or clients and review of policy and procedures.
- Worked with the HARP/BH HCBS Subcommittee (2017-2019) - consisting of representatives from MCOs, HHs, CMAs, and BH HCBS Provider agencies - which developed and provided a variety of tools to support care manager referrals to BH HCBS, on behalf of NYS' HH/MCO Workgroup.
- A process for care managers and supervisors to apply for a waiver of staff qualifications for administering the NYS Eligibility Assessments was established, in response to challenges in securing a CM workforce meeting both the education and experience criteria and need for more assessors.
To date, 4,977 care managers in NYS have completed the required training for conducting the NYS Eligibility Assessment for BH HCBS. Also, between July 1, 2021 and September30, 2021 5,229 eligibility assessments were completed. For the period between October1, 2020 and September 30, 2021 23,983 eligibility assessments were completed.
Despite extensive efforts outlined above and stakeholder participation to implement strategies for improved utilization of BH HCBS, the number of HARP enrollees successfully engaged with BH HCBS overall remain very low. NYS reviewed a significant amount of feedback from MCOs, Health Homes, Care Managers and other key stakeholders and determined the requirements for accessing BH HCBS were too difficult to standardize among 15 MCOs and 30 Health Homes.
As a result, the State released a draft proposal for public comment in June 2020 to transition 1115 Waiver BH HCBS into a State Adult Rehabilitation Services package for HARP enrollees and HARP eligible HIV-SNP enrollees, which to date has resulted in positive feedback. The State finalized the proposal and submitted to CMS in September 2020. The objectives of this transition are two-fold: to simplify and allow creativity in service delivery of community-based rehabilitation services tailored to the specific needs of the behavioral health population, and to eliminate barriers to access.
To receive the enhanced Federal Medical Assistance Percentage (eFMAP) available through the American Rescue Plan Act, the State revised the September 2020 proposal to comply with the eFMAP requirements and resubmitted to CMS in July 2021. CMS approved NYS's 1115 Waiver Amendment Request for Community Oriented Recovery and Empowerment (CORE) Services on October 5, 2021. CORE Services is a rehabilitation and recovery service array which includes four services previously available through BH HCBS: Psychosocial Rehabilitation (PSR), Community Psychiatric Support and Treatment (CPST), Family Support and Training (FST), and Empowerment Services - Peer Support (Peer Support).
Access to these CORE Services will no longer require an independent eligibility assessment, will remove settings restrictions, and will enable all HARP and HARP eligible HIV-SNP enrollees to access services with a recommendation from a licensed practitioner of the healing arts (LPHA). Enrollment in Health Home Care Management will continue to be an important piece of the HARP benefit package for the comprehensive, integrated coordination of the care offered by Health Home. Care managers will always have the important role of ensuring timely access to services reflective of the member's preferences and individual needs, in continued collaboration with the MCO and service providers.
The State will implement CORE Services over several months, with go-live targeted for February 1, 2022. Transition planning is underway, and the State is providing ongoing opportunities for stakeholder input through multiple forums. The State is developing consumer education materials and targeted trainings and technical assistance for providers, MCOs, and other stakeholders impacted by this transition.
Habilitation, Education Support Services, Pre-Vocational Services, Transitional Employment, Intensive Supported Employment, and Non-Medical Transportation remain in the BH HCBS benefit package. The State will continue its efforts to increase access to these services through working collaboratively with Health Homes.
In addition, the State is planning to extend the Infrastructure initiative to support the behavioral health providers transitioning the four services moving from BH HCBS to the new CORE Service array and continuing support of BH HCBS providers. OMH and OASAS are writing guidance for an Infrastructure Program Extension which will allow MCOs to contract for remaining, unspent funds totaling approximately $31M.
Transition of School-based Health Center (SBHC) Services from Medicaid Fee-for-Service to Medicaid Managed Care (MMC):
Quarter 4: No activity to report during this quarter. The transition of SBHC services from Medicaid Fee-for-Service to MMC has been moved to 2023. Additional information about the transition can be found here.
Annual:
Quarter 1: The Department resumed the Gap Report focus group calls in October and November 2020. Currently, this focus group consists of four MMC plans, and six SBHCs. As previously mentioned, the goal of this Gap Report Pilot focus group is to test the data exchange process for participating SBHCs to share student rosters with all contracted MMC plans. These calls provide the opportunity for the MMC plans and SBHCs participating in the pilot to discuss successes and barriers which have been identified during the data exchanges between the MMC plan and the SBHC. The Department is planning to compile best practices from the feedback from this focus group. A copy of the gap report template, instructions, and additional information about the transition can be found here.
Quarter 2: In response to competing priorities due to the COVID-19 public health emergency, the Gap Report focus group calls are currently on hold. The Department would like to take more time to reflect on where we are and review the feedback the Department has received so far to re- evaluate next steps for the pilot and the transition at large. The Department is planning to compile best practices from the feedback from this focus group and disseminate these findings to the larger stakeholder group. Additional information about the transition can be found here.
Quarter 3: A Gap Report Pilot Closeout meeting was held on June 3, 2021, this focus group consists of four MMC plans, and six SBHCs. The agenda included a summary of MMC plan/SBHC date exchange details, pilot takeaways, and best practices. The Department plans to hold a full SBHC Stakeholder Workgroup meeting in the future to discuss best practices and next steps. The transition of SBHC services from Medicaid Fee-for-Service to MMC has been moved to 2023. Additional information about the transition can be found here.
C. Managed Long-Term Care Program (MLTCP)
Managed Long-Term Care plans include Partial Capitation, Program for the All-Inclusive Care of the Elderly (PACE), Medicaid Advantage Plus (MAP), Medicaid Advantage (MA), and Fully Integrated Duals Advantage for individuals with Intellectual and Developmental Disabilities (FIDA-IDD) plans. As of October 1, 2021, there are 25 Partial Capitation plans, 9 PACE plans, 12 MAP, 3 MA plans, and 1 FIDA IDD plan. As of October 1, 2021, there are a total of 285,060 members enrolled across all MLTC products.
1. Accomplishments/Updates
During the July 2021 through September 2021 quarter, 1 new MAP plan began operations.
During the annual period of October 2020 through September 2021, the Department of Health (Department) approved service area expansions for 1 PACE plan, 1 MAP plan, and 1 MA plan. During that same annual period, the Department approved the opening of 3 new MAP plans.
New York's Enrollment Broker, NYMC, conducts the MLTC Post Enrollment Outreach Survey which contains questions specifically designed to measure the degree to which consumers could maintain their relationship with the services they were receiving prior to mandatory transitions to MLTC. For the July 2021 through September quarter, post enrollment surveys were completed for 6 enrollees. Of the 5 who responded to the question, all of them (100%) indicated that they continued to receive services from the same caregivers once they became members of an MLTCP (1 enrollee did not respond to this question). The percentage of affirmative responses is consistent with the previous quarter.
Enrollment: Total enrollment in MLTC partial capitation plans increased from 242,961 to 244,809 during the July 2021 through September 2021 quarter, a slight increase from the last quarter. For that period, 8,676 individuals who were being transitioned into Managed Long Term Care made an affirmative choice, a 10% decrease from the previous quarter and brings the 12-month total for affirmative choice to 40,277.
Monthly plan-specific enrollment for Partial Capitation plans, PACE plans, MAP plans, MA plans, and FIDA IDD plans during the October 2020 through September 2021 annual period is submitted as an attachment.
2. Significant Program Developments
During the July 2021 through September 2021 quarter:
- The 3rd quarter Member Services survey was conducted on 26 Partial Capitation Plans and 12 MAP Plans. This survey was intended to provide feedback on the overall functioning of the plans' member service performance. No response was required, but, when necessary, the department provided recommendations on areas of improvement;
- The Desk Review for 4 Partial Capitation Operational Surveys have been completed. Corrective Action Plans (CAP) have been completed by the plans and are awaiting department approval;
- 2 Operational Surveys are ongoing on Partial Capitation plans;
- A Focused Survey was conducted on 25 Partial Capitation and MAP plans targeting Social Day Care management practices during the 2nd quarter. The requested data has been received and is being analyzed;
- A Focused Survey was conducted on 1 MAP plan targeting MAP appeal notices during the 1st quarter. A Statement of Deficiencies was issued, and the CAP is under review;
- A Focused Survey was conducted on 1 Partial Capitation plan based on a TAC Complaint during the 1st quarter. A Statement of Deficiencies was issued, and the plan has submitted an unacceptable CAP. An appropriate CAP was requested and is due 11/1/2021;
- A Focused Survey was conducted on 1 Partial Capitation plan based on a TAC Complaint during the 2nd quarter. A Statement of Deficiencies was issued, and the CAP is under review; and
- A Focused Survey was conducted on 25 Partial Capitation and 12 MAP Plans focusing on Internal Appeal and Fair Hearing management practices. A review of plan files is still being conducted.
As a matter of routine course:
- Processes for Operational Partial Capitation and MAP surveys continue to be refined;
- The Surveillance tools continue to be updated to reflect process changes; and
- Reports have been developed/implemented to assist with summarizing survey findings.
In addition to the fourth quarter activities discussed above, below is a summary of other activities that have occurred during the October 2020 through September 2021 annual period:
- The COVID Pandemic temporarily halted Surveillance Activity from March 2020 - July 2020 and has resulted in extended response times from the plans.
- Three (3) Complaint Investigation Surveys were completed. These surveys assessed the plan's compliance with its Medicaid contract based on complaints received in the TAC unit.
3. Issues and Problems
There were no issues or problems to report for the July 2021 through September 2021 quarter, nor for the October 2020 through September 2021 annual period.
4. Summary of Self-Directed Options
Self-direction is provided within the MLTCP as a consumer choice and gives individuals and families greater control over services received. The Department published a Request for Offers in December 2019 to procure fiscal intermediary (FI) administrative services for the Consumer Directed Personal Assistance Program (CDPAP). After award and a transition process, only entities that have contracts with the Department may provide FI administrative services. Managed care plans will enter into separate administrative service agreements with Department-contracted FIs.
5. Required Quarterly Reporting
Unless otherwise noted, changes from last quarter are presumed to be due to COVID-19 pandemic.
Critical incidents: There were 1,409 critical incidents reported for the July 2021 through September 2021 quarter, a decrease of 3% from the previous quarter. The names of plans reporting no critical incidents are shared with the surveillance unit for follow up on survey. To date, none of those plans were found to have had critical incidents that should have been reported. Critical incidents by plan for this quarter are attached.
For the annual period October 2020 through September 2021, critical incidents decreased by 5% from the previous annual period.
Complaints and Appeals: For the July 2021 through September 2021 quarter, the top reasons for complaints/appeals changed from last quarter: Dissatisfaction With Transportation, Dissatisfaction With Quality Of Other Covered Services, Dissatisfaction With Quality of Homecare, Homecare Aide Late/Absent, Dissatisfaction With Choices of Providers In Network.
| Period: 7/1/2021 through 9/30/2021 (Percentages rounded to nearest whole number) |
|||
|---|---|---|---|
| Number of Recipients: 279,060 | Complaints | Resolved | Percent Resolved * |
| # Expedited | 26 | 18 | 69% |
| # Same Day | 3,085 | 3,085 | 100% |
| # Standard/Expedited | 11,044 | 10,475 | 95% |
| Total for this period: | 14,155 | 13,578 | 96% |
*Percent Resolved includes grievancesed during previous quarters that are resolved during the current quarter, that may result in creating a percentage greater than 100.
| Appeals | 10/2020-12/2020 | 1/2021-3/2021 | 4/2021-6/2021 | 7/2021-9/2021 | Average for Four Quarters |
|---|---|---|---|---|---|
| Average Enrollment | 270,539 | 274,366 | 275,540 | 279,060 | 274,876 |
| Total Appeals | 7,934 | 7,948 | 8,957 | 8,424 | 8,316 |
| Appeals per 1,000 | 29 | 29 | 32 | 30 | 30 |
| # Decided in favor of Enrollee | 1,101 | 923 | 1,088 | 1,496 | 1,152 |
| # Decided against Enrollee | 5,906 | 5,909 | 6,820 | 6,168 | 6,201 |
| # Not decided fully in favor of Enrollee | 604 | 575 | 652 | 612 | 611 |
| # Withdrawn by Enrollee | 204 | 206 | 288 | 231 | 232 |
| # Still pending | 544 | 766 | 118 | 886 | 579 |
| Average number of days from receipt to decision | 9 | 8 | 7 | 8 | 8 |
| Complaints and Appeals per 1,000 Enrollees by Product Type July 2021 - September 2021 | |||||
|---|---|---|---|---|---|
| Enrollment | Total Complaints | Complaints per 1,000 | Total Appeals | Appeals per 1,000 | |
| Partial Capitation Plan Total | 244,075 | 8,558 | 35 | 6,591 | 27 |
| Medicaid Advantage Plus (MAP) Total | 29,565 | 4,340 | 147 | 1,731 | 59 |
| PACE Total | 5,420 | 1,257 | 232 | 102 | 19 |
| Total for All Products: | 279,060 | 14,155 | 51 | 8,424 | 30 |
Total complaints decreased 2% from 14,396 the previous quarter to 14,155 during the July 2021 through September 2021 quarter.
The total number of appeals decreased 6% from 8,957 during the last quarter to 8,424 during the July 2021 through September 2021 quarter.
For the annual period October 2020 through September 2021, the number of complaints decreased by 12%, and the number of appeals increased by 3%.
Technical Assistance Center (TAC) Activity
During the July 2021 through September 2021 quarter, TAC opened 536 cases. This roughly the same as the previous quarter. TAC has seen a slight increase in substantiated cases. Many of these are due to plan's failing to canvas for vendors when there is a provider staffing shortage.
TAC continues to take the most cases for complaints against aide service, and there has been an increase since the previous quarter. Provider staffing issues continue to be the biggest trend for TAC.
| Call Volume | 7/1/2021-9/30/2021 |
|---|---|
| Call Volume | 7/1/2021- 9/30/2021 |
| Substantiated Complaints | 36 |
| Unsubstantiated Complaints | 311 |
| Closed As Duplicate | 2 |
| Resolved Without Investigation | 10 |
| Inquiries | 195 |
| Total | 554 |
The five most common types of calls were related to:
| Q4 2021 | 7/1/2021-9/30/2021 |
|---|---|
| Aide Service | 31% |
| General | 23% |
| Enrollment | 10% |
| Billing | 9% |
| Grievance | 8% |
63% of Q4 TAC cases are closed in the same month they are opened. This is up 11% from last quarter. This is most likely due to staffing and workflow improvements. Overall, TAC's complaint numbers have remained consistent when compared to the previous quarter. TAC continues to help members navigate through the changes and trends stemming from the public health emergency.
During the annual period from October 2020 through September 2021, TAC opened 2,095 cases. This is less than the previous year. TAC has seen a decrease in general questions and inquires over the past year. This decrease was anticipated as there was a spike in general questions at the beginning of the public health emergency.
TAC continues to take the most cases for complaints against aide service, and there was a 7% increase over the past year. This increase is most likely due to the home health aide shortage TAC has seen across the state. The rest of the common complaint categories have stayed about the same.
| Call Volume | 10/1/2020-9/30/2021 |
|---|---|
| Substantiated Complaints | 196 |
| Unsubstantiated Complaints | 1,074 |
| Closed As Duplicate | 3 |
| Resolved Without Investigation | 66 |
| Inquiries | 799 |
| Total | 2,139 |
The five most common types of calls were related to:
| Types of Calls | 10/1/2020-9/30/2021 |
|---|---|
| Aide Service | 27% |
| General | 20% |
| Enrollment | 11% |
| Billing | 11% |
| Grievance | 10% |
During the annual period from October 2020 through September 2021, the TAC Unit took in a total of 2,095 cases and resolved 2,139 cases. The TAC unit closed more cases than were opened due to rollover from last year. Due to issues surrounding the public health emergency, the TAC unit is finding that cases are staying open longer than usual.
60% of TAC cases are closed in the same month they are opened. This is down 2% from last year. This is mostly due to issues during the public health emergency. The TAC unit has also seen a 19% increase in efficiency since July. This is most likely due to staffing and workflow improvements.
TAC's complaint numbers have remained consistent when compared to the previous year. Though there has been an increase in COVID-19-related calls, TAC has also noticed a decrease in other types of complaints. Specifically, the TAC unit has seen an increase in inquiries and a decrease in unsubstantiated cases.
Evaluations for enrollment: The Conflict Free Evaluation and Enrollment Center (CFEEC) operations were fully implemented statewide by June 30, 2015. For July 2021 through September 2021 quarter, 7,165 people were evaluated, deemed eligible and enrolled into plans, a decrease of 12% from the previous quarter. This brings the total for the annual period October 2020 through September 2021 to 32,989.
Referrals and 30-day assessment: For the July 2021 through September 2021 quarter, MLTC plans conducted 24,864 assessments, a 6% decrease from 26,521 the previous quarter. The total number of assessments conducted within 30 days decreased 8% from 20,898 the previous quarter to 19,143 this quarter.
During the annual period October 2020 through September 2021, a total of 114,903 assessments were completed, with 74% of those assessments being conducted within 30 days of the request, which remains consistent with the previous annual period. The Department continues to monitor data collection, evaluation and reporting of CFEEC activity.
Referrals outside enrollment broker: For the July 2021 through September 2021 quarter, the number of people who were not referred by the enrollment broker and who contacted the plan directly was 22,145, a 5% decrease from 23,358 the previous quarter. The annual period October 2020 through September 2021 saw a decrease totaling 16% by the end of the year, compared to the decrease from the previous annual period (33%).
| Rebalancing Efforts | 7/2021-9/2021 |
|---|---|
| Enrollees who joined the plan as part of their community discharge plan and returned to the community this quarter | 165 |
| Plan enrollees who are or have been admitted to a nursing home for any length of stay and who return to the community | 2,086 |
| Individuals who are permanently placed in a nursing home and are new to plan | 235 |
As of September 30, 2021, there were 3,744 current plan enrollees who were in nursing homes as permanent placements, a 3% decrease from the previous quarter.
D. Children's Waiver
On August 2, 2021, CMS approved the Children's 1115 Waiver, with the goal of creating a streamlined model of care for children and youth under 21 years of age with behavioral health (BH) and Home and Community Based Service (HCBS) needs, including medically fragile children, children with a BH diagnosis, children with medical fragility and developmental disabilities, and children in foster care with developmental disabilities, by allowing managed care authority for their HCBS.
Specifically, the Children's 1115 Waiver provides the following:
- Managed care authority for HCBS provided to medically fragile children in foster care and/or with developmental disabilities and children with a serious emotional disturbance;
- Authority to include current Fee for Service HCBS authorized under the State's newly consolidated 1915c children's waiver in Medicaid Managed Care benefit packages;
- Authority to mandatorily enroll into managed care the children receiving HCBS via the 1915c Children's waiver;
- Authority to waive deeming of income and resources, if applicable, for all medically needy “Family of One” children (Fo1 children) who will lose their Medicaid eligibility as a result of them no longer receiving at least one 1915c service due to case management now being covered outside of the 1915c children's waiver, including non-Supplemental Security Income Fo1 children. The children will be targeted for Medicaid eligibility based on risk factors and institutional level of care and needs;
- Authority to institute an enrollment cap for Fo1 children who attain Medicaid eligibility via the 1115; and
- Authority to provide customized goods and services, such as self- direction and financial management services, that are currently approved under the demonstration's HARP's pilot to Fo1 children.
- Authority for Health Home care management monthly monitoring as an HCBS
- Removes managed care exclusion of children placed with Voluntary Foster Care Agencies
Given the approval, the New York State Department of Health has been engaged in implementation activities, including, but not limited to the following:
- Receiving approval from CMS for the Children's 1115 Evaluation Design as of April 16, 2020;
- Continuing to refine data collection and data analysis to ensure accurate reporting;
- Engaging a contract vendor for performance and quality monitoring for all elements of the Children's Redesign, including the Children's 1115 Waiver, to ensure consistency and quality in all elements of the initiative;
- Submitting the Preliminary Interim Evaluation Report to CMS, as drafted by the vendor;
- Submitting the Interim Evaluation Report to CMS, as drafted by the vendor;
- Drafting policies and guidance to ensure compliance with State and federal requirements - as well as working with service providers to confirm understanding and compliance with requirements such as the CMS HCBS Settings Final Rule and Electronic Visitor Verification;
- Conducting refresher training sessions and offering more in-depth training for care managers and HCBS providers - including additional resources and technical assistance with person-centered planning;
- Facilitating relationship building between Managed Care Organizations, HCBS providers, and care managers to improve communication and care coordination;
- Coordinating stakeholder meetings to obtain feedback from Managed Care Organizations, Health Homes, HCBS providers, advocate groups, regional Planning Consortiums, and others regarding the Medicaid Redesign and implementation;
- Evaluating accuracy of Managed Care Organizations and Fee-for-Service billing and claiming data;
- Defining performance and quality metrics;
- Responding to the COVID-19 pandemic and implementing emergency 1135 and Appendix K, inclusive of a Retainer Payment for Day and Community Habilitation providers - and continuing to support the recovery of impacted providers and consumers;
- Conducting case reviews;
- Working with Health Homes and HCBS providers to enhance capacity monitoring and streamline the referral process;
- Engaging with providers to understand barriers to service delivery - such as work force challenges, lack of referral sources / lack of service awareness, travel time for families in rural areas, etc. - and solutions to address these concerns, including the development of a state-wide capacity tracking system, which is currently underway;
- Engaging with providers, consumers, and New York State agencies partners to determine how best to use the enhanced FMAP authorized by the American Rescue Act to improve access to children's services and reduce administrative burden on providers; and
- Collecting stakeholder feedback (from consumers, HCBS providers, Health Homes, Managed Care Organizations, and advocate groups) to inform the 1915(c) Children's Waiver renewal - including suggestions on how to streamline the Managed Care processes and improve communication between Managed Care Organizations, Health Homes, and HCBS providers.
The above-listed activities will help to facilitate oversight and the provision of high-quality services, ensure that the goals of the Children's 1115 Waiver are achieved, and provide the necessary data elements to fulfill future reporting requirements.
The following table demonstrated the number of children enrolled in the 1915(c) Children's Waiver identified by NYS restriction exception (RE) code of K1 and the current claims for services for these enrolled children. Additionally, as outlined in the 1115 amendment, NYS is tracking the enrollment of children/youth who obtained Medicaid through "Family of One" Medicaid budgeting as identified by NYS restriction exception (RE) code KK. Therefore, the table below also demonstrates the number of children enrolled with this KK flag and the current claims for services for these enrolled children.
| Month | With K1 Flag - HCBS LOC | With KK Flag - Family of One | ||
|---|---|---|---|---|
| Enrolled Children | Enrolled Children w/HCBS Claims | Enrolled Children | Enrolled Children w/HCBS Claims | |
| Jul | 8,689 | 3,320 | 4,784 | 306 |
| Aug | 8,941 | 2,944 | 4,838 | 310 |
| Sep | 9,032 | 1,259 | 4,858 | 183 |
| Qrtly Avg. | 8,887 | 2,508 | 4,827 | 266 |
| Annual Average | 7,808 | 2,542 | 4,499 | 247 |
This table includes data from the 4th Quarter of FY2021; however, the data from July and August is still within the 90-day claim lag period. Data from this quarter continues to be impacted by the COVID-19 pandemic, which likely resulted in significantly decreased utilization and/or claiming, although this trend is improving, and utilization of these services is increasing. The annual average is also included in this table for FY2021 (October 2020 through September 2021). For the 4th Quarter, the Children's Waiver enrollment is above the annual average and enrolled children with HCBS claims are slightly below the annual average (which is likely due to the claims lag). This data will continue to be reviewed in relation to the claim lag, and data will continue to be analyzed to understand the impact of the pandemic, especially in relation to utilization.
____________________________________________
1. Q4 data is not available and will be submitted with the next quarterly update. 1
2. Q4 data is not available and will be submitted with the next quarterly update. 2
VI. Evaluation of the Demonstration
During this quarter ending June 30, 2021, five Independent Evaluations are in process. The first Independent Evaluation (IE) that is coming to conclusion is the DSRIP Independent Evaluation activity. This five-year analysis and DSRIP IE contract has been conducted by SUNY Albany School of Public Health Research Foundation. The DSRIP Draft Summative Evaluation Report was submitted to CMS on March 23, 2021. CMS returned the DSRIP Draft Summative Evaluation report with comments on July 13, 2021, with a return date of August 12, 2021. The
DSRIP Final Summative Evaluation Report along with responses to CMS comments on the Draft Summative Evaluation report were submitted to CMS on August 10, 2021. The DSRIP IE and DOH are eager to receive CMS approval on the Final Summative Evaluation.
Activities have also continued in parallel for the four additional Independent Evaluations (IE) supported by each of the RAND Corporation research teams. RAND has contracts to conduct each of the Independent Evaluations including the Children's waiver, the 1115 waiver, the Health and Recovery Program (HARP) and the Self-Directed Care (SDC) pilot program. The goals and deliverables for these four IE activities are for each RAND team to produce an Interim Evaluation report for each of the waiver programs per the CMS approved evaluation design plans.
On March 16, 2021 the RAND team conducting the Independent Evaluation of the 1115 Demonstration Waiver provided a full draft Interim Evaluation report to NYS for review. The draft report contained updated county enrollment findings on the Domain 1 research question related to Component 1 Managed Long Term Care enrollment and provided preliminary findings for the ten research questions related to the Domain 2 Component, to Limit Gaps in Continuous Enrollment. Previous findings for Domain 1 Component 2, Individuals Moving from Institutional to Community Based Settings in need of Long-Term Services and Supports, remain unchanged as reflected in the Preliminary Evaluation report shared with CMS in December 2020.
Those preliminary findings for both Domain 1 updates and all of Domain 2 were reviewed and discussed with NYS Department of Health staff in the Office of Health Insurance Programs (OHIP), Office of Quality and Patient Safety (OQPS), Division of Eligibility and Marketplace Innovations (DEMI), the Division of Health Plan Contracting and Oversight (DHPCO), and the Division of Operations and Systems (DOS). Comments were returned to RAND on March 30, 2021. RAND addressed those questions and submitted an updated version 3 full draft of the Interim Evaluation report to NYS reviewers last quarter. After all internal reviews concluded, the 1115 Interim Evaluation report for all 22 research questions was submitted to CMS on August 4, 2021. CMS returned the 1115 Interim Evaluation report with comments on September 10, 2021. CMS also requested clarity on the availability of individual-level data which was discussed further on the September 20, 2021 Monitoring Call with CMS and DOH.
In February 2021, the Heath and Recovery Program (HARP) and Self-Directed (SDC) pilot program teams at RAND gained access to all data tables for all 17 HARP and 13 SDC research questions. During this quarter, RAND also conducted and concluded all qualitative interviews with stakeholders, agencies, and beneficiaries and will begin integrating analysis of both qualitative and quantitative findings were appropriate. Staff from the Office of Health Insurance Programs (OHIP), Office of Quality and Patient Safety (OQPS), Office of Mental Health (OMH), Office of Addiction Services and Supports (OASAS) and the Division of Operations and Systems (DOS) continue to assist the RAND researchers weekly with HARP and SDC questions on data limitations and analysis. During this quarter, this RAND contract was also extended an additional year through February 11, 2022 to finalize all HARP and SDC Pilot Interim Evaluation activities. All data access and data use agreements were also extended in parallel through February 11, 2022. The contract extension was necessary due to the early impacts, last
Spring and Summer 2020, when resources were reprioritized to address the NYS COVID-19 pandemic. Thus, this IE team's implementation activities for RAND were delayed and timelines have been updated. The RAND team is currently at the phase of data analysis and interpretation for each HARP and SDC research question. The HARP and SDC Pilots will have separate draft Interim Evaluation reports prepared for review to NYS.
During February and March 2021, the RAND team conducting the Independent Evaluation of the Children's Waiver submitted a preliminary draft of the required Interim Evaluation report for NYS review and approval. This Interim Evaluation report included preliminary findings on the 7 required interim research questions related to the Children's waiver. Six remaining research questions will be addressed in the future Summative Evaluation for the Children's waiver per the STC requirements. The Interim Evaluation report for the Children's Wavier was submitted to CMS on July 27, 2021. CMS did not have any further comment on the report.
VII. Consumer Issues
A. MMC, HARP and HIV SNP Plan Reported Complaints
Medicaid Managed Care Organizations (MCOs), including Medicaid Managed Care (MMC) plans, Health and Recovery Plans (HARPs), and HIV Special Needs Plans (HIV SNPs) are required to report quarterly to the Department of Health on the number and type of enrollee complaints/action appeals that they received. MCOs are also required to report on the number and type of complaints that they received regarding enrollees who are in receipt of SSI.
The following table outlines the complaints MCOs reported by category for the most recent quarter and for the last four (4) quarters:
| MCO Product Line | Total Complaints | |
|---|---|---|
| FFY 21 Q4 7/1/2021-9/30/2021 | Last 4 Quarters 10/1/2020-9/30/2021 | |
| MMC | 7,380 | 30,508 |
| HARP | 934 | 3,573 |
| HIV SNP | 112 | 480 |
| Total MMCO Complaints | 8,426 | 34,561 |
As described in the table, total MCO enrollee complaints reported for the current quarter total 8,426. This represents a 1.3% increase from the prior quarter's total of 8,315.
This quarter's MCO complaints show an increase of 1.2% for MMCs from the previous quarter's total of 7,294. HARPs show a 3.0% increase in complaints since the prior quarter, which totaled 906. This quarter's HIV SNP complaints saw a decrease of 2.6% when compared to the previous quarter's total of 115.
The following table outlines the top five (5) most frequent categories of complaints reported for MMCs, HARPs, and HIV SNPs, combined, for the most recent quarter and for the last four (4) quarters:
| Description of Complaint | Percentage of Complaints | |
|---|---|---|
| FFY 21 Q4 7/1/2021-9/30/2021 |
Last 4 Quarters 10/1/2020-9/30/2021 |
|
| Dissatisfied with Provider Services (Non-Medical) or MCO Services | 14% | 17% |
| Reimbursement/Billing | 14% | 13% |
| Pharmacy/Formulary | 11% | 8% |
| Balance Billing | 10% | 15% |
| Dissatisfied with Quality of Care | 9% | 8% |
The following table outlines the top five (5) most frequent categories of complaints reported for HARPs for the most recent quarter and the last four (4) quarters:
| Description of Complaint | Percentage of Complaints | |
|---|---|---|
| FFY 21 Q4 7/1/2021-9/30/2021 |
Last 4 Quarters 10/1/2020-9/30/2021 |
|
| Dissatisfied with Provider Services (Non-Medical) or MCO Services | 21% | 25% |
| Dissatisfaction with Quality of Care | 12% | 11% |
| Pharmacy/Formulary | 12% | 10% |
| Difficulty with Obtaining: Specialist and Hospitals | 9% | 5% |
| Difficulty with Obtaining: Dental/Orthodontia | 8% | 8% |
The following table outlines the top five (5) most frequent categories of complaints reported for HIV SNPs for the most recent quarter and the last four (4) quarters:
| Description of Complaint | Percentage of Complaints | |
|---|---|---|
| FFY 21 Q4 7/1/2021-9/30/2021 | Last 4 Quarters 10/1/2020-9/30/2021 | |
| Pharmacy/Formulary | 27% | 19% |
| Dissatisfied with Provider Services (Non-Medical) or MCO Services | 15% | 21% |
| Difficulty with Obtaining: Dental/Orthodontia | 12% | 12% |
| Difficulty with Obtaining: Personal Care | 8% | 6% |
| Problems with Advertising/ Consumer Education/ Outreach/ Enrollment | 7% | 5% |
Monitoring of Plan Reported Complaints
The Department analyzes enrollee complaints by using an Observed to Expected (OE) ratio, to identify trends and potential problems.
The OE ratio is calculated by the Department for each MCO to determine which categories, if any, had a higher than expected number of enrollee complaints over a six-month period. The OE ratio compares the number of enrollee complaints the MCO reported to the number that is expected, based on the relative size of the MCO's Medicaid population and its share of enrollee complaints for each category compared to other MCOs. For example, an OE ratio of 6.2 means that the number of enrollee complaints reported for a category was over six times more than what was expected. An OE ratio of 0.5 means that there were half as many enrollee complaints reported for a given category as what was expected.
Based on the OE ratio over a six-month period, the Department requests that MCOs review and analyze categories of complaints where more than two times higher than expected complaint patterns persist. Where a persistent trend or an operational concern contributing to complaints is confirmed, the MCO is required to develop a corrective action plan.
The Department continues to monitor the progress of all corrective actions and requires additional intervention if the identified trend/issue persists.
| Complaint Category | OE Ratio | Issue Identified | Plan of Action |
|---|---|---|---|
| Affinity Health Plan FFY 21 Q2-FFY 21 Q3 (1/1/2021-6/30/2021) |
|||
| Denial of BH Clinical Treatment | 16.3 | The issue identified was that non-applicable provider action appeals were being reported by the MCO for both quarters, causing its reported numbers to be higher than expected. | The MCO will change the parameters for its reported action appeals to include only applicable action appeals. It will conduct additional training to ensure more accurate reporting. |
| Amida Care FFY 21 Q2-FFY 21 Q3 (1/1/2021-6/30/2021) |
|||
| Dissatisfaction with Provider Services (Non-Medical) or MCO Services | 12.0 | The trends identified from the complaints received were that MCO customer service staff were not meeting customer service standards, including enrollees experiencing difficulties contacting or receiving follow up calls from customer service staff, and that providers were not meeting customer service standards. | The MCO partnered with a call center services vendor in June 2021, hired additional customer service staff, implemented a new workflow, and will review calls received to meet customer service standards; will conduct additional refresher training and bi-weekly reviews for customer service staff to meet gender sensitivity standards; and will continue to provide targeted provider education to meet provider cultural sensitivity, gender sensitivity, and customer service standards. The Department will continue to monitor progress in the next reporting period due to this category's persistently high OE ratio. |
| Difficulty with Obtaining: Dental/ Orthodontia | 4.4 | The trends identified from the complaints received were that enrollees were dissatisfied with clinical requirements and time frames for dental benefits. | The MCO is developing materials that it will send out to help educate its enrollees on the specifications of what their dental coverage includes and reduce dissatisfaction. The issue identified was a lack of understanding by enrollees of requirements and processes for receiving dental services. |
| Pharmacy\Formulary | 14.8 | The trends identified from the complaints received were that enrollees were not receiving medication deliveries and there were delays with enrollees receiving prescriptions. The issues identified were that enrollees did not confirm availability for their medication deliveries and that providers were delayed in initiating prior authorization and/or sending prescriptions to the pharmacy. | The MCO will educate enrollees on pharmacy delivery protocols by conducting Town Hall meetings and using other methods of communication as necessary, and will coordinate provider education to help reduce prior authorization and prescription delays. The Department will continue to monitor progress in the next reporting period. |
| Difficulty with Obtaining: Personal Care | 12.5 | The trends identified from the complaints received were that enrollees were dissatisfied due to not having the same aide or schedule each day, not receiving the expected care, and having concerns regarding staffing availability. The issues identified were that enrollees had expectations that differed from their plan of care and had a lack of understanding of the requirements and processes for receiving a permanent aide. | The MCO is developing educational materials to improve enrollee understanding on staffing expectations, including requesting a permanent aide; communicating with the agency when concerns arise, including the escalation process for unaddressed issues; reviewing a plan of care; and how to request clarification from their agency when needed. The MCO will conduct orientation and training with agencies on policy and procedures to improve enrollee satisfaction. |
| Excellus Health Plan FFY 21 Q2-FFY 21 Q3 (1/1/2021-6/30/2021) |
|||
| Difficulty with Obtaining: Eye Care | 2.6 | The trend identified from the complaints received was that enrollees were being denied routine vision exams or eyewear due to benefit exhaustion. The issues identified were that non-applicable action appeals involving medical necessity were being reported by the MCO, causing its reported numbers to be higher than expected, and that the MCO's website contained misinformation regarding the benefit. | The MCO updated its website to correct the misinformation being presented, will change the parameters for its reported action appeals to include only applicable action appeals, and will educate providers and enrollees on the scope of the benefit to improve understanding. |
| Difficulty with Obtaining: Dental/ Orthodontia | 2.7 | The trend identified from the complaints and action appeals received was that enrollees were being denied services due to the lack of information being submitted with service authorization requests. The issue identified was that enrollees and providers were unaware of all the information needed to obtain approval. | The MCO will send out enrollee/provider communication to improve understanding on what information is needed to obtain authorization. The Department will continue to monitor progress in the next reporting period. |
| Healthfirst FFY 21 Q2-FFY 21 Q3 (1/1/2021-6/30/2021) |
|||
| Appointment Availability: PCP | 2.1 | The trend identified from the complaints received was that enrollees were unable to make appointments with in-network PCPs. The issues identified were that complaints regarding access to dentists were being miscategorized by the MCO, causing its reported numbers in this category to be higher than expected, and that providers were unable to accommodate appointments due to COVID-19 restrictions. | The MCO will communicate to enrollees that telemedicine is an alternative provider option to improve the enrollee's ability to see a PCP provider if COVID-19 restrictions prevent the provider from seeing the enrollee in person, and will educate their staff to ensure proper categorization of complaints. |
| Appointment Availability: Specialist | 3.1 | The trend identified from the complaints received was that enrollees were unable to make appointments with in-network specialists. The issues identified were that complaints regarding access to dentists were being miscategorized by the MCO, causing its reported numbers in this category to be higher than expected, and that providers were unable to accommodate appointments due to COVID-19 restrictions. | The MCO will communicate to enrollees that telemedicine is an alternative provider option to improve the enrollee's ability to see a specialist provider if COVID-19 restrictions prevent the provider from seeing the enrollee in person, and will educate their staff to ensure proper categorization of complaints. |
| Long Wait Time | 2.1 | The trend identified from the complaints received was that enrollees were dissatisfied with delays in being seen by providers. The issues identified were that providers reduced in-office practice hours due to COVID-19 and that providers tried to accommodate patients without appointments. | The MCO will communicate to enrollees that telemedicine is an alternative appointment option to reduce wait times if COVID-19 restrictions cause the provider to have limited in-office practice hours. |
| Dissatisfaction with Provider Services (Non-Medical) or MCO Services | 2.8 | The trends identified from the complaints received were that MCO customer service staff and providers were not meeting customer service standards, including rudeness and lack of communication, and that enrollees were experiencing issues related to durable medical equipment (DME), including delivery issues. | The MCO improved channels of communication to improve timely delivery of DME and will conduct monthly reviews with customer service leadership teams to address staff performance issues. The Department will continue to monitor progress in the next reporting period. |
| Difficulty with Obtaining: Specialist and Hospitals | 2.8 | The trends identified from the complaints received were that enrollees were dissatisfied with the provider network and were having difficulty obtaining specialist care. The issues identified were that providers were not meeting service standards and there were inadequate options for providers of specialty care. | The MCO highlighted providers offering telemedicine options in its directory and will continue to work with providers to improve enrollee specialty care access. The MCO will continue to follow up with providers it identified as having repeated complaints to improve provider service. |
| Pharmacy\Formulary | 2.3 | The trend identified from the complaints received was that enrollees were receiving pharmacy claim denials. The issues identified were that enrollees were unaware of other primary pharmacy insurance coverage preventing the MCO from approving pharmacy claims and that the MCO's formulary changes impacted coverage of over the counter (OTC) medications. | The MCO will directly handle coordination of benefit (COB) issues for its enrollees to reduce denials by implementing a process in which the pharmacy benefit manager (PBM) connects enrollees to the MCO when needed to complete an override, as well as a long-term solution of revalidating insurance coverage, and has trained MCO customer service staff to assist pharmacies and enrollees with finding OTC medications that are covered by its formulary. |
| Reimbursement/Billing | 3.0 | The trends identified from the complaints received were that enrollees were being billed for non-covered services and providers were incorrectly billing enrollees for services that should have been covered. The issues identified were that enrollees were unaware of which services are covered, and providers were unaware of the enrollee's insurance coverage. | The MCO will remind enrollees to present their insurance identification cards to assist providers in billing the correct insurance and will educate providers on proper billing protocols to reduce billing errors. |
| Difficulty with Obtaining: Private Duty Nursing | 4.4 | The trends identified from the complaints received were that private duty nursing (PDN) agencies were unable to provide adequate staffing for meeting the needs of enrollees and enrollees were dissatisfied with PDN services. The issues identified were that there was a shortage of private duty nurses and the nurses were not meeting service standards. | The MCO will continue to follow up with agencies it identifies as having repeated complaints to improve PDN services. The MCO will implement corrective action plans and address patterns of deficiencies within specific PDN agencies using penalties to their incentive programs to meet staffing needs. |
| Difficulty with Obtaining: Home Health Care | 2.9 | There were no trends identified by the MCO. The issue identified was that complaints regarding PDN and personal care were being miscategorized by the MCO, causing its reported numbers in this category to be higher than expected. | The MCO will educate their staff to ensure proper categorization of complaints. The Department will continue to monitor progress in the next reporting period. |
| Difficulty with Obtaining: Personal Care | 4.2 | The trends identified from the complaints received were that personal care aides were not meeting customer service standards and personal care agencies were unable to provide adequate staffing for meeting the needs of enrollees. The issues identified were that there was a shortage of aides and the aides were not meeting service standards. | The MCO will continue to follow up with agencies it identifies as having repeated complaints to improve personal care services. The MCO will implement corrective action plans and address patterns of deficiencies within specific personal care agencies using penalties to their incentive programs to meet staffing needs. The Department will continue to monitor progress in the next reporting period. |
| Difficulty with Obtaining: CDPAS | 4.1 | The trend identified from the complaints received was that enrollees were having problems starting and continuing CDPAS. The issues identified were that there were authorization issues and processing issues regarding payment, registering for CDPAS, and changing CDPAS status. | The MCO will follow up with fiscal intermediaries it identified as having repeated complaints to improve access to CDPAS. The Department will continue to monitor progress in the next reporting period. |
| Dissatisfaction with BH Provider Services | 3.5 | The complaints received were regarding enrollee dissatisfaction with behavioral health (BH) provider customer service. There were no trends or issues identified by the MCO. | The MCO will monitor for further trends. The Department will continue to monitor progress in the next reporting period. |
| HealthNow FFY 21 Q2-FFY 21 Q3 (1/1/2021-6/30/2021) |
|||
| Denial of Clinical Treatment | 7.6 | The trend identified from the complaints received was that enrollees were receiving denials for requested services from out of network (OON) providers. The issue identified was that enrollees were unaware of in-network providers offering the services they were seeking. | The MCO is including information on multiple in-network providers in denials enrollees receive for services from OON providers, to assist enrollees in accessing services. |
| Balance Billing | 3.6 | The trend identified from the complaints received was that providers were incorrectly billing enrollees for emergency services. The issue identified was that providers were unaware of the enrollee's insurance coverage. | The MCO will remind enrollees to present their insurance identification cards to assist providers in billing the correct insurance and will develop an educational piece to be posted on the enrollee website to reduce instances of improper billing. The Department will continue to monitor progress in the next reporting period. |
| HealthPlus FFY 21 Q2-FFY 21 Q3 (1/1/2021-6/30/2021) |
|||
| All Other | 2.7 | There were no trends identified by the MCO. The issue identified was that complaints were being miscategorized by the MCO, causing its reported numbers in this category to be higher than expected. | The MCO will work to ensure proper categorization of complaints. The Department will continue to monitor progress in the next reporting period. |
| Health Insurance Plan of Greater New York FFY 21 Q2-FFY 21 Q3 (1/1/2021-6/30/2021) |
|||
| Long Wait Time | 7.4 | The trend identified from the complaints received was that enrollees were dissatisfied with delays in being seen by providers. The issue identified was that providers had limited on-site appointment availability due to COVID-19. | The MCO will continue to communicate to enrollees that telemedicine is an alternative appointment option to reduce wait times if COVID-19 restrictions cause the provider to have limited on-site appointment availability, and the MCO stated that providers in its network are adding on-site appointment options. |
| Reimbursement/Billing | 2.8 | The trend identified from the complaints received was that enrollees were dissatisfied with receiving notice from the MCO for requests for payment. The issue identified was that enrollees were misinterpreting explanation of benefits (EOBs) as bills, even though no enrollee liability was listed. | The MCO is continuing to work on improving the clarity of its EOBs, to indicate no member liability, and to explore opportunities to improve how EOBs are provided to its enrollees. The Department will continue to monitor progress in the next reporting period. |
| Independent Health Association FFY 21 Q2-FFY 21 Q3 (1/1/2021-6/30/2021) |
|||
| Dissatisfaction with Quality of Care | 3.1 | The complaints received were regarding enrollee dissatisfaction with patient care. There were no trends or issues identified by the MCO. | The MCO will continue to evaluate participating provider performance and institute action plans for resolving instances of substandard care. The Department will continue to monitor progress in the next reporting period. |
| Difficulty with Obtaining: Dental/ Orthodontia | 3.0 | The trend identified from the complaints received was that enrollees were dissatisfied with the covered dental services. There were no issues identified by the MCO. | The MCO did not provide any plan of action, as the majority of complaints were for non-covered services. The Department will continue to monitor progress in the next reporting period. |
| Pharmacy\Formulary | 7.4 | The trend identified by the MCO was that enrollees were dissatisfied with prior authorization requirements and non-covered medications. The issue identified was that inquiries were being miscategorized by the MCO, causing its reported numbers in this category to be higher than expected. | The MCO will work to ensure proper categorization of inquiries and complaints. The Department will continue to monitor progress in the next reporting period. |
| Problems with Advertising\ Consumer Education\ Outreach\Enrollment | 3.0 | The trend identified by the MCO was that enrollees had concerns regarding their identification cards. The issue identified was that inquiries were being miscategorized by the MCO, causing its reported numbers in this category to be higher than expected. | The MCO will work to ensure proper categorization of inquiries and complaints. The Department will continue to monitor progress in the next reporting period. |
| All Other | 4.6 | The trend identified by the MCO was that enrollees had concerns regarding aspects of enrollment. The issues identified were that inquiries and interactive voice response (IVR) complaints were being miscategorized by the MCO, causing its reported numbers in this category to be higher than expected. | The MCO will work to ensure proper categorization of inquiries and complaints. The Department will continue to monitor progress in the next reporting period. |
| MetroPlus Health Plan FFY 21 Q2-FFY 21 Q3 (1/1/2021-6/30/2021) |
|||
| Appointment Availability: PCP | 3.3 | The trend identified from the complaints received was that enrollees were assigned PCPs who were no longer in-network or accepting new patients, or who had changed practices. The issue identified was that providers were not notifying the MCO of their status changes. | The MCO will increase the number of providers it surveys regarding their availability to see new patients; will educate providers on notifying the MCO of demographic and status changes, including creating a page on its provider portal website and adding alerts for providers to update their information; and will act on information received to ensure enrollees are assigned active, participating PCPs. |
| Difficulty with Obtaining: Emergency Services | 7.1 | The trend identified from the complaints received was that providers were incorrectly billing enrollees for emergency services. The issue identified was that providers were unaware of the enrollee's insurance coverage. | The MCO will remind enrollees through a member newsletter alert to present their insurance identification cards and will allow enrollees to access their identification cards electronically to assist providers in billing the correct insurance. The Department will continue to monitor progress in the next reporting period. |
| Problems with Advertising/ Consumer Education/ Outreach/ Enrollment | 2.2 | The trend identified from the complaints received was that enrollees were having issues receiving their identification cards. The issue identified was that enrollees were not reporting address changes. | The MCO will update its member portal to remind enrollees to report changes in their demographics, including address changes to ensure identification cards are received by the enrollee. |
| Balance Billing | 5.5 | The trend identified by the MCO was that enrollees had concerns regarding bills they received. The issue identified was that inquiries were being miscategorized by the MCO, causing its reported numbers in this category to be higher than expected. | The MCO will work to ensure proper categorization of inquiries and complaints. The Department will continue to monitor progress in the next reporting period. |
| Molina Healthcare FFY 21 Q2-FFY 21 Q3 (1/1/2021-6/30/2021) |
|||
| Dissatisfaction with Provider Services (Non-Medical) or MCO Services | 5.1 | The trend identified from the complaints received was that authorization requests were being denied by the MCO. The issue identified was that providers were not submitting authorization requests properly. | The MCO conducted provider education and outreach to help reduce the number of authorization request denials. |
| Difficulty with Obtaining: Specialist and Hospitals | 11.4 | The trend identified from the complaints received was that enrollees were dissatisfied with the participating provider options. The issues identified were that enrollees wanted continuity of care from OON providers and enrollees had difficulty navigating the MCO's provider directory. | The MCO implemented a new Single Case Agreement (SCA) policy in which OON providers who enrollees regularly request access to are contacted to become participating providers. The MCO updated its provider directory to improve access to participating providers for enrollees. |
| Difficulty with Obtaining: Dental/Orthodontia | 2.9 | The trend identified from the complaints received was that enrollees were appealing non-covered service denials. The issue identified was that enrollees and providers needed more education and resources regarding benefit coverage. | The MCO is developing a plan to improve enrollee and provider education and access to resources regarding benefit coverage. The Department will continue to monitor progress in the next reporting period. |
| Pharmacy\Formulary | 6.7 | The trend identified from the complaints received was that enrollees were receiving denials for medications. The issue identified was that prior authorization requests did not include all necessary clinical information. | The MCO continues to provide education and training to its customer service representatives to help enrollees and providers submit the proper documentation for prior authorization requests. |
| Problems with Advertising\ Consumer Education\ Outreach\ Enrollment | 9.4 | There were no trends identified by the MCO. The issue identified was that complaints were being miscategorized by the MCO, causing its reported numbers in this category to be higher than expected. | The MCO will educate their staff to ensure proper categorization of complaints. The Department will continue to monitor progress in the next reporting period. |
| All Other | 25.9 | The trends identified from the complaints received were that enrollees were dissatisfied with the MCO's authorization requirements and the MCO's IVR. The issues identified were that enrollees and providers from the Your Care acquisition were still adjusting to the new authorization process, the IVR was changed to incorporate more options, and complaints were being miscategorized by the MCO, causing its reported numbers in this category to be higher than expected. | The MCO will educate providers on authorization requirements to help ensure they are completed correctly. The MCO will also update the IVR to address any complaint trends and educate its staff to ensure proper categorization of complaints. |
| Balance Billing | 5.3 | The trends identified from the complaints received were that enrollees were dissatisfied with receiving notice from the MCO for requests for payment and being billed directly by providers. The issues identified were that enrollees were misinterpreting EOBs as bills, even though no enrollee liability was listed, and that providers billing enrollees directly were unaware of standard Medicaid practices. | The MCO has provided multiple notices and newsletters to improve understanding of EOBs and has educated providers on standard Medicaid practices during provider group meetings to prevent enrollees from being billed directly. The Department will continue to monitor progress in the next reporting period. |
| MVP Health Plan FFY 21 Q2-FFY 21 Q3 (1/1/2021-6/30/2021) |
|||
| Difficulty with Obtaining: Dental/ Orthodontia | 3.3 | The trend identified from the complaints received was that enrollees' customer service expectations at dental practices were not being met. The issues identified were that dental treatment plans were not being discussed, appointments that got cancelled were not rescheduled in a timely manner, and authorization requests with proper information were not submitted timely. | The MCO educated dental providers to help them meet customer service expectations and complete administrative tasks timely. The Department will continue to monitor progress in the next reporting period. |
| United Healthcare FFY 21 Q2-FFY 21 Q3 (1/1/2021-6/30/2021) |
|||
| Dissatisfaction with Quality of Care | 2.7 | The trend identified from the complaints received was that enrollees were dissatisfied with their care. The issue identified was that providers were not thorough enough with their care. | The MCO reached out to the providers who treated the enrollees who were dissatisfied with their care to ensure that enrollee concerns are addressed. The Department will continue to monitor this category. |
| Denial of Clinical Treatment | 9.7 | The trend identified from the complaints received was that enrollees were receiving service denials. The issue identified was that enrollees were not informed about the benefits available to them. | The MCO continues to provide education and training to its customer service representatives to better inform enrollees of their available benefits. The Department will continue to monitor progress in the next reporting period. |
| Communications/ Physical Barrier | 6.0 | There were no trends identified by the MCO. The issue identified was that complaints regarding customer service were being miscategorized by the MCO, causing its reported numbers in this category to be higher than expected. | The Department will follow up with the MCO to advise of the miscategorized complaints. The Department will continue to monitor progress in the next reporting period. |
| VNS Choice FFY 21 Q2-FFY 21 Q3 (1/1/2021-6/30/2021) |
|||
| Difficulty with Obtaining: Dental/Orthodontia | 15.2 | The trend identified from the complaints received was that enrollees were receiving denials for non-covered dental services. The issue identified was that enrollees were unaware of what services were covered under their dental benefit. | The MCO will send out educational materials to help educate its enrollees on the specifications of what their dental coverage includes and increase awareness. |
| All Other | 21.5 | There were no trends identified by the MCO. The issue identified was that complaints submitted did not contain enough details to identify an appropriate category. | The MCO will continue to conduct outreach to enrollees who submit complaints with insufficient information and will educate their customer service staff to collect the necessary information to better categorize these complaints. |
Long Term Services and Supports (LTSS)
As SSI recipients typically access LTSS, the Department monitors complaints and action appeals filed with MCOs by SSI recipients. Of the 8,426 total reported complaints/action appeals, MCOs reported 1,171 complaints and action appeals from their SSI recipients. This compares to 1,060 SSI complaints/action appeals from the previous quarter, representing a 10.5% increase.
The following table outlines the total number of complaints/action appeals MCOs reported for SSI recipients by category for the most recent quarter and the last four (4) quarters:
| Description of Complaint | Number of Complaints/Action Appeals Reported for SSI Recipients | |
|---|---|---|
| FFY 21 Q4 7/1/2021-9/30/2021 | Last 4 Quarters 10/1/2020-9/30/2021 | |
| Appointment Availability: PCP | 7 | 33 |
| Appointment Availability: Specialist | 10 | 32 |
| Appointment Availability: BH HCBS | 0 | 0 |
| Long Wait Time | 0 | 7 |
| Dissatisfied with Quality of Care | 105 | 366 |
| Denial of Clinical Treatment | 27 | 121 |
| Denial of BH Clinical Treatment | 0 | 3 |
| Dissatisfied with Provider Services (Non-Medical) or MCO Services | 347 | 1,495 |
| Dissatisfaction with BH Provider Services | 0 | 5 |
| Dissatisfaction with Health Home Care Management | 6 | 7 |
| Difficulty with Obtaining: Specialist and Hospitals | 80 | 162 |
| Difficulty with Obtaining: Eye Care | 8 | 25 |
| Difficulty with Obtaining: Dental/Orthodontia | 35 | 149 |
| Difficulty with Obtaining: Emergency Services | 0 | 7 |
| Difficulty with Obtaining: Mental Health or Substance Abuse Services/Treatment | 3 | 15 |
| Difficulty with Obtaining: RHCF Services | 1 | 1 |
| Difficulty with Obtaining: Adult Day Care | 0 | 2 |
| Difficulty with Obtaining: Private Duty Nursing | 25 | 64 |
| Difficulty with Obtaining: Home Health Care | 22 | 105 |
| Difficulty with Obtaining: Personal Care | 99 | 500 |
| Difficulty with Obtaining: PERS | 3 | 13 |
| Difficulty with Obtaining: CDPAS | 58 | 128 |
| Difficulty with Obtaining: AIDS Adult Day Health Care | 1 | 1 |
| Pharmacy/Formulary | 117 | 320 |
| Access to Non-Covered Services | 7 | 45 |
| Access for Family Planning Services | 0 | 4 |
| Communications/ Physical Barrier | 2 | 8 |
| Problems with Advertising/ Consumer Education/ Outreach/ Enrollment | 22 | 51 |
| Recipient Restriction Program and Plan Initiated Disenrollment | 0 | 2 |
| Reimbursement/Billing | 86 | 363 |
| Balance Billing | 53 | 224 |
| Transportation | 28 | 79 |
| All Other | 19 | 142 |
| Total | 1,171 | 4,480 |
The following table outlines the top five (5) most frequent categories of SSI recipient complaints/action appeals MCOs reported for the most recent quarter and the last four (4) quarters:
| Description of Complaint | Percentage of Total Complaints/Appeals Reported for SSI Recipients | ||
|---|---|---|---|
| FFY 21 Q4 7/1/2021-9/30/2021 | Last 4 Quarters 10/1/2020-9/30/2021 | ||
| Dissatisfied with Provider Services (Non-Medical) or MCO Services | 30% | 33% | |
| Pharmacy/Formulary | 10% | 7% | |
| Dissatisfied with Quality of Care | 9% | 8% | |
| Difficulty with Obtaining: Personal Care | 8% | 11% | |
| Reimbursement/Billing | 7% | 8% | |
The Department requires MCOs to report the number of enrollees in receipt of LTSS as of the last day of the quarter. During the current reporting period of July 1, 2021 through September 30, 2021, MCOs reported LTSS enrollment of 45,258 enrollees. This compares to 44,432 LTSS enrollees from the previous quarter, representing a 1.9% increase. The following table outlines the number of LTSS enrollees by MCO for each of the last four (4) quarters:
| Plan | Number of LTSS Enrollees | |||
|---|---|---|---|---|
| FFY 21 Q4 7/1/2021-9/30/2021 | FFY 21 Q3 4/1/2021-6/30/2021 | FFY 21 Q2 1/1/2021-3/31/2021 | FFY 21 Q1 10/1/2020-12/31/2020 | |
| Affinity Health Plan | 987 | 954 | 905 | 870 |
| Amida Care | 1,366 | 1,425 | 1,705 | 1,471 |
| Capital District Physicians Health Plan | 699 | 677 | 630 | 605 |
| Excellus Health Plan | 1,526 | 1,568 | 1,555 | 1,542 |
| Fidelis Care | 15,517 | 14,960 | 14,328 | 14,005 |
| Healthfirst | 12,314 | 11,882 | 11,528 | 11,187 |
| HealthNow | 206 | 198 | 182 | 176 |
| HealthPlus | 2,896 | 2,728 | 2,892 | 2,989 |
| HIP of Greater New York | 367 | 355 | 333 | 335 |
| Independent Health Association | 512 | 508 | 484 | 452 |
| MetroPlus Health Plan | 2,757 | 2,604 | 3,380 | 3,074 |
| Molina Healthcare | 1,094 | 1,635 | 1,412 | 1,323 |
| MVP Health Plan | 1,825 | 1,812 | 1,691 | 1,755 |
| United Healthcare | 2,850 | 2,761 | 2,730 | 2,644 |
| VNS Choice | 342 | 365 | 348 | 345 |
| Total | 45,258 | 44,432 | 44,103 | 42,773 |
The following table outlines the total number of complaints/action appeals received from all enrollees, regardless of product line, regarding difficulty with obtaining LTSS that MCOs reported for each of the last four quarters:
| Description of Complaint | Number of Complaints/Action Appeals Reported | |||
|---|---|---|---|---|
| FFY 21 Q4 7/1/2021-9/30/2021 | FFY 21 Q3 4/1/2021-6/30/2021 | FFY 21 Q2 1/1/2021-3/31/2021 | FFY 21 Q1 10/1/2020-12/31/2020 | |
| Difficulty with Obtaining: AIDS Adult Day Health Care | 5 | 3 | 1 | 0 |
| Difficulty with Obtaining: Adult Day Care | 2 | 3 | 2 | 0 |
| Difficulty with Obtaining: CDPAS | 106 | 41 | 66 | 41 |
| Difficulty with Obtaining: Home Health Care | 60 | 92 | 53 | 43 |
| Difficulty with Obtaining: RHCF Services | 3 | 6 | 1 | 0 |
| Difficulty with Obtaining: Personal Care | 257 | 238 | 435 | 264 |
| Difficulty with Obtaining: PERS | 9 | 6 | 11 | 7 |
| Difficulty with Obtaining: Private Duty Nursing | 35 | 21 | 25 | 10 |
| Total | 477 | 410 | 594 | 365 |
The increase in Difficulty Obtaining: CDPAS compared to last quarter was due to one MCO's increase in reported complaints for the category. The Department is actively monitoring the complaint category.
B. Critical Incidents:
The Department requires MCOs to report critical incidents involving enrollees in receipt of LTSS. There were 103 critical incidents reported for the July 1, 2021 through September 30, 2021 period, most of which have a resolved status. Many of the incidents stemmed from falls. The Department continues to work with MCOs to maintain accuracy in reporting of their LTSS critical incident numbers.
The following table outlines the total number of LTSS critical incidents reported by MMCs, HARPs, and HIV SNPs for each of the last two (2) quarters, the net change over the last two (2) quarters, and the total for the last four (4) quarters:
| Plan Name | Critical Incidents | |||
|---|---|---|---|---|
| FFY 21 Q4 7/1/2021-9/30/2021 | FFY 21 Q3 4/1/2021-6/30/2021 | Net Change | Last 4 Quarters 10/1/2020-9/30/2021 | |
| Medicaid Managed Care Plans | ||||
| Affinity Health Plan | 0 | 0 | 0 | 0 |
| Capital District Physicians Health Plan | 0 | 1 | -1 | 1 |
| Excellus Health Plan | 3 | 5 | -2 | 50 |
| Fidelis Care | 0 | 0 | 0 | 0 |
| Healthfirst | 32 | 30 | +2 | 99 |
| HIP of Greater New York | 0 | 0 | 0 | 0 |
| HealthNow | 0 | 0 | 0 | 0 |
| HealthPlus | 2 | 1 | +1 | 7 |
| Independent Health Association | 0 | 0 | 0 | 0 |
| MetroPlus Health Plan | 1 | 1 | 0 | 2 |
| Molina Healthcare | 0 | 1 | -1 | 4 |
| MVP Health Plan | 1 | 2 | -1 | 6 |
| United Healthcare | 0 | 0 | 0 | 0 |
| Total | 39 | 41 | -2 | 169 |
| Health and Recovery Plans | ||||
| Affinity Health Plan | 0 | 0 | 0 | 0 |
| Capital District Physicians Health Plan | 0 | 0 | 0 | 0 |
| Excellus Health Plan | 6 | 5 | +1 | 23 |
| Fidelis Care | 0 | 0 | 0 | 0 |
| Healthfirst | 54 | 38 | +16 | 158 |
| HIP of Greater New York | 0 | 0 | 0 | 0 |
| HealthPlus | 0 | 0 | 0 | 0 |
| Independent Health Association | 0 | 0 | 0 | 0 |
| MetroPlus Health Plan | 0 | 0 | 0 | 0 |
| Molina Healthcare | 0 | 1 | -1 | 2 |
| MVP Health Plan | 2 | 0 | +2 | 3 |
| United Healthcare | 0 | 0 | 0 | 0 |
| VNS Choice | 0 | 4 | -4 | 5 |
| Total | 62 | 48 | +14 | 191 |
| HIV Special Needs Plans | ||||
| Amida Care | 0 | 0 | 0 | 0 |
| MetroPlus Health Plan | 0 | 0 | 0 | 0 |
| VNS Choice | 2 | 1 | +1 | 7 |
| Total | 2 | 1 | +1 | 7 |
| Grand Total | 103 | 90 | +13 | 367 |
The following table outlines the total number of critical incidents MCOs reported for enrollees in receipt of LTSS by category for each of the last two (2) quarters, the net change over the last two (2) quarters, and the total for the last four (4) quarters:
| Plan Name | Critical Incidents | |||
|---|---|---|---|---|
| FFY 21 Q4 7/1/2021-9/30/2021 | FFY 21 Q3 4/1/2021-6/30/2021 | Net Change | Last 4 Quarters 10/1/2020-9/30/2021 | |
| Medicaid Managed Care Plans | ||||
| Any Other Incidents as Determined by the Plan | 2 | 3 | -1 | 14 |
| Crimes Committed Against Enrollee | 1 | 2 | -1 | 11 |
| Crimes Committed by Enrollee | 0 | 3 | -3 | 7 |
| Instances of Abuse of Enrollees | 1 | 2 | -1 | 12 |
| Instances of Exploitation of Enrollees | 1 | 0 | +1 | 1 |
| Instances of Neglect of Enrollees | 2 | 1 | +1 | 9 |
| Medication Errors that Resulted in Injury | 0 | 0 | 0 | 1 |
| Other Incident Resulting in Hospitalization | 6 | 9 | -3 | 43 |
| Other Incident Resulting in Medical Treatment Other Than Hospitalization | 26 | 21 | +5 | 68 |
| Use of Restraints | 0 | 0 | 0 | 2 |
| Wrongful Death | 0 | 0 | 0 | 1 |
| Total | 39 | 41 | -2 | 169 |
| Health and Recovery Plans | ||||
| Any Other Incidents as Determined by the Plan | 3 | 2 | +1 | 9 |
| Crimes Committed Against Enrollee | 1 | 2 | -1 | 5 |
| Crimes Committed by Enrollee | 2 | 0 | +2 | 2 |
| Instances of Abuse of Enrollees | 1 | 0 | +1 | 3 |
| Instances of Exploitation of Enrollees | 0 | 1 | -1 | 1 |
| Instances of Neglect of Enrollees | 1 | 1 | 0 | 3 |
| Medication Errors that Resulted in Injury | 0 | 0 | 0 | 1 |
| Other Incident Resulting in Hospitalization | 5 | 8 | -3 | 28 |
| Other Incident Resulting in Medical Treatment Other Than Hospitalization | 49 | 34 | +15 | 136 |
| Use of Restraints | 0 | 0 | 0 | 1 |
| Wrongful Death | 0 | 0 | 0 | 2 |
| Total | 62 | 48 | +14 | 191 |
| HIV Special Needs Plans | ||||
| Instances of Abuse of Enrollees | 0 | 0 | 0 | 0 |
| Instances of Neglect of Enrollees | 1 | 1 | 0 | 4 |
| Other Incident Resulting in Hospitalization | 0 | 0 | 0 | 1 |
| Other Incident Resulting in Medical Treatment Other Than Hospitalization | 1 | 0 | +1 | 2 |
| Total | 2 | 1 | +1 | 7 |
| Grand Total | 103 | 90 | +13 | 367 |
C. Enrollee Complaints Received Directly by the Department
In addition to the MCO reported complaints, the Department directly received 50 enrollee complaints this quarter. This total is a 56.8% decrease from the previous quarter, which reported 88 enrollee complaints.
Annually, the Department directly received 311 MCO member complaints regarding MMCs, HARPs, and HIV SNPs. The following chart represents previously reported complaints filed directly with NYSDOH, including complaints from members and their representatives.
| MCO Enrollee Complaints Received Directly by the Department | ||||
|---|---|---|---|---|
| FFY 21 Q4 7/1/2021-9/30/2021 | FFY 21 Q3 4/1/2021-6/30/2021 | FFY 21 Q2 1/1/2021-3/31/2021 | FFY 21 Q1 10/1/2020-12/31/2020 | Total FFY 21 10/1/2020-9/30/2021 |
| 50 | 88 | 92 | 81 | 311 |
The top five (5) most frequent categories of enrollee complaints received directly by the Department involving MCOs were as follows:
| Percentage of MCO Enrollee Complaints Received Directly by the Department | ||||
|---|---|---|---|---|
| Description of Complaint | FFY 21 Q4 7/1/2021-9/30/2021 | FFY 21 Q3 4/1/2021-6/30/2021 | FFY 21 Q2 1/1/2021-3/31/2021 | FFY 21 Q1 10/1/2020-12/31/2020 |
| Pharmacy/Formulary | 8% | 14% | 17% | 9% |
| Reimbursement/Billing | 16% | 13% | 8% | 16% |
| Problems with Advertising/ Consumer Education/ Outreach/ Enrollment | 12% | 5% | 5% | 1% |
| Difficulty with Obtaining: Home Health Care | 8% | 6% | 4% | 1% |
| Dissatisfied with Quality of Care | 8% | 0% | 0% | 1% |
The Department monitors and tracks enrollee complaints reported to the Department related to new or changed benefits and populations enrolled into MCOs.
In compliance with the Families First Coronavirus Response Act, Medicaid Managed Care enrollees have remained eligible for and enrolled in Medicaid. This has been in effect since March 18, 2020, with exceptions being enrollees who move out of state or who elect to cancel their coverage. Since March of 2020 the Department has carefully monitored any complaints regarding MCO enrollment issues related to suspended loss of Medicaid coverage and addressed these issues in accordance with maintenance of effort requirements during this period.
On July 1, 2021, New York State's Foster Care Transition to Medicaid Managed Care went into effect, completing the Medicaid Redesign Team's Children's Medicaid System Transformation and expanding the population and benefits under Medicaid Managed Care. Individuals in foster care populations were no longer excluded from MMC or HIV SNP enrollment. As part of this transition, most Voluntary Foster Care Agencies voluntarily transitioned into Article 29-I Health Facilities to provide those in foster care with Core Limited Health-Related Services, including skill building services, nursing supports and medication management, Medicaid treatment planning and discharge planning, clinical consultation and supervision, managed care liaison/administration, and optional additional services. The Department is actively tracking any complaints that arise from expanding the population and benefits under this transition and treating them as urgent issues to be addressed.
D. Fair Hearings
There were 392 fair hearings involving MMCs, HARPs, and HIV SNPs during the period of July 1, 2021 through September 30, 2021. The dispositions of these fair hearings as well as the previous three quarters are as follows:
| Fair Hearing Decisions (includes MMC, HARP and HIV SNP) | ||||
|---|---|---|---|---|
| Hearing Dispositions | FFY 21 Q4 7/1/2021-9/30/2021 | FFY 21 Q3 4/1/2021-6/30/2021 | FFY 21 Q2 1/1/2021-3/31/2021 | FFY 21 Q1 10/1/2020-12/31/2020 |
| In favor of Appellant | 91 | 84 | 79 | 96 |
| In favor of Plan | 272 | 225 | 157 | 153 |
| No Issue | 29 | 28 | 20 | 39 |
| Total | 392 | 337 | 256 | 288 |
For fair hearing dispositions occurring for the most recent quarter and for the previous quarter, the following table describes the number of days from the initial request for a fair hearing to the final disposition of the hearing, including time elapsed due to adjournments.
| Fair Hearing Days from Request Date till Decision Date (includes MMC, HARP and HIV SNP) | ||||
|---|---|---|---|---|
| Decision Days | FFY 21 Q4 7/1/2021-9/30/2021 | FFY 21 Q3 4/1/2021-6/30/2021 | FFY 21 Q2 1/1/2021-3/31/2021 | FFY 21 Q1 10/1/2020-12/31/2020 |
| 0-29 | 13 | 16 | 14 | 18 |
| 30-59 | 93 | 50 | 31 | 55 |
| 60-89 | 90 | 66 | 32 | 42 |
| 90-119 | 54 | 53 | 29 | 60 |
| =>120 | 142 | 152 | 150 | 113 |
| Total | 392 | 337 | 256 | 288 |
E. Medicaid Managed Care Advisory Review Panel (MMCARP) Meetings
Quarter 4: No activity to report during this quarter. The next MMCARP meeting is scheduled for October 7, 2021.
Annual: The Medicaid Managed Care Advisory Review Panel is required to meet quarterly. Meetings were held on December 17, 2020, February 18, 2021, June 17, 2021. The September 23, 2021 meeting was rescheduled to October 7, 2021 due to scheduling conflicts.
VIII. Quality Assurance/Monitoring
A. Quality Measurement in Managed Long-Term Care
In October 2020, the Department released the 2019 MLTC Report was publicly released in October. This Report presents information on the 50 plans that were enrolling members during the data collection period. This Report is the basis for the Consumer Guides and the Quality Incentive.
The 2019 MLTC Consumer Guides were released in December 2020 on the Department's website. The Guides are also printed by Maximus, our facilitated Medicaid enroller, for inclusion in new member's packets. The Guides help new members to choose a managed long-term care plan that meets their health care needs. The Guides offer information about the quality of care offered by the different plans, and people's opinions about the care and services the plans provide.
The 2019 Quality Incentive awards were announced in April 2021. The quality incentive is calculated on the percentage of total points a plan earned in the areas of quality, satisfaction, compliance, and efficiency. Since the MLTC is budget neutral, the bottom tier did not receive any contributed monies back, all the other tiers received back a portion or full amount of contributed monies plus additional award.
| 2019 MLTC Quality Incentive Results | ||||
|---|---|---|---|---|
| Payer | Plan ID | Plan Name | QI Points, adjusted | Tier |
| MAP | 02914056 | VNS CHOICE Total | 75.77 | 3 |
| MAP | 03173113 | Elderplan | 68.11 | 3 |
| partial | 03506989 | Centers Plan for Healthy Living | 65.56 | 3 |
| PACE | 03114514 | ArchCare Senior Life | 64.29 | 3 |
| partial | 02644562 | Empire BCBS HealthPlus MLTC | 63.01 | 3 |
| partial | 03234044 | ElderServe dba RiverSpring | 63.01 | 3 |
| partial | 03459881 | Senior Whole Health Partial | 61.74 | 3 |
| partial | 03253707 | Elderplan dba Homefirst | 61.74 | 3 |
| partial | 03581413 | Prime Health Choice | 60.46 | 2 |
| MAP | 02932896 | Senior Whole Health | 60.32 | 2 |
| MAP | 04682248 | VillageCareMAX Total Advantage | 57.91 | 2 |
| partial | 03549135 | Extended MLTC | 56.63 | 2 |
| partial | 03466906 | MetroPlus MLTC | 56.63 | 2 |
| partial | 01750467 | VNS CHOICE MLTC | 55.36 | 2 |
| partial | 03475427 | Integra MLTC | 55.36 | 2 |
| partial | 03522947 | Hamaspik Choice | 54.08 | 2 |
| partial | 02104369 | Senior Health Partners | 51.53 | 2 |
| partial | 03420399 | VillageCareMAX | 51.53 | 2 |
| partial | 03481927 | AgeWell New York | 48.98 | 1 |
| PACE | 04190745 | Fallon Health Weinberg-PACE | 48.41 | 1 |
| partial | 01825947 | EverCare Choice | 47.70 | 1 |
| partial | 03458546 | Aetna Better Health | 47.70 | 1 |
| partial | 03466800 | ArchCare Community Life | 46.43 | 1 |
| MAP | 03420808 | MHI Healthfirst Complete Care | 46.43 | 1 |
| PACE | 03072740 | Catholic Health -LIFE | 43.88 | 1 |
| partial | 01788325 | Fidelis Care | 41.84 | 1 |
| partial | 01778523 | Senior Network Health | 40.05 | 0 |
| PACE | 01234037 | CenterLight PACE | 38.78 | 0 |
| PACE | 03056544 | Total Senior Care | 38.49 | 0 |
| PACE | 01519162 | PACE CNY | 36.22 | 0 |
| partial | 01865329 | Independence Care System | 34.95 | 0 |
| partial | 03439663 | United Health Personal Assist | 34.95 | 0 |
| partial | 02188296 | Fallon Health Weinberg | 33.67 | 0 |
| partial | 03594052 | Montefiore MLTC | 33.67 | 0 |
| MAP | 02927631 | Fidelis Legacy Plan | 33.33 | 0 |
| PACE | 03320725 | Complete Senior Care | 33.22 | 0 |
| partial | 03529059 | Nascentia Health Options | 31.12 | 0 |
| partial | 02825230 | WellCare Advocate Partial | 31.12 | 0 |
| PACE | 01674982 | Eddy Senior Care | 29.37 | 0 |
| partial | 03866960 | iCircle | 28.57 | 0 |
| partial | 03690851 | Kalos Health | 28.57 | 0 |
| partial | 04122776 | Elderwood Health Plan | 28.08 | 0 |
| PACE | 01278899 | ElderONE | 23.47 | 0 |
*Centers Plan Map and Empire BCBS HealthPlus MAP are excluded due to having less than 50% of possible base points.
B. Quality Measurement in Medicaid Managed Care
Quality Measure Benchmarks 2020 (Measurement Year 2019)
Quality of care remained high for Medicaid Managed Care members for the Demonstration Year. In measurement year 2019 national benchmarks were available for 52 measures for Medicaid. Out of the 52 measures that NYS Medicaid plans reported, 82% of measures met or exceeded national benchmarks. New York State consistently met or exceeded national benchmarks across measures, especially in Medicaid managed care. The NYS Medicaid, rates exceed the national benchmarks for behavioral health on adult measures (e.g., receiving follow-up within 7 and 30 days after an emergency department visit for mental illness), and child measures (e.g., metabolic monitoring for children and adolescents on antipsychotics, the initiation/continuation of follow-care for children prescribed ADHD medication, and the use of first-line psychosocial care for children and adolescents on antipsychotics). New York State managed care plans also continue to surpass national benchmarks in several women's preventive care measures (e.g., postnatal care, as well as screening for Chlamydia, and cervical cancer). There were COVID-19 related impacts to Medicaid statewide reporting due to interruptions to medical record review that typically take place in January - March. The state selected the higher of the two measurement years, 2018 or 2019, for hybrid measures to respond to the pandemic related impacts.
2020 Satisfaction Survey
The Department conducted a satisfaction survey with children enrolled in Medicaid managed care in the fall of 2020. The Consumer Assessment of Healthcare Providers and systems (CAHPS®) Medicaid 5.0 Child survey was administered to parents of children, ages 0 to 17, enrolled in Medicaid. The administration methodology consisted of a two-wave mailing protocol, with telephone follow up for non-responders. The overall response rate was 21.9% (with a range of 16% to 30% for response rates by plan). This return rate was slightly higher than the previous child survey that was fielded in 2018. The responses to the survey were analyzed and released to the plans in May 2021.
Response options for overall rating questions ranged from 0 (worst) to 10 (best). In the table below, the achievement score represents the proportion of parents/caretakers of members who responded with a rating of "8", "9", or "10". Results are presented for MMC/CHP Statewide, Payer status (Medicaid and CHP), and Chronic Condition status (CC-Negative and CC-Positive). Payer status and Chronic Condition status are presented for additional information but are not compared to the MMC/CHP Statewide achievement scores.
CC-Negative and CC-Positive scores represent a split of all respondents by the child member's chronic condition status. Chronic condition status is determined by the parent's/caretaker's answers to screening questions. The child member is considered positive for a chronic condition if the responses to one or more of five sets of screening questions indicates a chronic condition.
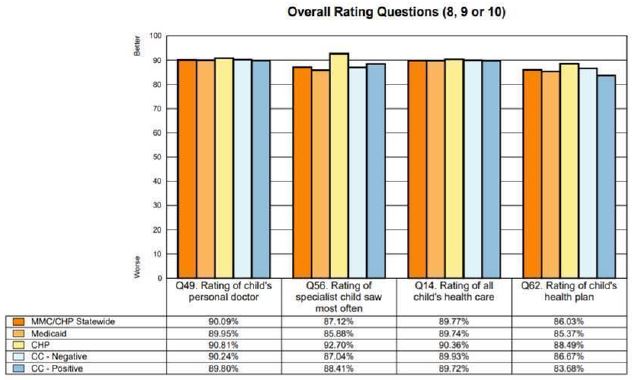
2020 Quality Incentive for Medicaid Managed Care
The 2020 Quality Incentive Awards calculations were finalized in July 2021. The quality incentive is calculated on the percentage of total points a plan earned in the areas of quality, satisfaction, and Prevention Quality Indicators. Points for issues with Compliance are subtracted from the total plan points before calculating the percentage of total points. Plans were classified into 5 Tiers based on their total score. The amount of the incentive award is determined by the Division of Finance and Rate Setting and subject to final approval from Division of Budget and the Center for Medicare and Medicaid Services (CMS). The results for the 2020 Incentive included no plans in Tier 1, ten plans receiving some portion of the award (Tier 2-3), four plans in Tier 4, and one plan in Tier 5.
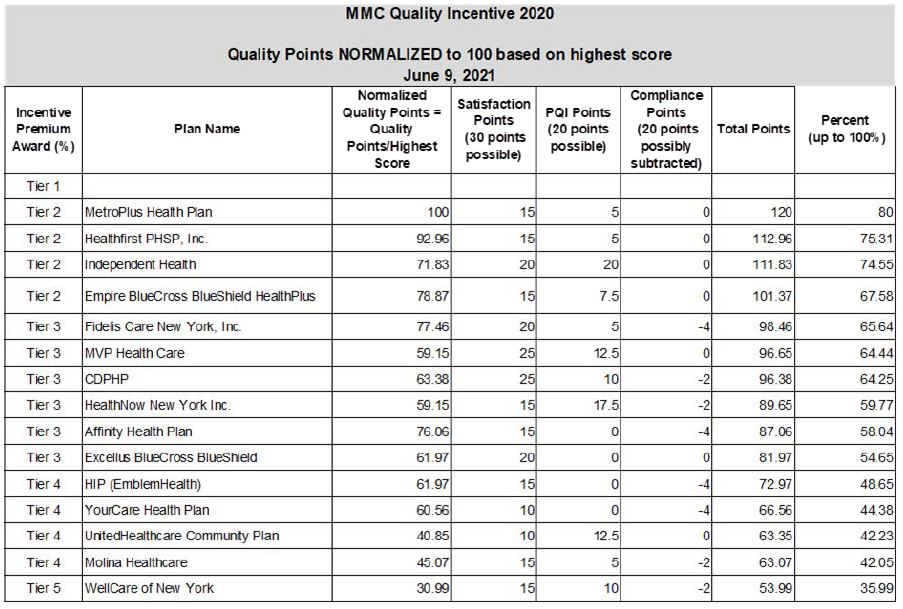
Quality Assurance Reporting Requirements (QARR)
We had 26 health plans submit Quality Assurance Reporting Requirement (QARR) data on June 15, 2021. Data is being reviewed for completeness and accuracy and final results will be published by December 2021.
C. Quality Improvement
External Quality Review
IPRO continues to provide EQR services related to required, optional, and supplemental activities, as described by CMS in 42 CFR, Part 438, Subparts D and E, expounded upon in NYS's consolidated contract with IPRO. Ongoing activities include: 1) validation of performance improvement projects (PIPs); 2) validation of performance measures; 3) review of MCO compliance with state and federal standards for access to care, structure and operations, and quality measurement and improvement; 4) validating encounter and functional assessment data reported by the MCOs; 5) overseeing collection of provider network data; 6) administering and validating consumer satisfaction surveys; 7) conducting focused clinical studies; and 8) developing reports on MCO technical performance. In addition to these specified activities, NYSDOH requires our EQRO to also conduct activities including performing medical record reviews in MCOs, hospitals, and other providers; administering additional surveys of enrollee experience; and, providing data processing and analytical support to the Department. EQR activities cover services offered by New York's MMC plans, HIV-SNPs, MLTC plans, HARPs, and BHOs, and include the state's Child Health Insurance Program (CHP). Some projects may also include the Medicaid FFS population, or, on occasion, the commercial managed care population for comparison purposes.
During 2021 the Access Survey of Provider Availability (Provider Directory) was completed, and the final report was prepared by the EQRO and reviewed by OHIP. At the end of the 4th quarter, OHIP still had the final report in their quality assurance review process. The EQRO will conduct a re-survey of failed providers when OHIP gives them authorization. The Member Services Survey was conducted in 2021 and the final report of the survey was prepared by the EQRO and provided to OHIP. At the end of the 4th quarter, the final report was in OHIP's review and approval process. The EQRO will start a new Member Services Survey when they have OHIP's authorization to begin. The High-Volume PCP Ratio survey was completed by the EQRO in 2021, and in the 4th quarter, the final report for the survey was in OHIP's review process.
In the 2nd quarter of 2021, IPRO began the Behavioral Health Access & Availability (BH A&A) Survey, on behalf of the NYS Office of Mental Health (OMH). The survey was completed by the end of the 3rd quarter and a final report was being prepared in the 4th quarter. By the end of the 4th quarter, it was determined that the final report will be used for information purposes only and will not be distributed to the plans. For the 3rd quarter the BH A&A survey was completed and IPRO provided OMH with a final report of the survey findings.
Provider Network Data System (PNDS)
IPRO continued to oversee two sub-contracts, RMCI and Quest Analytics, for the management of the rebuild of the Provider Network Data System (PNDS). IPRO facilitated ongoing adjustments and fixes required for the PNDS rebuild and addressed any continuing issues with the rebuild of the PNDS network, relative to use, expansion, and maintenance. Quarter 2 2021 PNDS submission requires health plans to submit network information between April1st- June 30th. The deadline was at the end of July 2021. There are currently around 400 active networks in NYS that are submitting data to the PNDS every quarter.
Provider Network Panel
Panel data submissions resulted in 6,464,252 records (members enrolled in MMC, HARP, SNP, QHP, EP/AP and CHP). Technical assistance was provided by DOH and IPRO throughout the submission process. DOH provided detailed analytics to plans to address fields at risk of failing thresholds. Manual checks are still required to ensure the data submitted is complete and accurate. DOH continues to revise and build on the Standard Operating Procedures to improve efficiency and streamline processes.
Provider and Health Plan LOOK-UP
Refreshes continued to occur on a monthly basis. DOH continued to monitor the site for content and functionality. DOH and IPRO worked collaboratively to address and remediate minor site functionality issues. Future enhancements, including adding a telehealth indicator on the site, continue to be discussed.
The Managed Long-Term Care (MLTC) Performance Improvement Project (PIP) was extended until 12/31/21, due to the pandemic. During 2021 the EQRO conducted PIP progress calls with the plans, provided the call summary report to the DOH, and reviewed the MLTC plans PIP interim reports and provided feedback to the plans. The current PIP cycle will end at the end of 2021, and a new PIP cycle will begin, with a new PIP topic. The MLTC Technical Report/External Quality Review (EQR) Annual Technical Report (ATR) draft was being prepared by IPRO during 2021. During the 4th quarter, IPRO and DOH started weekly conference calls to discuss the development of the MLTC EQR ATR. A new report format will be used for the report. It was determined that MY 20202 and MY 2019 data will be used to populate the report.
The MLTC Satisfaction Survey was conducted in 2021. The survey closed in quarter 3. In the 4th quarter, the EQRO drafted the final report for the survey. The EQRO will provide DOH with the final report once it has gone through the EQRO's quality assurance review process.
The MLTC Encounter Data Validation Survey was conducted in 2021. An encounter validation survey was conducted for the mainstream MMC plans, and for the MLTC plans. For the mainstream portion of the Encounter Data Validation Survey, a final report was prepared by the EQRO and in the 4th quarter, the report went through OQPS' review/approval process and then OHIP's review approval process. For the MLTC survey, a final report was prepared by the EQRO in quarter 4, and the report was in their quality assurance review process.
The final report of the Child CAHPS survey was completed in the 3rd quarter of 2021 and in the 4th quarter the report was reviewed by the DOH legal dept and will be posted to the NYSDOH website after approval is given. In the4th quarter, preparations for the next survey, an Adult CAHPS survey, will be conducted.
On June 15, 2021, the Medicaid managed care plans submitted their annual QARR data submissions. During the 4th quarter the EQRO cleaned and analyzed the data and provided the DOH with the final QARR data files. In the 4th quarter of 2021, the EQRO will prepare for the next QARR submission, by preparing to conduct a WebEx on the QARR Technical Specifications Manual.
For 2021 DOH and the EQRO conduct bi-weekly planning and status calls to prepare for the MY/DY 2020 EQR ATR that is due to CMS in April 2022. In the 4th quarter and beyond, DOH is providing IPRO with data files that are necessary to populate the EQR ATR.
Performance Improvement Projects (PIPs) for Medicaid Managed Care Plans (MMC)
2017-18 HARP PIP
For the 2017-2018 Health and Recovery Plan (HARP) and HIV Special Needs Plan (SNP) PIP the selected common topic was Inpatient Care Transitions. Final reports for the 2017-18 HARP PIP projects were received in August 2019 and were finalized and approved in October 2019. A PIP Compendium of Abstracts was prepared by IPRO and was initially reviewed by the NYSDOH. Final edits were sent to IPRO in March 2021 and the revised version was received September 8, 2021 and is under review.
2019-2021 HARP PIP
The 2019-2021 HARP PIP topic is Care Transitions after Emergency Department and Inpatient Admissions. The HARP PIP Proposals were submitted December 21, 2018. The submitted PIP Proposals were reviewed and finalized by IPRO, NYSDOH and partners (including OASAS and OMH). Plan interventions began in early 2019. In June 2020 the MCOs were notified that the 2019-2020 PIPs were extended through December 31, 2021. Oversight calls were conducted in February 2021; May/June 2021; and Sept./Oct. 2021. The MCOs submitted a PIP Update Call Summary Report prior to the oversight calls. An Interim Report was due in February 2021. These were submitted by all plans and were finalized.
2019-2020 Medicaid KIDS Quality Agenda
The 2019-2020 Medicaid managed care (MMC) PIP topic is the KIDS Quality Agenda Performance Improvement Project. The overall goal of the PIP is to optimize the healthy development trajectory by decreasing risks for delayed/disordered development. The areas of focus for the PIP include screening, testing and linkage to services for lead exposure, newborn hearing loss and early identification of developmentally at-risk children. The PIP Proposals were due in the first quarter of 2019. The submitted PIP Proposals were reviewed and approved by IPRO and NYSDOH. In June 2020 the MCOs were notified that the 2019- 2020 PIPs were extended through December 31, 2021. Oversight calls were conducted in February/March/April 2021; July 2021; and November 2021. The MCOs submitted a PIP Update Call Summary Report prior to the oversight calls. An Interim Report was due March 8, 2021. These were submitted by all plans and were finalized. Plan-Specific Member Level Files for Lead Testing results data were sent from NYSDOH to the plans quarterly. The most recent Lead data was distributed to plans in September 2021. Plan Specific Member Level Files for Hearing Screening data were sent from NYSDOH to plans monthly. The most recent Hearing Screening data were distributed in September 2021.
Breast Cancer Selective Contracting
Staff completed the Breast Cancer Selective Contracting process for contract year 2021- 2022. This included: updating the computer programs used to extract and analyze inpatient and outpatient surgical data from the Statewide Planning and Research Cooperative System (SPARCS); identifying low-volume facilities for restriction; notifying restricted facilities of their status; conducting the appeals process; posting the list of restricted facilities to the NYS DOH public website; and, supplying the list of restricted facilities to eMedNY staff so that
Medicaid fee-for-service payments can be appropriately restricted, as well as, sharing the list with Medicaid managed care health plans' Chief Executive Officers and Medical Directors.
In total, the annual review identified 232 facilities. Facility designations were as follows: 113 high-volume facilities, 23 low-volume access facilities, and 96 low-volume restricted facilities.
Staff also completed the summer review of breast cancer surgical volume data. Provisional volume designations for contract year 2022-2023 were shared with facilities' SPARCS coordinators in September 2021. Release of these data will give facilities ample time to identify and correct any discrepancies between facility-calculated volume and SPARCS reported volume.
Patient Centered Medical Home (PCMH)
Federal Fiscal Quarter: 4 (7/1/2021-9/30/2021)
As of September 2021, there were 9,952 NCQA-recognized PCMH providers and 2,414 practices in New York State (NYS). All providers are recognized under the standards of NYS Patient-Centered Medical Home (NYS PCMH), a new recognition program that was released on April 1, 2018. NYS PCMH is based on NCQA PCMH 2017 recognition standards but requires NYS practices to meet a higher number of criteria to achieve recognition, with emphasis placed on behavioral health, care management, population health, value-based payment arrangements, and health information technology capabilities. Of the 9,952 providers that became recognized in September 2021, 67 were new to the NYS PCMH program.
Due to budget constraints, effective May 1, 2018, NYS discontinued PCMH incentive payments to providers recognized at level 2 under the 2014 standards, and reduced the incentive for 2014 level 3, and 2017-recognizerd providers. Current information on PCMH incentives in Medicaid can be found here.
The incentive rates for the New York Medicaid PCMH Statewide Incentive Payment Program as of September 2021 are:
- 2014 level 2: $0 PMPM
- 2014 level 3: $6.00 PMPM
- 2017 recognition: $6.00 PMPM
- NYS PCMH recognition: $6.00 PMPM
The Adirondack Medical Home demonstration (‘ADK'), a multi-payer medical home demonstration in the Adirondack region, has continued with monthly meetings for participating payers. There is still a commitment across payers and providers to continue through 2021 but discussions around alignment of methods for shared savings models are still not finalized.
All quarterly and annual reports on NYS PCMH and ADK program growth can be found on the NYSDOH website, available here.
Annual: 10/1/2020-9/30/2021
With the expiration of old 2014 and 2017 PCMH standards, the total number of recognized PCMH providers in New York State has slightly decreased throughout the year. In October 2020, there were 10,052 NCQA-recognized PCMH providers in New York State, this number slightly shrunk to 9,952 by the end of September 2021. The number of NCQA- recognized PCMH practices in New York State also decreased throughout the year, going from 2,724 in October 2020 to 2,414 in September 2021.
The first providers and practices achieved NYS PCMH recognition in July 2018. As of September 2021, 2,343 practices have achieved NYS PCMH recognition. From October 2020 to September 2021, the number of PCMH providers recognized under NYS PCMH standards increased from 8,949 (89. 03% of all PCMH recognized providers in NYS) to 9,952 (100%).
As of September 2021, incentive payments for NYS PCMH standards remain at $6.00 PMPM.
IX. Financial, Budget Neutrality Development/Issues
A. Quarterly Expenditure Report Using CMS-64
Quarterly budget neutrality reporting is up to date and on schedule. The State continues to work with CMS in resolving any emergent issues with the reporting template and PMDA system and in eliminating delays in the utilization of the Budget Neutrality Reporting Tool for quarterly reporting.
The State is also awaiting further guidance on two timely filing waivers submitted to correct reporting errors noted in previous quarterly reports. These expenditures, though not currently represented on the Schedule C, are included in the BN reporting tool workbook to accurately reflect the state's Budget Neutrality position:
- As detailed in STC X.10, the State identified a contractor, KPMG, to complete a certified and audited final assessment of budget neutrality for the October 1, 2011 through March 31, 2016 period. The audit was completed over the summer of 2018. A final audit report was submitted to CMS on September 19, 2019, with CMS confirming in a subsequent discussion on October 10, 2019, that all corrective action requirements outlined in the STCs have been satisfied. The State has addressed all audit findings, however, entry of corrected data for F-SHRP DY6 into MBES is pending approval of a timely filing waiver.
- The State has also requested a timely filing waiver to address an issue with reporting for DY18 Q1-4 and DY19 Q1 resulting from an error in the query language used to pull data for this time period which resulted in the exclusion of F-SHRP counties for these quarters. This error was not uncovered until all DY18 quarters were processed, allowing for comparisons to previous full data years that had already been reported, and the source of the issue was not identified until DY19Q1 was already processed.
X. Other
A. Transformed Medicaid Statistical Information Systems (T-MSIS)
NYS Compliance
The State sends the following files to CMS monthly:
- Eligibility
- Provider
- Managed Care
- Third Party Liability
- Inpatient Claims
- Long-Term Care Claims
- Prescription Drug Claims
- Other Types of Claims
The State is current in its submission of these files. Moreover, New York State is actively working on addressing the Top 32 Priority Issues (TPIs) identified and prioritized by CMS for 2021. New York stands in the highest compliance category (Blue) for the TPIs 1 through 23 as defined by CMS for 2021. The state has also begun aligning with and addressing the issues associated with the new Measure Based Assessment Compliance Criteria proposed by CMS for 2022.
New York State continues to work closely with CMS and its analytics vendors to define, identify and prioritize new issues.
To help facilitate resolution of identified data issues, the state has instituted a Data Governance workgroup for T-MSIS. The group's focus is to address data issues and specific processes/policies that are unique to NY and provide narration to aid in the understanding of these state processes/policies.
The State has started resubmitting historical claim files for the period July 2015 through June 2021 per CMS's request.
B. 1115 Waiver Public Comment Days
With the implementation of the Medicaid Redesign Team in 2011, New York has prioritized transparency and public engagement as a key element of developing and implementing Medicaid policies. The public comments provided at these forums have been shared with the New York teams working on these programs and has informed implementation activities. We will continue to consider these issues and engage stakeholders as part of our ongoing efforts.
On January 21, 2021, the Department of Health conducted a virtual public hearing/public forum. A second virtual public hearing/public forum was held on January 27, 2021.
A recording of the live webcasts, transcript, and presentation slides from each public hearing/public forum are available here. All written public comments received are shared with the program areas within the State for their consideration in shaping policy and procedures.
Attachments:
Attachment 1– MLTC Critical Incidents
Attachment 2– MLTC Partial Capitation Plan, PACE, and MAP Enrollment
State Contact:
Phil AlottaAssociate Health Planner
Division of Program Development and Management
Office of Health Insurance Programs
phil.alotta@health.ny.gov
Phone (518) 486-7654
Fax# (518) 473-1764
Submitted via email: December 2, 2021
Uploaded to PMDA: December 2, 2021
Critical Incidents
Plan Name Number of Critical Incidents Wrongful Death Use of Restraints Medication errors that resulted in injury Instances of Abuse, Neglect and/or Exploitation of Enrollees Involvement with the Criminal Justice System Other Incident Resulting in Hospitalization Other Incident Resulting in Medical Treatment Other than Hospitalization Any Other Incidents as Determined by the Department Enrollment Critical Incidents as a Percentage of Enrollment Aetna Better Health 3 0 0 0 0 0 2 1 0 5,919 0.10% AgeWell NY 17 0 0 1 3 6 3 4 0 12,948 0.26% Agewell MAP 0 0 0 0 0 0 0 0 0 55 0.00% Archcare Community Life 51 0 0 1 8 0 27 15 0 4,582 2.23% Archcare PACE 17 0 0 0 1 0 7 9 0 729 4.66% Catholic Health-LIFE 21 0 5 0 0 0 4 9 3 261 16.09% Centerlight PACE 39 0 0 0 1 0 17 15 6 2446 3.19% Centers Plan for Healthy Living 289 3 0 0 31 0 100 155 0 45,038 1.28% Centers Plan for Healthy Living MAP 9 0 0 0 0 0 4 5 0 653 2.76% Complete Senior Care 1 0 0 0 0 0 1 0 0 126 1.59% Eddy SeniorCare 7 0 0 0 0 0 3 4 0 295 4.75% Elant Choice (EverCare) 34 0 0 0 2 0 7 22 3 1,001 6.79% Elderplan MAP 0 0 0 0 0 0 0 0 0 2,802 0.00% Elderserve MAP 0 0 0 0 0 0 0 0 0 69 0.00% Elderserve 254 0 0 0 2 3 102 147 0 15,342 3.31% Elderwood 28 0 0 0 0 0 9 19 0 1,009 5.55% Empire BlueCross BlueShield Healthplus 2 0 0 0 0 0 0 0 2 5,218 0.08% Empire BlueCross BlueShield Healthplus MAP 0 0 0 0 0 0 0 0 0 102 0.00% Extended 60 0 0 0 2 3 35 20 0 5965 2.01% Fallon Health (TAP) MLTC 0 0 0 0 0 0 0 0 0 875 0.00% Fallon Health (TAP) PACE 0 0 0 0 0 0 0 0 0 127 0.00% Fidelis Care at Home 2 0 0 0 0 0 2 0 0 19,392 0.02% Fidelis MAP 0 0 0 0 0 0 0 0 0 120 0.00% Hamaspik 27 0 0 0 2 2 13 9 1 2,059 2.62% Hamaspik MAP 0 0 0 0 0 0 0 0 0 88 0.00% Healthfirst CompleteCare 0 0 0 0 0 0 0 0 0 19,390 0.00% HomeFirst, Inc. (Elderplan) 0 0 0 0 0 0 0 0 0 13794.7 0.00% Icircle 0 0 0 0 0 0 0 0 0 3,701 0.00% Independent Living for Seniors (ILS/ElderOne) 0 0 0 0 0 0 0 0 0 729 0.00% Independent Living Services of CNY (PACE CNY) 19 0 0 0 0 0 11 8 0 562 6.76% Integra MLTC 1 1 0 0 0 0 0 0 0 39,758 0.01% Kalos ErieNiagara DBA: First Choice Health 2 0 0 0 0 0 2 0 0 678 0.59% MetroPlus 0 0 0 0 0 0 0 0 0 1,435 0.00% Monefiore 0 0 0 0 0 0 0 0 0 1,521 0.00% Prime 60 0 0 0 0 5 13 39 3 590 20.34% Senior Health Partners 87 0 0 0 1 1 31 54 0 10,745 1.62% Senior Network Health, LLC 11 0 0 0 0 0 4 7 0 390 5.64% Senior Whole Health 1 0 0 0 0 1 0 0 0 13,673 0.01% Senior Whole Health MAP 0 0 0 0 0 0 0 0 0 118 0.00% Total Senior Care 5 0 0 0 0 0 0 5 0 144 6.94% Village Care 243 0 0 0 27 2 54 160 0 13,315 3.65% Village Care MAP 92 0 0 0 13 1 22 56 0 3,038 6.06% VNA Homecare Options (Nascentia Health Options) 0 0 0 0 0 0 0 0 0 3,309 0.00% VNS Choice MAP TOTAL 27 0 0 0 10 0 6 11 0 3,130 1.73% VNS Choice MLTC 192 0 0 2 37 1 55 97 0 21,819 1.76% Total: 2818 1409 4 5 2 103 24 479 774 18 MLTC Partial Capitation Plan Enrollment
Managed Long Term Care Partial Capitation Plan Enrollment October 2020 - September 2021 Plan Name Oct-20 Nov-20 Dec-20 Jan-21 Feb-21 Mar-21 Apr-21 May-21 Jun-21 Jul-21 Aug-21 Sep-21 Enrollment Enrollment Enrollment Enrollment Enrollment Enrollment Enrollment Enrollment Enrollment Enrollment Enrollment Enrollment Aetna Better Health 6,708 6,585 6,496 6,415 6,322 6,257 6,116 6,071 6,023 5975 5909 5,872 AgeWell New York 12,089 12,123 12,312 12,442 12,453 12,558 12,532 12,616 12,739 12825 12954 13,065 ArchCare Community Life 4,525 4,526 4,556 4,564 4,518 4,524 4,507 4,518 4,538 4565 4590 4,592 Centers Plan for Healthy Living 42,574 42,937 43,344 43,360 43,333 43,623 43,694 44,141 44,448 44701 44993 45,421 Elant 1,106 1,099 1,101 1,083 1,065 1,066 1,046 1,054 1,034 1012 999 991 Elderplan 14,280 14307 14465 14259 14061 14008 13,824 13,831 13,826 13808 13781 13,792 Elderserve 15,154 15,181 15,268 15,305 15,159 15,113 15,033 15,132 15,200 15266 15335 15,425 Elderwood 913 905 913 946 943 973 967 992 1,005 1005 1009 1,012 Extended MLTC 6,602 6,596 6,558 6,538 6,467 6,420 6,234 6,094 6,035 5993 5970 5,931 Fallon Health Weinberg (TAIP) 904 890 887 871 865 858 846 860 868 872 872 881 Fidelis Care at Home 21,494 20,732 20,665 20,516 20,174 20,085 19,703 19,664 19,588 19474 19398 19,303 Hamaspik Choice 2,151 2,118 2,138 2,135 2,114 2,112 2,063 2,044 2,047 2045 2064 2,068 HealthPlus-Amerigroup 5,830 5,802 5,748 5,686 5,591 5,517 5,413 5,401 5,315 5268 5226 5,159 iCircle Services 3,929 3,834 3,826 3,823 3,799 3801 3,735 3,747 3,714 3706 3703 3,693 Integra 33,820 35269 36786 37535 37960 38,400 38,526 38,870 39,180 39457 39776 40,041 Kalos Health-Erie Niagara 936 872 842 825 792 772 724 709 704 690 680 663 MetroPlus MLTC 1,630 1,606 1,606 1,586 1,547 1,518 1,483 1,491 1,473 1448 1427 1,429 Montefiore HMO 1,607 1,592 1,595 1,584 1,550 1,535 1,525 1,532 1,532 1525 1522 1,517 Prime Health Choice 593 598 615 614 616 625 627 624 617 612 578 580 Senior Health Partners 13,104 13,085 13,045 12,573 12,202 11,929 11,526 11,381 11,180 10946 10719 10,570 Senior Network Health 423 423 424 424 413 409 403 406 402 393 392 386 Senior Whole Health 13,062 13,094 13,193 13,222 13,313 13,394 13,339 13,428 13,541 13645 13673 13,702 Village Care 13,012 13,242 13,400 13,161 13,092 13,080 12,967 13,011 13,097 13151 13358 13,436 VNA HomeCare Options 3,449 3,248 3,283 3,286 3,284 3,290 3,199 3,214 3,262 3286 3313 3,329 VNS Choice 20,581 20,775 21,136 16,289 21,219 21,350 21,281 21,393 21,593 21699 21808 21,951 Total 240,476 241,439 244,202 239,042 242,852 243,217 241,313 242,224 242,961 243,367 244,049 244,809 MAP Enrollment October 2020 - September 2021 Fidelis 66 67 63 63 60 59 58 72 78 106 117 138 Hamaspik 0 0 0 0 0 0 0 0 0 37 92 135 Agewell 22 20 20 24 25 38 44 51 53 53 55 58 Centers 21 21 21 162 528 402 435 1032 1126 612 659 687 Elderplan 2247 2222 2199 2418 2465 2475 2606 2685 2730 2771 2801 2833 Elderserve 29 31 32 44 51 61 63 64 66 69 67 72 Healthfirst Complete Care 15055 15053 15122 16107 16556 17160 17655 18144 18629 19019 19406 19746 Healthplus 11 11 11 11 8 27 64 63 82 88 100 117 Senior Whole Health 132 129 127 125 120 119 114 115 112 117 118 119 VNS 3111 3092 3066 3105 3050 3020 3014 3035 3088 3122 3127 3141 Village Care 2439 2373 2317 2613 2701 2794 2882 2949 3001 3024 3047 3043 Total 23133 23019 22978 24672 25564 26155 26935 28210 28965 29018 29589 30089 PACE Plan Enrollment October 2020 - September 2021 Archcare 739 748 745 726 715 702 692 731 751 747 741 699 CHS Buffalo Life 273 271 267 255 249 250 250 253 253 256 262 265 Complete Senior Care 127 131 130 130 126 126 125 126 127 125 127 126 Comprehensive Care Management 2474 2448 2446 2433 2408 2360 2402 2372 2378 2386 2435 2518 Eddy Senior Care 300 296 301 303 293 294 294 295 295 297 296 293 Fallon Health Weinberg PACE 150 150 151 144 141 139 131 132 131 132 125 125 Independent Living For Seniors 757 760 769 763 744 733 736 732 726 730 729 728 Pace CNY 609 606 600 611 578 580 574 568 568 567 561 559 Total Senior Care 139 142 143 143 137 137 139 143 140 143 144 144 Total 5568 5552 5552 5508 5391 5321 5343 5352 5369 5383 5420 5457 MA Plan Enrollment October 2020 - September 2021 Fidelis Legacy 1150 1148 1136 1122 1089 1063 1041 1045 1030 1009 999 983 Wellcare 1108 1103 1122 1030 992 953 926 900 882 862 859 846 United Healthcare 1278 1269 1262 1254 1242 1232 1215 1205 1191 1177 1164 1156 Total 3536 3520 3520 3406 3323 3248 3182 3150 3103 3048 3022 2985 FIDA-IDD Enrollment October 2020 - September 2021 Partners Health Plan 1750 1754 1757 1746 1748 1743 1740 1738 1744 1734 1724 1720
Follow Us