Nursing Home Transition and Diversion (NHTD) Waiver
Eligibility Criteria
- Overview is also available in Portable Document Format (PDF)
An individual applying to participate in the NHTD waiver must meet all of the following criteria:
- Be a recipient of Medicaid coverage that supports community–based long–term care services. Such coverage includes:
- All Services except Nursing Facility Service
- Community Coverage with Community–Based Long Term Care
- Outpatient Coverage with Community–Based Long Term Care
- Outpatient Coverage with no Nursing Facility Services
- Be between the ages of 18 and 64 with a physical disability, or age 65 and older upon application to the waiver; If under age 65, the physical disability will be documented by:
- Award letters/determination of:
- Supplemental Security Income (SSI);
- Social Security Disability Insurance (SSDI); or
- Railroad Retirement letter for total permanent disability for SSI benefits.
- A letter from the Local Department of Social Services or local disability team (form LDSS 4141) stating the individual has been determined to have a physical disability;
- Documentation from the individual´s physician, hospital summaries or Nursing Home records verifying the physical disability.
- Award letters/determination of:
- Be assessed to need a nursing home level of care. Nursing home eligibility is determined by the Hospital and Community Patient Review Instrument and SCREEN (H/C PRJ and SCREEN) if the individual is in a hospital or nursing facility and will be reassessed within ninety days (90) of enrollment in the waiver utilizing the Uniform Assessment System for New York (UAS–N Y). For individuals in the community, the UAS–NY will be used to assess nursing facility level of care. The form must be dated with in ninety (90) calendar days prior to the Effective Date of the Notice of Decision and be completed by an individual certified by the State of New York to administer the tool;
- Sign the Freedom of Choice form indicating whether he/she chooses to participate in the NHTD waiver;
- Be able to identify the actual location and living arrangements in which the waiver participant will be living when participating in the waiver;
- Complete and submit an Application Packet which includes the Initial Service Plan in cooperation with the Service Coordinator. This Initial Service Plan must describe why the individual is at risk for nursing home placement without the services of the waiver and indicate how the available supports and requested waiver services identified in the Plan and how the use of the waiver services will prevent institutionalization. The potential applicant must need at least one waiver service;
- Have a completed Plan for Protective Oversight (PPO). Be capable of directing his/her Service Plan or has a legal guardian available to direct the participant´s Service Plan;
- Services agreed upon in the Initial Service Plan (ISP) must meet regional and statewide cost neutrality; and
- Be able to live in the community where health and welfare can be maintained as determined by the Regional Resource Development Specialist
Participant Enrollment Information
NHTD Waiver Enrollment by Region as of August 2015
| Region | Active Participants |
|---|---|
| Adirondack | 379 |
| Binghamton | 199 |
| Buffalo | 260 |
| Capital | 195 |
| Long Island | 168 |
| Lower Hudson Valley | 261 |
| New York City | 339 |
| Rochester | 301 |
| Syracuse | 155 |
| TOTAL | 2257 |
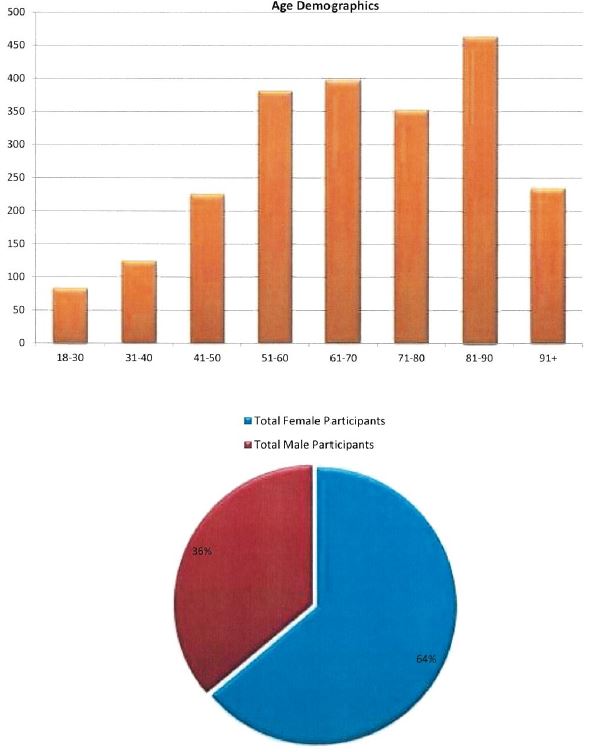
NHTD Active Participant Demographics
As of 08/14/2015
Follow Us