Rate Setting for Transition into Managed Care
Division of Finance and Rate Setting
- Presentation is also available in Portable Document Format (PDF)
Torrey Duchessi
Michael Dembrosky
November 16, 2016
NHTD/TBI Waiver Transition Workgroup Meeting
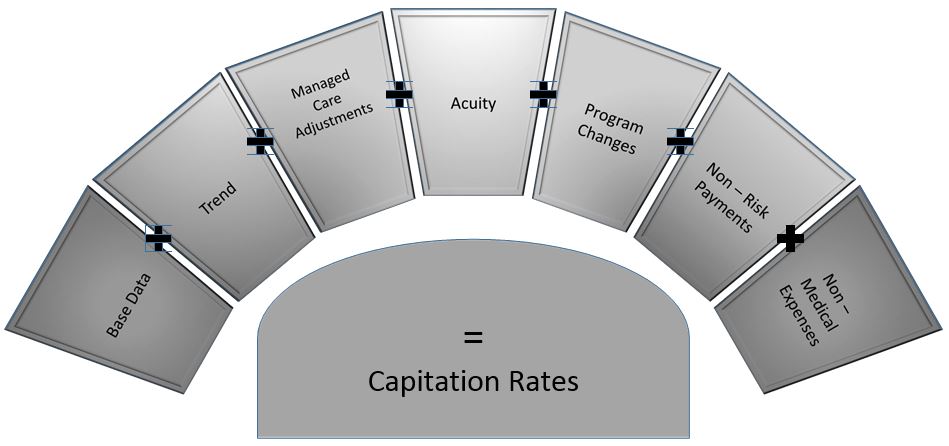
Rate Setting Guiding Principles
- Capitation rates should match payment to risk.
- Capitation rates should promote cost containment and quality health outcomes.
- Capitation rates should provide a fair and reasonable level of reimbursement for the contracted health plans.
- Capitation rates should support budget predictability.
- The methodology for developing capitation rates should be sufficiently flexible so that it can be readily adapted to fit with the State's vision for Medicaid Managed Care over the next three to five years.
- The capitation rates should appropriately reflect the states operational and/or resource realities.
- To the extent that it is feasible and practical, the process for developing capitation rates should be a collaborative effort between Mercer, the State and the contracted plans.
Base Data
| MMC |
MLTC |
- 2 years of Medicaid Managed Care Operating Report (MMCOR) data is used to develop the region average base premiums.
- Data is split by:
- Region
- Category of Aid (COA)
- Age
- Non–maternity (Core), maternity and birth
- Base is adjusted for Plan reported Incurred But Not Reported (IBNR) expenditures.
|
- 2 years of Medicaid Managed Care Operating Report (MMCOR) data is used to develop the region average base premiums.
- Data is split by:
- Base is adjusted for Plan reported Incurred But Not Reported (IBNR) expenditures.
|
Trend
| MMC |
MLTC |
- Adjusts MMCOR base data to reflect contract period
- Applied from midpoint of base to midpoint of contract period
- Applied by COA and Region
- Reflects changes in utilization, inflation, changes in mix of services, other market forces that impact Health Plans
- Applied to CORE and Optional services
|
- Adjusts MMCOR base data to reflect contract period
- Applied from midpoint of base to midpoint of contract period
- Applied by COA and Dual Status
- Reflects changes in utilization, inflation, changes in mix of services, other market forces that impact Health Plans
- Applied to LTC services and Care Management
|
Managed Care Adjustments
| MMC |
MLTC |
- Managed care plans are expected to reach certain levels of efficiency.
- Efficiency adjustment is used to value the amount of various preventable events.
- Behavioral Health Organizations/ Health and Recover Plans (BHO/HARP) adjustment reflects differences between the fee for service (FFS) and MMC delivery system.
|
- The mandatory MLTC rate adjustment reflects differences between the fee for service (FFS) and MLTC delivery system.
|
Acuity
| MMC |
MLTC |
- All plans are paid the same regional average premium, adjusted by a plan specific risk adjustment factor (risk score) that accounts for differences in enrollee acuity across plans.
- Risk Scores are calculated using the Clinical Risk Group (CRG) model developed by 3M and CRG cost weights are developed by DOH.
- Plan specific risk scores are calculated relative to the regional average.
|
- All plans are paid the same regional average premium, adjusted by a plan specific risk adjustment factor (risk score) that accounts for differences in enrollee acuity across plans.
- Risk Scores are calculated using the regression model based on the Uniform Assessment System (UAS).
- Plan specific risk scores are calculated relative to the regional average.
|
Non – Risk Payments
| MMC |
MLTC |
- Quality Incentive
- Patient Centered Medical Home
|
- Quality Incentive
- Recruitment, Training and Retention (RTR)
|
Non – Medical Expenses
| MMC |
MLTC |
- Administration
- Underwriting Gain
- Applicable Taxes
|
- Administration
- Underwriting Gain
- Applicable Taxes
|
Finalizing of Premiums
- Premiums are certified by an independent actuary before being presented to the Centers for Medicare and Medicaid Services (CMS) and the New York State Division of Budget (DOB) for approval.
- DOH and its actuary are currently evaluating how the Managed Care Final Rule applies to the existing premium rate setting methodology.
- Once appropriate approvals are received, the premiums are loaded to the State's fiscal agent, eMedNY for payment to plans.
Questions?
Follow Us