New York Association on Independent Living
- This Presentation is also available in Portable Document Format (PDF)
Nursing Home Transition and Diversion (NHTD) Waiver and Traumatic Brain Injury (TBI) Waiver Transition to Managed Care Workgroup Meeting
Rebecca Corso, Deputy Director, Division of Long Term Care
Office of Health Insurance Programs
New York State Department of Health
November 30, 2015
Medicaid Redesign Background
- In keeping with the Medicaid Redesign Team (MRT) goal of Care Management for All, the state plans to transition the Nursing Home Transition and Diversion (NHTD) and Traumatic Brain Injury (TBI) waiver participants into managed care programs.
- The Care Management for All approach will improve benefit coordination, quality of care, and patient outcomes over the full range of health care, including mental health, substance abuse, developmental disability and physical health care services.
- To receive long term care services, as well as to continue receiving current benefits received through the waivers, current NHTD/TBI participants will be offered a managed care program:
- Managed Long Term Care (MLTC), or
- Medicaid Managed Care (MMC).
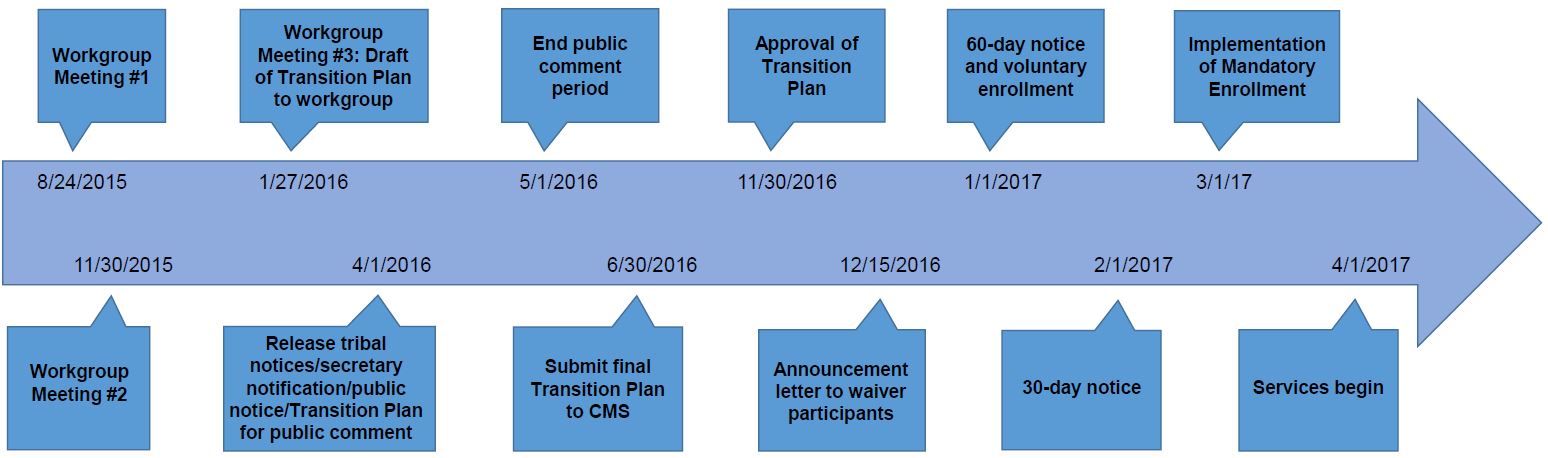
Draft NHTD/TBI Transition Timeline
Workgroup Update
- The workgroup commenced on August 24, 2015. As a result of this meeting, four subcommittees were formed:
- Services and Workforce Qualifications;
- Outreach and Education;
- Uniform Assessment System (UAS–NY); and
- Finance and Rates.
- The meeting minutes are available on the MRT 90 website
Subcommittee Update
- A meeting of the four subcommittees was held on October 6, 2015.
- The Services and Workforce Qualifications subcommittee also met on October 23, 2015, and November 6, 2015, to continue the discussion on services and qualifications.
- These meeting minutes are also available on the MRT 90 website.
Services & Workforce Qualifications Update
- This subcommittee focused on the following:
- NHTD and TBI services that would transition to MMC and MLTC
- Continuity–of–care for waiver participants and providers
- Services:
- The proposed action is to transition NHTD/TBI benefits not currently included in the MMC and MLTC benefit packages with a few exceptions.
- Home Visits by Medical Personnel
- Peer Mentoring
- To address the issue of Peer Mentoring, workgroup member Lindsay Miller, Executive Director of the New York Association on Independent Living, will speak on one type of peer services already available in the state.
- The proposed action is to transition NHTD/TBI benefits not currently included in the MMC and MLTC benefit packages with a few exceptions.
- In order to get these services, after the transition occurs, new individuals must continue to meet waiver eligibility.
- The Regional Resource Development Center (RRDC) will continue to have a role in the coordination of services including, but not limited to, Service Coordination and other non–State Plan services.
- Service coordination will be afforded as a benefit in addition to care coordination, based on need.
- In order to receive service coordination, participants must have a:
- Nursing Home Level of Care, plus
- a diagnosed moderate cognitive impairment.
- Continuity–of–care:
- The Department is proposing to establish a two–year continuity–of–care period for participants and service providers.
- As a result, Managed Care Organizations will be required to contract with current service providers for a minimum of two years:
- If the service provider is serving five or more current waiver participants;
- If the service provider continues to serve participants unless a health/safety concern exists; and
- As long as the service provider assures that there are appropriately licensed personnel to provide and/or supervise services.
- Current waiver participants:
- Will have the choice to maintain his/her existing services and the providers of these services for 90 days.
- Will have the option to keep the same providers for up to two years, if his/her needs remain the same after the 90 days, and if the provider meets the conditions above.
Outreach & Education Update
- This subcommittee discussed the role of New York Medicaid Choice (Maximus) as the enrollment broker through the transition process:
- Education will be involved to address the extended needs of the population.
- Outreach includes face–to–face education at the local level and phone support through call centers.
- The call center has multiple language lines and contracts with a translation company.
- Outreach calls/follow–up assistance calls continue throughout the timeline of the transition.
- DOH will train Maximus to effectively work with these specific populations.
- Maximus requires its employees to complete training and also provides written training materials.
UAS–NY Update
- This subcommittee presented a review of the UAS–NY.
- The UAS–NY shows the level of functioning and provides information for assessors to analyze and make decisions based on the outcomes.
- The required UAS–NY training for assessors was discussed.
- DOH will continue to utilize the UAS–NY.
Finance & Rates Update
- A review of the DOH process for rate setting was presented.
- Rates are determined by looking at trends in the base data (per region). Base data is reviewed in depth with the plans, DOH and Mercer (actuary).
- Once established, base rates are updated annually, or as necessary due to program changes.
- DOH made a two–year commitment to maintaining the current reimbursement that NHTD and TBI providers currently receive in the fee–for–service system.
- Additional discussion will be needed, based on the recommendations of additional benefits to the MMC and MLTC benefits packages and its impact on the 1115 waiver budget neutrality requirement.
Other Considerations
- Current housing subsidy:
- DOH has committed to maintaining the housing subsidy for individuals who are receiving a subsidy at the time of transition.
- The subcommittee discussed that housing is not a discrete waiver service and thus will not be outlined in the transition plan.
- The subcommittee agreed that housing is a broader issue that should be discussed with the MRT Supportive Housing Team.
- Community First Choice Option (CFCO) – Offers similar services and the eligibility requirement is Nursing Home Level of Care. More information on the approved New York State Plan Amendment is available here.
- Home and Community–Based Services (HCBS) Settings Transition Plan
- Amendments to the 1115 Waiver will also be needed after the Transition Plan is approved by CMS.
Next Steps
- If needed, hold additional subcommittee meetings.
- The Department will develop a draft Transition Plan based on the feedback and comments received to date.
- The Department will share the Transition Plan with the full workgroup at the next meeting to be held on January 27, 2016.
QUESTIONS?
Contact Us:
Transition questions may be emailed to: Waivertransition@health.ny.gov
Follow Us