Transition (Carve-Out) of Pharmacy Benefit from Managed Care to Fee-For-Service (FFS)
All Stakeholder: Implementation Update
- Presentation also available in Portable Document Format (PDF)
October 19, 2020
Overview
Project Overview
- Transitioning pharmacy services from Managed Care to fee-for-service (FFS) will, among other things, do the following:
- Provide the State with full visibility into prescription drug costs.
- Centralize and leverage negotiation power.
- Provide a single drug formulary with standardized utilization management protocols.
- Address the growth of the 340B program and associated reductions in State rebate revenue.
Stakeholder Engagement Update
All Stakeholders: Monthly
Purpose:
NYS DOH will lead and provide all interest stakeholders with updates, facilitate a Q&A session, and incorporate feedback into the workplan as needed.Status:
- Monthly meetings ongoing starting with July 13 session
- Remaining meetings scheduled for third Monday of each month
Technical Workgroup: Bi-weekly
Purpose:
NYS DOH is leading working sessions with Medicaid Managed Care Plans (and other subject matter experts as needed) to address transition topics and incorporate feedback into the workplan as needed.Status:
- Sessions 1-5 complete covering Roles & Responsibilities, Scope of Benefits, Data Sharing, Transition Strategy, Member & Provider Communication, Value-Based Payments, QARR Measures, and Program Integrity
- Next three sessions will address Data File, Access & Reports; DME Supplies and Model Contract
340B Advisory Group: Four Meetings
Purpose:
Provide non-binding recommendations by October 1, 2020 regarding the reimbursement of 340B claims.Status:
- Three meetings held on 8/5, 8/26, and 9/16. An additional meeting will be held, per the request of the Advisory Group (data TBD).
- Several ideas have been suggested and discussed. DOH will evaluate final recommendations for alignment with Goals and Expectations and update work plan if necessary.
Transition & Communications Strategy
Transition Guiding Principles
Continuity
Ensure members are provided with continued access to needed medications and supplies with minimal impact.
- Comparison of FFS pharmacy claims, and Medicaid Managed Care pharmacy encounters will inform our transition strategy.
Communication
Maintain communication with stakeholders (e.g. providers, patient advocates, and Principles Communication Managed Care Plans).
- Recurring stakeholder meetings
- Pertinent information posted on the Department of Health (DOH) website.
Oversight
Utilize "post implementation" processes that ensure appropriate oversight, issue identification, tracking and resolution.
Smoothing The Transition
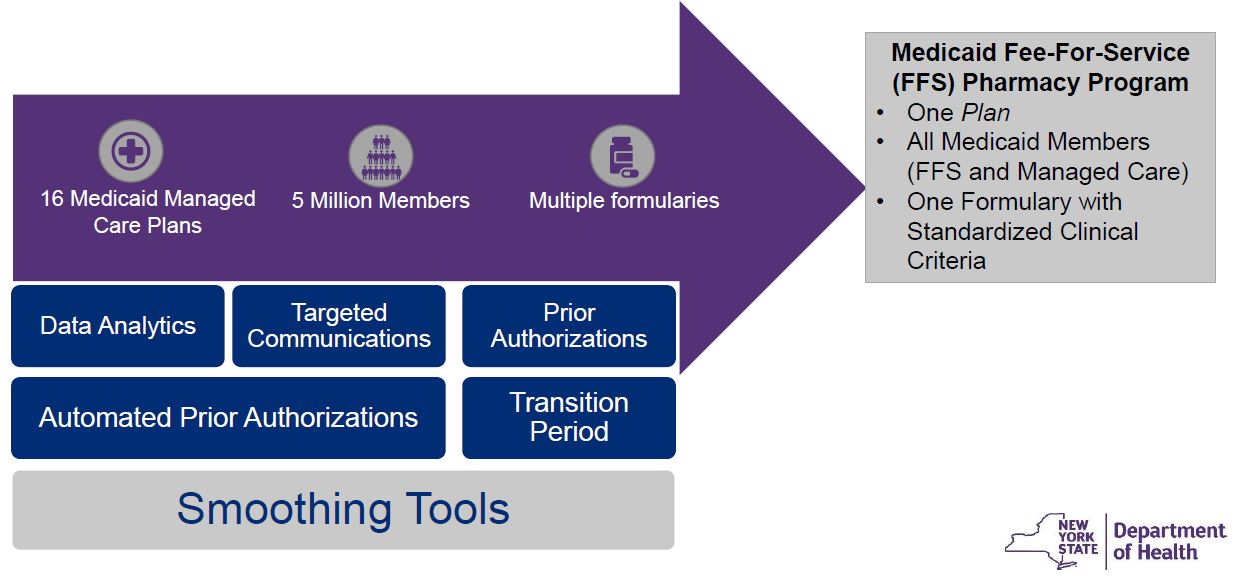
Tools to Smooth the Transition
- Transition Period: Between April 1, 2021 through June 30, 2021, members can obtain a one- time fill for non-preferred FFS medications without prior authorization.
- Prior Authorizations (PAs): PAs previously authorized by plans will be recognized/honored in FFS.
- Automated PA: PAs will be automatically bypassed when information in managed care claims history meets PA requirements (e.g. right diagnosis).
- Data Analytics: Managed Care claim analysis by focus area or program (e.g. Preferred Drug and Diabetic Supply Programs) will inform communication and transition activities.
- Targeted Communications: Will be used to notify members and providers of actions that can be taken to smooth the transition.
Pharmacies & Prescribers
Analysis: Identify pharmacies and prescribers that are serving Medicaid Managed Care members that are not enrolled in the Medicaid FFS program
| Provider Type | % Claims with FFS enrolled Providers |
|---|---|
| Pharmacies | 97% |
| Prescribers | 93% |
Smoothing Tools
- Notice to pharmacies and prescribers of the need to enroll in Medicaid FFS.
- Work with Managed Care Plans to encourage Medicaid FFS enrollment.
- Focused outreach with specific instruction based on provider´s status (e.g. pharmacies that are enrolled as Managed Care only and previously enrolled FFS prescribers)
Based on Q2 2020 data
Preferred Drug and Diabetic Supply Programs (PDP and PDSP)
Analysis: Identify products that are currently being used by Managed Care Members that are not preferred in FFS
| Program | % Claims That Match FFS Preferred Products |
|---|---|
| Preferred Drug Program (PDP) | 91% |
| Preferred Diabetic Supply Program (PDSP) (Meters & Test strips)* | 97% |
*50% of claims that do not match FFS Preferred Products are for acute medications.
** FFS Non preferred products are isolated to a single manufacturer.
Smoothing Tools
- Targeted Outreach/Education will be conducted to publicize the PDP/PDSP list of preferred products.
- One-time transition fill will be provided for non-preferred products during the transition period 4/1/21-6/30/21.
Based on Q1 2020 Data
Practitioner Administered Drugs
Analysis: Identify practitioner administered drug claims for Managed Care members that are not open on the Medicaid FFS formulary
| Specialty High Cost Drugs | # of Claims | % of Claims not on the Medicaid FFS Outpatient Formulary |
|---|---|---|
| High Cost, requires monitoring, special handling. Ex: IV immunotherapy, chemotherapy, etc. | 356,001 | 2% |
| Low Cost Drugs | # of Claims | % of Claims not on the Medicaid FFS Outpatient Formulary |
|---|---|---|
| Non-specialty physician administered, acute use. Ex: IV antibiotics, heparin, etc. | 19,022 | 5% |
Transition Strategy
- Practitioner Administered Drugs not open on the Medicaid FFS outpatient formulary will continue to be made available by the Medicaid Managed Care Plans via the medical benefit.
- The Department will continue to analyze these medications and where appropriate and may make additions to the Medicaid FFS outpatient formulary.
Based on Q2 2020 Data
Durable Medical Equipment (DME) & Supplies
Analysis: Identify claims for managed care members for products that are not currently covered under the Medicaid FFS Pharmacy Program
| DME & Supplies | % of Claims Covered under the Medicaid FFS Pharmacy Program |
|---|---|
| Claims | 99% |
Transition Strategy
- The Department had been working with our Managed Care Plan partners to identify DME/supplies that are not a covered benefit in Medicaid FFS.
- The Department is reviewing some items for possible inclusion on the Pharmacy Procedures and Supplies list of products.
Based on Q2 2020 Data
Communication Plan
|
Medicaid Update | October 2020 | Informs pharmacies, prescribers and Durable Medical Equipment (DME) Providers that if they are not enrolled in Medicaid Fee-For-Service (FFS), they must enroll to continue to serve Medicaid Managed Care members effective 4/1/2021. |
|
Medicaid Update | December 2020 & February 2021 | Provides information regarding the Medicaid Formulary and Prior Authorization (PA) Programs, which includes the Preferred Drug Program (PDP) Preferred Diabetic Supply Program (PDSP). |
|
Prescriber Outreach | March 2021 | Conduct prescriber outreach activities targeted to inform high volume prescribers of non-preferred products of the carve-out impact and actions that can be taken to smooth the transition (e.g. change to a preferred product or seek prior authorization) |
|
Custom Member and/or Prescriber Notifications | April - June 2021 | Prescribers and members will be notified of their patients that are on non-preferred drugs. Guidance will be provided regarding the one-time transition fill, alternative drugs, and the prior authorization process. |
Key Deliverables and Timeline Update
Key Deliverables and Timeline Update
| Deliverable(s) | Target Date |
|---|---|
| Complete Work Plan and Establish State Transition Team and 340B Advisory Group | June 2020 ✔️ |
| Recurring Workgroup Calls with Health Plans and All Stakeholders begin | July 2020 ✔️ |
| Frequently Asked Questions Posted to the NYS DOH Website | August 2020* ✔️ |
| Finalize NYS DOH/Managed Care Plan Roles and Scope of Benefits | September 2020 ✔️ |
| Consensus between the state and plans on data sharing concept | October 2020 |
| Recommendations from 340B Advisory Group | October 2020 |
| Changes to Model Contract Identified | November 2020 |
| Transition Analysis Conducted (e.g., Formulary, DME, OTC Comparisons), Changes Made To Smooth Transition and Transition Strategy Finalized | November 2020 |
| Deliver file formates, data dictionary, and process for daily claim file | November 2020 |
| Notice of 1115 Waiver Amendment | December 2020 |
| Required System Changes Identified and Implemented | December 2020 |
| 340B Related State Plan Amendment (SPA) Submitted | December 2020 |
| Initial Special Edition Medicaid Update Published | December 2020 |
| Systems Stress Testing Performed | January 2021 |
| Member and Provider Notifications Sent and Second Special Edition Medicaid Update Published | February 2021 |
| Customer Service Staff Hired and Trained | February 2021 |
| Make Required Changes to Common Benefit Identification Card (CBIC), Carrier or Notice | March 2021 |
| 1115 Waiver Amendment and SPA Approved by CMS | March 2021 |
| Go Live: Daily Calls with Stakeholders (through 4/30/2021 or Beyond as Needed) | April 2021 |
Communications and Resources
Website Updates
- The following content has been added to the website since the last meeting:
- All Stakeholder September 21 Presentation
- FAQ Update - October 9, 2020
- Transition & Communications Activities Timeline
- Website updates will continue to be communicated via the MRT listserv.
Resource Spotlight: Materials Posted
Resources and materials will be updated and clarified based on stakeholder feedback
- 12 New FAQs added October 9, 2020 to address:
- Questions submitted in the September All Stakeholder session
- Questions submitted to the PPNO mailbox
- Questions posed in other venues and received through other channels that will be helpful to a wider audience
- FAQ Update – Updated categories include:
- General
- 340B
- Managed Care Plans (MCPs)
- Scope of Benefits
- Data Sharing
FAQ Spotlight: Scope of Benefits
FAQ 053 Will Long Acting 2nd generation injectables be covered as a pharmacy benefit when given in a clinic setting?
Published: September 4, 2020
Long Acting 2nd generation antipsychotics, when administered by a physician or other practitioner in a clinic setting and billed on an institutional or medical claim form will continue to be covered by the member’s managed care plan.
FAQ Spotlight: Managed Care Plans
FAQ 017 What health plans does the pharmacy carve-out apply to? Will the pharmacy benefit carve-out impact dual eligible members that have Medicaid Advantage and Medicaid? Does the pharmacy carveout apply to Managed Long-Term Care plans? Does the pharmacy carve-out apply to CHP?
Updated: October 9, 2020
The Fee-For-Service (FFS) Pharmacy Carve Out does not apply to Managed Long-Term Care plans (e.g., PACE, MAP, MLTC), the Essential Plan, or CHP.
The FFS Pharmacy Carve Out applies to all mainstream Managed Care Plans (MCPs), including HARP and HIV-SNP plans. More information can be found on slide 3 of the Transition (Carve-Out) of the Pharmacy Benefit from Managed Care to Fee-for-Service (FFS): Implementation Update & Strategy presentation.
FAQ Spotlight: General & 340B
FAQ 061 In the calculated amount $87.2M in State savings as a result of the pharmacy carve-out, did NYS DOH take into consideration an anticipated increase in Medicaid admissions and emergency room (ER) visits?
FAQ 067 Has NYS DOH conducted an analysis to measure the impact the pharmacy carve-out will have on agencies providing services to populations with HIV/AIDs? We are concerned that the pharmacy carve-out will result in rising HIV/AIDs infections and deaths?
- NYS DOH recognizes that 340B revenue associated with Medicaid Managed Care claims is used to provide support services to vulnerable populations and therefore, has committed to a multi-year reinvestment to 340B Covered Entities, which includes $102M in SFY 2021-22.
- Medicaid Managed Care Plans will continue to have the ability to coordinate activities necessary for their members’ care. NYS DOH recognizes the importance of these activities, which will be funded through the administrative portion of capitated managed care premiums. Furthermore, NYS DOH will provide the plans with access to data that is needed to coordinate care.
Resources
Resources
Website
Information regarding the transition of the pharmacy benefit from Managed Care to FFS will be posted at the above website.
Email: PPNO@health.ny.gov – Please write Carve-Out in the subject line
Questions?
Please enter your question within the chat feature of the WebEx Event meeting.
Follow Us