The Future of Long Term Care in NYS
Mark Kissinger, Director, Division of Long Term Care
Rebecca Corso, Deputy Director, Division of Long Term Care
Office of Health Insurance Programs
NYS Department of Health (NYSDOH)
- Slides also available in Portable Document Format (PDF, 734KB)
September 29, 2015
Today´s Goals
- Present ideas and options for the future of MLTC and FIDA
- Have an Active Discussion with stakeholders to obtain feedback
Long Term Care - What Have We Accomplished?
- New York has shifted from a primarily fee-for-service delivery system to a robust managed care system.
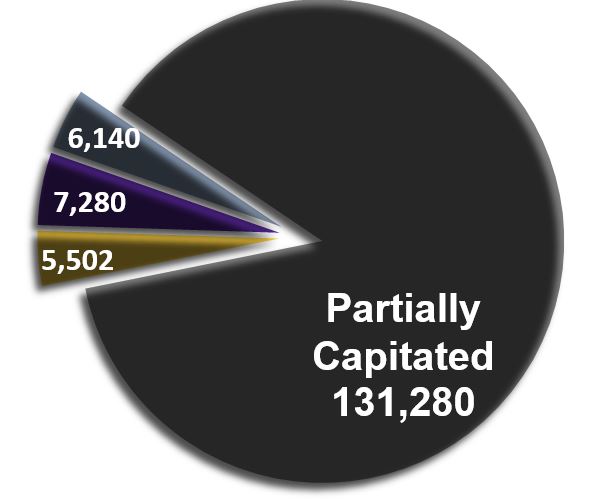
- Offer four MLTC options serving nearly 150,000 New Yorkers:
- Partial cap (available statewide)
- PACE (available in 16 counties)
- MAP (available in 12 counties)
- FIDA (available in 8 counties)
- Plan to build off of the successes of these models and look to the future of MLTC.
The Future of MLTC and FIDA
- Goal is to focus on integrating Medicaid and Medicare services to provide a delivery system that is better coordinated and that will help us to achieve the "Triple Aim," which includes:
- Lower health care costs
- Better health outcomes
- Better care experience
Proposed Initiative:
MLTC Plus
MLTC Plus
- MLTC "Plus" will build off of the partial cap MLTC product.
- The initiative is proposed to take a three-pronged approach

3 Elements of MLTC Plus
- Enhance MLTC benefit package
- Enhance the MLTC partial capitation benefit package, adding primary care and preventive health services.
- Add behavioral health services traditionally provided through the New York State Office of Mental Health´s Home and Community-Based Services (HCBS) Waiver program and Health and Recovery Plans (HARPs).
- These new services will bring added value to the MLTC population and is an extension of the MLTC program´s person-centered approach to care.
- Improve coordination
- Establish a mechanism to incentivize high-level, patient-centered care and increase the quality of care coordination services to plan enrollees.
- MLTC plans will determine the quality of an enrollee´s relationship with his/her primary care physician by establishing metrics.
- Reimbursement for successful performance will result in a bonus payment paid by the MLTC plan to physician.
- The bonus payment will be an amount reflective of the physician´s successful satisfaction of the MLTC plan´s quality metrics per active member per calendar year.
- Physician response to community-based nurse within two hours for urgent issues
- Physician response to community-based nurse within 24 hours for non-urgent issues
- Physician provides office or home visits a minimum of four times annually
- Physician returns signed orders within 7 business days
- Physician achieves satisfactory score on annual patient satisfaction survey on:
- Enrollee wait time
- Responsiveness to enrollee needs
- Clear communication of enrollee´s health issues, treatment options, etc.
- Physician provides timely and appropriate interventions, avoiding unnecessary hospitalizations
- Physician provides follow-up visits to enrollee within one week of hospital discharge
- Improve transitions
- Create specific requirements for care managers/transition specialists to achieve coordinated transitions.
- Care manager/transition coordinator will be required to:
- Communicate with a hospital discharge planner 48-72 hours prior to discharge.
- Review information related to the admission, including diagnosis, treatment, testing, imaging, additions/changes to medications, etc.
- Conduct outreach to a Certified Home Health Agency (CHHA) provider based on hospital discharge plans, if appropriate, based on the care plan
- Communicate with enrollees to discuss impending discharge and MLTC services available in the community
- Answer any questions, share telephone contact information and set up home visits within 48 hours of hospital discharge to review plans for follow up appointments or testing
- Conduct 2 follow-up telephone calls with the enrollee (or family, as appropriate) within 10 days of discharge to assure that the enrollee´s needs are being met
Additional Considerations for MLTC Plus
- MLTC Plus will strengthen the role of MLTC plans in promoting enrollee health and well- being by incentivizing quality outcomes and integrating behavioral health and other services into the MLTC partial capitation model.
- Through the implementation of the MLTC Plus initiative areas, successful local projects will be studied and scaled statewide as appropriate, across the MLTC partial capitation plan infrastructure. In this way, MLTC Plus will promote the "Triple Aim" and ensure delivery system reform.
- DLTC will select a number of MLTC partial capitation plans and providers for these purposes to help identify and develop the best ways for MLTC plans to support delivery system reform. In conjunction with DLTC, these partners will help implement and evaluate the DSRIP supportive activities.
QUESTIONS?
The Future of FIDA
The Future of FIDA
FIDA was designed to enhance what is offered under existing models by providing more services, along with a more intensive participant-centered care coordination model.
Approach will result in:
- Better coordination of care
- Better health outcomes
- Cost savings
NYS wants to take the opportunity to work with stakeholders on the design to determine what the future of the program will look like.
FIDA - Current Status
- Began voluntary enrollment in January 2015 and Passive Enrollment in April 2015 in New York City and Nassau County.
- Implementation in Region 2 (Suffolk and Westchester Counties) was halted, but will move forward on or around January 2016.
- CMS has offered demonstration states the option of requesting a two year extension.
- DOH has requested an extension through December 2019
- It is not binding and we can decide not to move forward with the extension
- Over 7,000 people are enrolled.
FIDA Enrollment
Participants, plans and providers report that the people enrolled in FIDA are:
- Satisfied with the program
- Being successfully served
FIDA has experienced lower than expected enrollments.
Potential participants do not want to change programs because:
- Fearful that they will lose their current providers;
- Unclear on how FIDA could benefit them above and beyond what they are getting in their current MLTC program;
- Satisfied with their MLTC Plan; and
- Cautious of making any change in their healthcare coverage.
Additional factors:
- Plans´ efforts toward marketing
- Providers were not educated early enough to support the program
- Medicare providers may be unwilling to work with managed care plans
- The IDT model is perceived to be onerous on providers
- Plans are not opening their networks to providers that are working with FIDA participants, especially Medicare providers
- Rate uncertainty
- Provider training requirements are onerous
We Are In This Together
- NYSDOH and CMS are committed to the growth and success of FIDA
- We need the support and commitment of Plans, Providers, Advocates and Consumers
How Can We Move Forward?
- Propose several changes to the program design and requirements that will provide:
- Incentives & Rewards
- Flexibility
FIDA IDT
- The IDT offers an opportunity for participants and their providers to work collaboratively in making decisions about participants´ care.
- This collaborative approach can lead to better outcomes for participants because the individual is more invested in the process.
- The IDT Policy was slightly modified on September 15, 2015 to provider greater flexibility to plans and providers.
FIDA IDT Proposal
- Modify the FIDA program to make the IDT optional for participants.
- Individuals who wish to participate in the FIDA program would be offered the option of having an IDT or a care manager to coordinate their care.
- Create incentives for utilization and participation in the IDT.
FIDA - IDT Participation Incentives
- To incentivize utilization of the IDT model over traditional care management, NYSDOH will develop a bonus pool in which FIDA plans will receive bonus payments for utilization of the IDT model.
- Bonus payments will be designed so that plans must achieve a minimum threshold of 25% utilization of the IDT model for participants with long term care needs.
- Anything below 25% will result in plans being fiscally penalized by receiving a reduction in future capitation payments.
- Plans will receive a bonus payment from a pool of funds for the percentage of their long term care membership that utilizes the IDT model above 25%.
- Above the 25%, plans can receive bonus payments that progressively increase based on percentage of IDT utilization.
- Create a provider incentive pool in which funding will be provided to plans who must pass the bonus payment to providers for participation in IDT meetings.
- The program could also allow for participants to receive a small incentive (such as a grocery gift card) each time he/she participates in an IDT meeting.
FIDA Marketing Proposals
- Consider the following changes in the marketing guidelines to provide flexibility:
- Allow Plans to provide a comparison between their MLTC programs.
- Eliminate the requirement that a licensed marketing representative be the only person that can describe the FIDA plan to potential consumers.
- Explore additional areas of flexibility within Medicare rules.
- NYSDOH would invest resources to develop a FIDA marketing campaign.
FIDA Enrollment Proposal
- Allow FIDA plans to enroll directly into their plan as allowed in Medicare Advantage.
- In certain cases, modify intelligent assignment to be specific to an individual and attempt to match individuals to a plan that most closely resembles their providers, with preference given to their primary care provider and home care provider.
- Incentivize plans to enroll individuals into integrated care by requiring companies participating in the FIDA Program to achieve 25% integrated care (FIDA, MAP or PACE) across all LTSS members by December 2016.
- Additional expansion measures:
- Implement semi-annual passive enrollment into FIDA.
- Offer individuals on Medicaid FIDA as their first choice upon enrollment into Medicare when they turn age 65 and are in need of long term care services.
- Expand enrollment to the dual population not in need of 120 days of LTSS (well duals) and include the rollout of a passive enrollment process for this population.
FIDA Service Package Proposal
- FIDA has a more robust service package than any other managed care plan, including State Plan HARP services, as well as the Nursing Home Transition and Diversion (NHTD) and the Traumatic Brain Injury (TBI) waiver services.
- We propose to also add the following services:
- Add the HARP HCBS services to the benefit package
- Require that all plans offer an "Over the Counter" card
- Evaluate services identified by stakeholders that should be added or eliminated
FIDA Network Proposal
- Many opt-outs have occurred because potential participants were afraid that their Medicare providers would not be in the network.
- NYSDOH proposes to add an "any willing primary care provider" requirement to the program whereby FIDA plans must allow any qualified primary care provider who is willing to accept the terms of the managed care plan to provide services to FIDA participants.
QUESTIONS?
Contact us:
MRT website
https://www.health.ny.gov/health_care/medicaid/redesign/
MLTC MRT 90 website
https://www.health.ny.gov/health_care/medicaid/redesign/mrt90/
FIDA MRT 101 website
https://www.health.ny.gov/health_care/medicaid/redesign/mrt_101.htm
Email:
FIDA@health.ny.gov
Follow Us