Managed Long Term Care (MLTC)
Clinical Advisory Group Meeting
- Presentation is also available in Portable Document Format (PDF)
Khalil Alshaer, Md Raina Josberger
Medical Director Deputy Director
Division of Long Term Care Division of Quality Measurement
Office of Health Insurance Programs Office of Quality and Patient Safety
Welcome and Introductions
Welcome and Introductions
- Welcome to the 8th Meeting of the MLTC Clinical Advisory Group (CAG)!
- Our last meeting was June 7, 2018 when we provided a status update on MLTC progress in VBP and solicited feedback on the strategies for partial plans in VBP Level 2 and for Skilled Nursing Facilities (SNFs).
- As always, we greatly appreciate your participation in the MLTC CAG and welcome any newcomers to the group!
Meeting Purpose and Agenda
Purpose: To provide the final MY 2019 measure set and to inform the CAG about the policy for Skilled Nursing Facilities (SNFs).
Agenda
- Welcome and Introductions
- Final MLTC VBP Measure for MY 2019
- Skilled Nursing Facilities (SNFs) in VBP
MLTC Discussions and Sub–Team meetings
Convened Sub–team meetings since August 2017 CAG meeting
| October 2017 – February 2018 | November 2017 | November – December 2017 | January 2018 | February 2018 | May 2018 | May 2018 | June 2018 | September 2018 |
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|
|
Attribution of Members to VBP Contractors
Key Distinctions for Level 2:
• Attribution is to the IPA or ACO
- Current attribution methodologies will remain in place for Level 1.
- For Level 2, the Office of Quality and Patient Safety (OQPS) will need to identify providers/VBP contractor combinations by requesting a Tax Identification Number (TIN) for an IPA/ACO group taking responsibility for a grouping of members together as a network.
- Attributions Files were due on August 1, 2018
2019 MLTC Partial Cap Measure Set
2019 MLTC VBP Quality Measure Set Changes
- Update – The MY 2019 Quality Measure Sets will be released in October 2018
- Specifically, the following updates have been confirmed:
- Addition of the Category 1 new falls measure
- Removal of the Category 1 No ER visit in the last 90 days measure
2019 MLTC Partial VBP Quality Measure Set – Category 1 Measures
| Measures | Measure Source/ Steward | Classification |
|---|---|---|
| Percentage of members who did not experience falls that resulted in major or minor injury in the last 90 days * | UAS – NY/New York State | P4P |
| Percentage of members who received an influenza vaccination in the last year* | UAS – NY/New York State | P4P |
| Percentage of members who remained stable or demonstrated improvement in pain intensity* | UAS – NY/New York State | P4P |
| Percentage of members who remained stable or demonstrated improvement in Nursing Facility Level of Care (NFLOC) score* | UAS – NY/New York State | P4P |
| Percentage of members who remained stable or demonstrated improvement in urinary continence* | UAS – NY/New York State | P4P |
| Percentage of members who remained stable or demonstrated improvement in shortness of breath* | UAS – NY/New York State | P4P |
| Percentage of members who did not experience uncontrolled pain* | UAS – NY/New York State | P4P |
| Percentage of members who were not lonely and not distressed* | UAS – NY/New York State | P4P |
| Potentially Avoidable Hospitalizations (PAH) for a primary diagnosis of heart failure, respiratory infection, electrolyte imbalance, sepsis, anemia, or urinary tract infection* | UAS – NY/New York State with linkage to SPARCS^ data | P4P |
| Potentially Avoidable Hospitalizations (PAH) for a primary diagnosis of heart failure, respiratory infection, electrolyte imbalance, sepsis, anemia, or urinary tract infectionǂ | MDS 3.0§/New York State with linkage to SPARCS Data | P4P |
* Included in the NYS DOH MLTC Quality Incentive measure set
+ UAS – NY denotesthe Uniform Assessment System for New York for MLTC members
^ SPARCS denotes the Statewide Planning and Research Cooperative System
ǂ Included in the NYS DOH Nursing Home Quality Initiative measure set
2019 MLTC Partial VBP Quality Measure Set – Category 2 Measures
| Measures | Measure Source/ Steward | Classification |
|---|---|---|
| Percent of long stay high risk residents with pressure ulcersǂ | MDS 3.0 + /CMS | P4P |
| Percent of long stay residents who received the pneumococcal vaccineǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents who received the seasonal influenza vaccineǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents experiencing one or more falls with major injuryǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents who lose too much weightǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents with a urinary tract infectionǂ | MDS 3.0/CMS | P4P |
| Care for Older Adults – Medication Review | NCQA§ | P4R |
| Use of High–Risk Medications in the Elderly | NCQA | P4R |
| Percent of long stay low risk residents who lose control of their bowel or bladderǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents whose need for help with daily activities has increasedǂ | MDS 3.0/CMS | P4P |
| Percentage of members who rated the quality of home health aide or personal care aide services within the last 6 months as good or excellent* | MLTC Survey/New York State | P4R |
| Percentage of members who responded that they were usually or always involved in making decisions about their plan of care* | MLTC Survey/New York State | P4R |
| Percentage of members who reported that within the last 6 months the home health aide or personal care aide services were always or usually on time* | MLTC Survey/New York State | P4R |
| Percent of long stay residents who have depressive symptomsǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents with dementia who received an antipsychotic medicationǂ | MDS 3.0/Pharmacy Quality Alliance | P4P |
| Percent of long stay residents who self– report moderate to severe painǂ | MDS 3.0/CMS | P4P |
§ NCQA denotes the National Committee for Quality Assurance
* Included in the NYS DOH MLTC Quality Incentive measure set
ǂIncluded in the NYS DOH Nursing Home Quality Initiative measure set
2019 MLTC Fully Capitated Plans Measure Set – MAP and FIDA
2019 MLTC MAP and FIDA – Primary and Preventative Care Measures
| Measures | Measure Source/ Steward | Measure Identifier | Classification |
|---|---|---|---|
| Comprehensive Diabetes Care: Eye Exam (Retinal) Performed* | NCQA/ HEDIS | NQF 0055 | P4R |
| Comprehensive Diabetes Care: Medical Attention for Nephropathy* | NCQA/ HEDIS | NQF 0062 | P4R |
| Colorectal Cancer Screening* | NCQA/ HEDIS | NQF 0034 | P4R |
| Antidepressant Medication Management – Effective Acute Phase Treatment & Effective Continuation Phase Treatment* | NCQA/ HEDIS | NQF 0105 | P4R |
| Follow–up After Hospitalization for Mental Illness^ | NCQA/ HEDIS | NQF 0576 | P4R |
| Initiation and Engagement of Alcohol and Other Drug Dependence Treatment* | NCQA/ HEDIS | NQF 0004 | P4R |
* Included in the IPC/TCGP measure set
^ Included in the Health and Recovery Plan (HARP) measure set
Acronyms: NCQA denotes the National Committee for Quality Assurance; HEDIS denotes the Healthcare Effectiveness Data and Information Set; NQF denotes National Quality Forum
2019 MLTC MAP, FIDA, and PACE – Category 1 Measures
| Measures | Measure Source/ Steward | Classification |
|---|---|---|
| Percentage of members who did not experience falls that resulted in major or minor injury in the last 90 days * | UAS – NY/ New York State | P4P |
| Percentage of members who received an influenza vaccination in the last year* | UAS – NY/ New York State | P4P |
| Percentage of members who remained stable or demonstrated improvement in pain intensity* | UAS – NY/ New York State | P4P |
| Percentage of members who remained stable or demonstrated improvement in Nursing Facility Level of Care (NFLOC) score* | UAS – NY/ New York State | P4P |
| Percentage of members who remained stable or demonstrated improvement in urinary continence* | UAS – NY/ New York State | P4P |
| Percentage of members who remained stable or demonstrated improvement in shortness of breath* | UAS – NY/ New York State | P4P |
| Percentage of members who did not experience uncontrolled pain* | UAS – NY/ New York State | P4P |
| Percentage of members who were not lonely and not distressed* | UAS – NY/ New York State | P4P |
| Potentially Avoidable Hospitalizations (PAH) for a primary diagnosis of heart failure, respiratory infection, electrolyte imbalance, sepsis, anemia, or urinary tract infection* | UAS – NY/ New York State with linkage to SPARCS data | P4P |
| Potentially Avoidable Hospitalizations (PAH) for a primary diagnosis of heart failure, respiratory infection, electrolyte imbalance, sepsis, anemia, or urinary tract infectionǂ | MDS 3.0/ New York State with linkage to SPARCS data | P4P |
* Included in the NYS DOH MLTC Quality Incentive measure set
ǂ Included in the NYS DOH Nursing Home Quality Initiative measure set
Acronyms: UAS – NY denotes the Uniform Assessment System for New York for MLTC members; SPARCS denotes the Statewide Planning and Research Cooperative System; MDS 3.0 denotes the Centers for Medicare and Medicaid Services Minimum Data Set for nursing home members
2019 MLTC MAP, FIDA, and PACE – Category 2 Measures
| Measures | Measure Source/ Steward | Classification |
|---|---|---|
| Percent of long stay high risk residents with pressure ulcersǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents who received the pneumococcal vaccineǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents who received the seasonal influenza vaccineǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents experiencing one or more falls with major injuryǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents who lose too much weightǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents with a urinary tract infectionǂ | MDS 3.0/CMS | P4P |
| Care for Older Adults – Medication Review | NCQA | P4R |
| Use of High–Risk Medications in the Elderly | NCQA | P4R |
| Percent of long stay low risk residents who lose control of their bowel or bladderǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents whose need for help with daily activities has increasedǂ | MDS 3.0/CMS | P4P |
| Percentage of members who rated the quality of home health aide or personal care aide services within the last 6 months as good or excellent* | MLTC Survey/New York State | P4R |
| Percentage of members who responded that they were usually or always involved in making decisions about their plan of care* | MLTC Survey/New York State | P4R |
| Percentage of members who reported that within the last 6 months the home health aide or personal care aide services were always or usually on time* | MLTC Survey/New York State | P4R |
| Percent of long stay residents who have depressive symptomsǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents with dementia who received an antipsychotic medicationǂ | MDS 3.0/Pharmacy Quality Alliance | P4P |
| Percent of long stay residents who self– report moderate to severe painǂ | MDS 3.0/CMS | P4P |
* Included in the NYS DOH MLTC Quality Incentive measure set
ǂ Included in the NYS DOH Nursing Home Quality Initiative measure set
Acronyms: UAS – NY denotes the Uniform Assessment System for New York for MLTC members; SPARCS denotes the Statewide Planning and Research Cooperative System; MDS 3.0 denotes the Centers for Medicare and Medicaid Services Minimum Data Set for nursing home members
2019 MLTC Fully Capitated Plans Measure Set – PACE
2019 PACE – Quality Measures Specific to PACE
| Measures | Measure Source/ Steward | Measure Identifier | Classification |
|---|---|---|---|
| Percentage of PACE Participants with an Advance Directive or Surrogate Decision Maker Documented in the Medical Record AND Percentage of PACE Participants with Annual Review of their Advance Directive or Surrogate Decision Maker Document | CMS | –– | P4R |
| Percent of Participants Not in Nursing Homes | CMS | –– | P4R |
| PACE Participant Emergency Department Use Without Hospitalization | CMS | –– | P4R |
* Included in the NYS DOH MLTC Quality Incentive measure set
ǂ Included in the NYS DOH Nursing Home Quality Initiative measure set
Acronyms: UAS – NY denotes the Uniform Assessment System for New York for MLTC members; SPARCS denotes the Statewide Planning and Research Cooperative System; MDS 3.0 denotes the Centers for Medicare and Medicaid Services Minimum Data Set for nursing home members
2019 MLTC MAP, FIDA, and PACE – Category 1 Measures
| Measures | Measure Source/ Steward | Classification |
|---|---|---|
| Percentage of members who did not experience falls that resulted in major or minor injury in the last 90 days * | UAS – NY/ New York State | P4P |
| Percentage of members who received an influenza vaccination in the last year* | UAS – NY/ New York State | P4P |
| Percentage of members who remained stable or demonstrated improvement in pain intensity* | UAS – NY/ New York State | P4P |
| Percentage of members who remained stable or demonstrated improvement in Nursing Facility Level of Care (NFLOC) score* | UAS – NY/ New York State | P4P |
| Percentage of members who remained stable or demonstrated improvement in urinary continence* | UAS – NY/ New York State | P4P |
| Percentage of members who remained stable or demonstrated improvement in shortness of breath* | UAS – NY/ New York State | P4P |
| Percentage of members who did not experience uncontrolled pain* | UAS – NY/ New York State | P4P |
| Percentage of members who were not lonely and not distressed* | UAS – NY/ New York State | P4P |
| Potentially Avoidable Hospitalizations (PAH) for a primary diagnosis of heart failure, respiratory infection, electrolyte imbalance, sepsis, anemia, or urinary tract infection* | UAS – NY/ New York State with linkage to SPARCS data | P4P |
| Potentially Avoidable Hospitalizations (PAH) for a primary diagnosis of heart failure, respiratory infection, electrolyte imbalance, sepsis, anemia, or urinary tract infectionǂ | MDS 3.0/ New York State with linkage to SPARCS data | P4P |
* Included in the NYS DOH MLTC Quality Incentive measure set
ǂ Included in the NYS DOH Nursing Home Quality Initiative measure set
Acronyms: UAS – NY denotes the Uniform Assessment System for New York for MLTC members; SPARCS denotes the Statewide Planning and Research Cooperative System; MDS 3.0 denotes the Centers for Medicare and Medicaid Services Minimum Data Set for nursing home members
2019 MLTC MAP, FIDA, and PACE – Category 2 Measures
| Measures | Measure Source/ Steward | Classification |
|---|---|---|
| Percent of long stay high risk residents with pressure ulcersǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents who received the pneumococcal vaccineǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents who received the seasonal influenza vaccineǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents experiencing one or more falls with major injuryǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents who lose too much weightǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents with a urinary tract infectionǂ | MDS 3.0/CMS | P4P |
| Care for Older Adults – Medication Review | NCQA | P4R |
| Use of High–Risk Medications in the Elderly | NCQA | P4R |
| Percent of long stay low risk residents who lose control of their bowel or bladderǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents whose need for help with daily activities has increasedǂ | MDS 3.0/CMS | P4P |
| Percentage of members who rated the quality of home health aide or personal care aide services within the last 6 months as good or excellent* | MLTC Survey/New York State | P4R |
| Percentage of members who responded that they were usually or always involved in making decisions about their plan of care* | MLTC Survey/New York State | P4R |
| Percentage of members who reported that within the last 6 months the home health aide or personal care aide services were always or usually on time* | MLTC Survey/New York State | P4R |
| Percent of long stay residents who have depressive symptomsǂ | MDS 3.0/CMS | P4P |
| Percent of long stay residents with dementia who received an antipsychotic medicationǂ | MDS 3.0/Pharmacy Quality Alliance | P4P |
| Percent of long stay residents who self– report moderate to severe painǂ | MDS 3.0/CMS | P4P |
* Included in the NYS DOH MLTC Quality Incentive measure set
ǂ Included in the NYS DOH Nursing Home Quality Initiative measure set
Acronyms: UAS – NY denotes the Uniform Assessment System for New York for MLTC members; SPARCS denotes the Statewide Planning and Research Cooperative System; MDS 3.0 denotes the Centers for Medicare and Medicaid Services Minimum Data Set for nursing home members
MLTC VBP Quality Measure Reporting for Full Cap Plans
- For all new measures specific to MAP, FIDA, and PACE that require Medicare data or follow CMS measure development for PACE
- Category 1 – P4R measures must be reported to the State on an annual basis
- For MAP and FIDA, plans will report measures for Plan/Provider–VBP Contractor attribution combinations
- For PACE, PACE organizations will report measures for the PACE
The instructions for reporting will be added to the 2019 Value Based Payment Reporting Requirements Technical Specifications Manual
- For all measures recommended for P4P use for VBP purposes for MAP, FIDA, and PACE (see slide 19)
- Category 1 VBP measures selected by MAP, FIDA, and PACE plans and Providers/VBP Contractors from the MLTC VBP Quality Measure set will be calculated by the State for Plan/Provider–VBP Contractor combinations submitted to the State in the plan–submitted attribution file.
- The Nursing Home PAH measure will be calculated annually at a facility level.
- All Category 2 MLTC VBP measures may be used at the discretion of the contractual parties.
- At least one measure must be used as a P4P measure.
VBP Skilled Nursing Facility (SNF) Model
SNF in VBP
Background
The limitation on the Managed Long Term Care (MLTC) Nursing Home benefit is for Partially Capitated plans only. It has been proposed to CMS; however, it will not be a limited benefit until it has CMS approval. Managed Long Term Care will cover residents residing in skilled nursing facilities, for at least 3 months after permanent placement designation and exhaustion of Medicare benefit. To accommodate this transition, the VBP model for SNF would be slightly modified to apply to short–stay residents with appropriate quality metrics.
Proposal
- The Nursing Home Potentially Avoidable Hospitalization (PAH) measure would be an optional measure between the MLTC plan and the SNF.
- Require MLTC plan and nursing facility to base their level 1 arrangements on at least the CMS "successfully discharged to the community" measure from the CMS short stay measure set.
- Allow other short stay measures to be included in the contract, at the discretion of the MLTC plan and SNF. This approach continues SNF participation in VBP where much progress has been achieved.
MLTC SNF in VBP
CMS has nine "short stay" measures at a facility level:
- Percentage of short–stay residents who report moderate to severe pain
- Percentage of short–stay residents who were successfully discharged to the community
- Percentage of short–stay residents who had an outpatient emergency department visit
- Percentage of short–stay residents who were re–hospitalized after a nursing home admission
- Percentage of short–stay residents who improved in their ability to move around on their own
- Percentage of short–stay residents with pressure ulcers that are new or worsened
- Percentage of short–stay residents who needed and got a flu shot for the current flu season
- Percentage of short–stay residents who needed and got a vaccine to prevent pneumonia
- Percentage of short–stay residents that got antipsychotic medication for the first time
Funding of Proposed Short–Stay Measure
- For weighing purposes, the Nursing Home PAH measure will be replaced with the short– stay measure "successfully discharged to the community".
- There are proposed plan savings for better performance on the CMS short–stay measure of successful discharge to the community.
- Successful movement of members from the Nursing Home to the community have the potential for inclusion in the community PAH measure.
Next Steps and Closing Remarks
- Key Milestones
- October 2018 – MY 2019 Measures Released
- October 2018 – MLTC Measure Reporting Guidance Released
- Questions and Comments
- As always, questions and comments may be directed to mltcvbp@health.ny.gov
- Many thanks for participating in the MLTC CAG!
Appendix
MLTC VBP Quality Measure Data Reporting Timeline
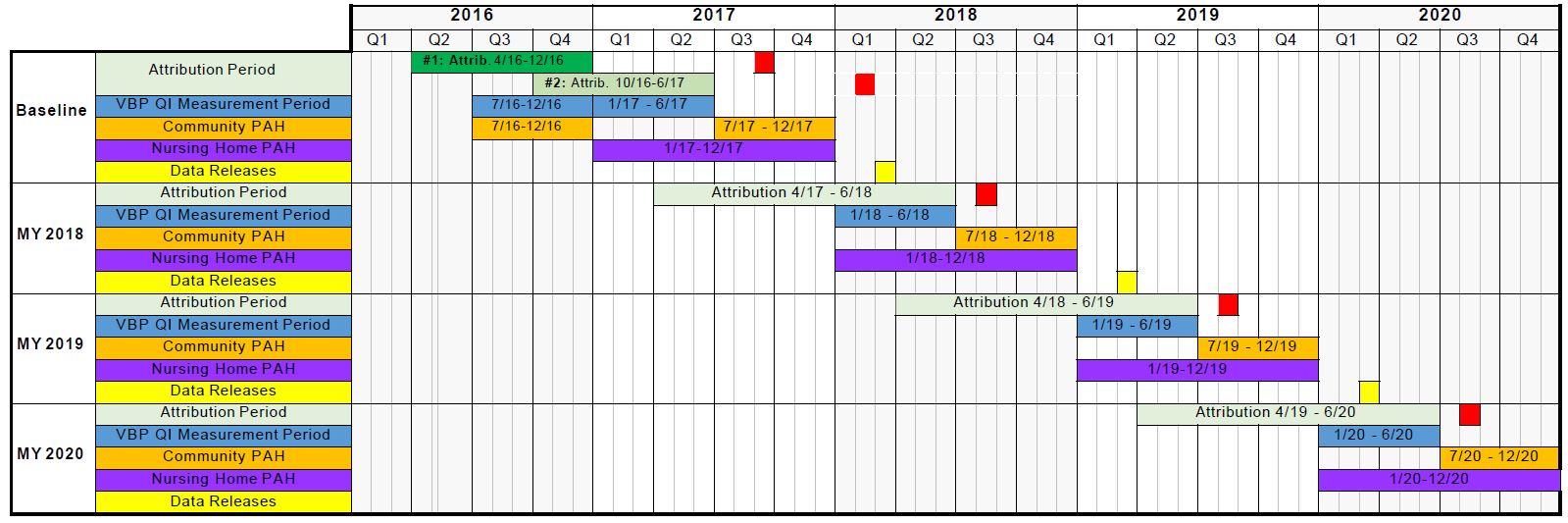
Legend
- Attribution file due to DOH
- Preliminary Community Potentially Avoidable Hospitalizations (PAH) data released
- Final VBP Quality Incentive (QI) and PAH data released
Follow Us