VBP Pilots Update
- Transcript
- Webinar also available in Portable Document Format (PDF)
March 8, 2018
Agenda
- Program Overview and Current State
- Recent Policy Updates
- DUA and HCS Account Updates
- Payment and Contract Reminders
- Social Determinants of Health
- Quality Measure Test Project
- Next Steps
VBP Pilot Program Overview
VBP Pilot Program is a two–year program intended to create momentum and support the transition to VBP, establishing best practices and sharing lessons learned. It is also intended to test new outcome measures, and where necessary improve design of VBP arrangements. The Pilots are required to:
- Adopt on–menu VBP arrangements, as per NYS VBP Roadmap guidelines
- Submit a VBP contract (or contract addendum) by April 1, 2017, with a retroactive effective contract date of no later than January 1, 2017 and through December, 2018 (2–year program)
- Report on all reportable Category 1 and a minimum of one (1) distinct Category 2 measures for each arrangement being contracted, or have a State and Plan approved alternative
- Move to Level 2 VBP arrangements in Year 2 of the Pilot Program
- Develop Webinars on lessons learned from the contracting process and participation in the program
Current State
| Type | Provider | Managed Care Organization | Level (Y1) | Status |
|---|---|---|---|---|
| HARP | Maimonides Medical Center | Healthfirst PHSP, Inc. | 1 | Approved |
| Mount Sinai Health Partners | Healthfirst PHSP, Inc. | 1 | Approved | |
| IPC | Community Health IPA | Affinity Health Plan, Inc. | 1 | Approved |
| TCGP | Greater Buffalo United ACO | Yourcare Health Plan, Inc. | 1 | Approved |
| Somos Your Health IPA | Affinity Health Plan, Inc. | 2 | Approved | |
| Somos Your Health IPA | HealthPlus HP, LLC | 2 | Approved | |
| Somos Your Health IPA | New York State Catholic Health Plan, Inc. | 2 | Approved | |
| Somos Your Health IPA | Healthfirst PHSP, Inc | 1 | Approved | |
| Somos Your Health IPA | United Healthcare of New York, Inc. | 2 | Pending | |
| Somos Your Health IPA | Wellcare of New York, Inc. | 2 | Approved | |
| St. Joseph´s Hospital Health Center | New York State Catholic Health Plan, Inc. | 1 | Approved | |
| St. Joseph´s Hospital Health Center | Molina Healthcare of New York, Inc. | 1 | Approved |
Recent Policy Updates
Recent Policy Updates
Quality Measure Reporting
Originally, the Pilots were to report on at least 2 distinct Category 2 measures. Through the Feasibility Taskforce it became clear that the Pilots would not be able to achieve the originally required measure reporting. Instead, participants will report only one Category 2 measure of their choice for year 2.
Category 1 Measures: VBP Pilots are required to report all Category 1 measure data that the DOH has defined as reportable for Year1. Pilot participants will also report Controlling High Blood Pressure (Category 1) as part of a Quality Measure Testing Project.
MAPP Portal Access
Early MAPP portal access and data analysis is expected to be available in July 2018.
The Pilot team will communicate notices regarding HCS account access to the Pilot participants depending upon DUA process.
|top of section| |top of page|DUA and HCS Account Updates
UPDATE: Date Exchange Application Agreement
- A DUA is required from all Pilot provider organizations and MCOs in order for the State to share Medicaid data with VBP Pilot participants
- MCOs should complete a DUA in order to access VBP Dashboards when they go live
- MCOs can still receive data from their Pilot providers so long as the partners have a BAA in place
HCS Account Setup
Creating a HCS account is the first step in gaining access to the Medicaid Analytics Performance Portal (MAPP), which houses the VBP Dashboards.
Pilot HCS Account Set Up
- While some organizations may already have DSRIP HCS accounts, new accounts or designations unique to their VBP entities must be created to permit access to the VBP Dashboards in MAPP
- Once the initial VBP Dashboard Access Form is approved for each VBP contracting entity, the organization will then be able to add their own users to the system
Payment and Contract Reminders
Pilot Adjustment Payouts
- New Target Budgets based on the 2015 claims data is scheduled for release in March 2018.
- Year 1 payments to the Pilot participants will begin to be paid in March 2018 over a 6–month period.
- Year 2 payments to the Pilot participants will be in the April 2018 rates and paid over a 6–month period.
- The Pilot team will conduct quarterly interviews with the Pilot organizations during Year 2 of the program to ensure continued implementation.
Contracting
- All Year 2 contracts must be sent to contract@health.ny.gov by March 31, 2018 with "VBP Pilot" in the subject line
- Please use on–menu checklist to complete Year 2 contracts. Checklist can be found here.
- Effective January 1, 2018, all Year 2/Level 2 contracts are required to include one social determinant of health intervention.
- As of March 31, 2018, a Level 2 contract cannot be reported by the MCO on the VBPTR Survey without the defined SDH components within the contract. Failure to produce the SDH components in a Level 2 contract could result in the possibility of additional penalty.
Quality Measure Test Project
Current State Snapshot– Overview
- A summary report of the relevant internal quality measurement activities, processes, and systems that impact, directly or indirectly, your organization´s ability to share clinical data and report the Controlling High Blood Pressure measure for your VBP arrangement at the VBP contractor level.
- Some questions may pertain more broadly to the way your organization collects clinical data or calculates quality measures, while others may be specific to the VBP Arrangement in which you participate. Special instructions have been provided for those questions where responses will need to be specified by VBP Arrangement.
- There are two different sets of questions for MCOs and VBP Contractors
Testing Parameters
- MCOs will calculate the denominator using the eligible population for the Controlling High Blood Pressure (CBP) measure
- NCQA has just released newly proposed recommendations to add an Administrative Specification to use the eligible population for the denominator and use administrative data for numerator
- Where possible, the Testing project will take into consideration the proposed HEDIS recommendations to help determine the measure specifications used for the project
- MCOs will share information for VBP–attributed members included in the eligible population with providers in their VBP contracts
- VBP Contractors and MCOs will then work together to identify the necessary clinical data elements for patient blood pressure readings and design a common reporting format to share this data to populate numerator compliance
How will this information be used?
- Document the current state for how MCOs and providers share member and clinical data for HEDIS measurement
- Help project stakeholders understand the various data, systems, and processes used for VBP quality measurement or HEDIS
- Identify the availability of clinical data that can be used for quality measurement
- Ensure project stakeholders understand the limitations and challenges in using these data and systems
- Share current state findings
- Draft a Current State Report for how MCOs and providers share data for quality measurement
- Engage QEs, third parties, and other stakeholders to better support a VBP use case for quality measurement or HEDIS
- Develop project recommendations and requirements
- Align project requirements to newly proposed HEDIS specifications, where possible
- Develop standards for data formats, transport methods, etc. so data is available and useable
- Identify policy levers that can be used to support ongoing quality measurement
Current State Snapshot– General Questions
- Description of your organization
- Description of your organization´s existing VBP activities to help the State align project activities, milestones, and reporting protocols to reduce unnecessary project burden
- Attribution method used for your organization
- Use of third parties to help with quality measurement and whether or not they will be potentially included as a partner for your project
Eligible Population and Denominator
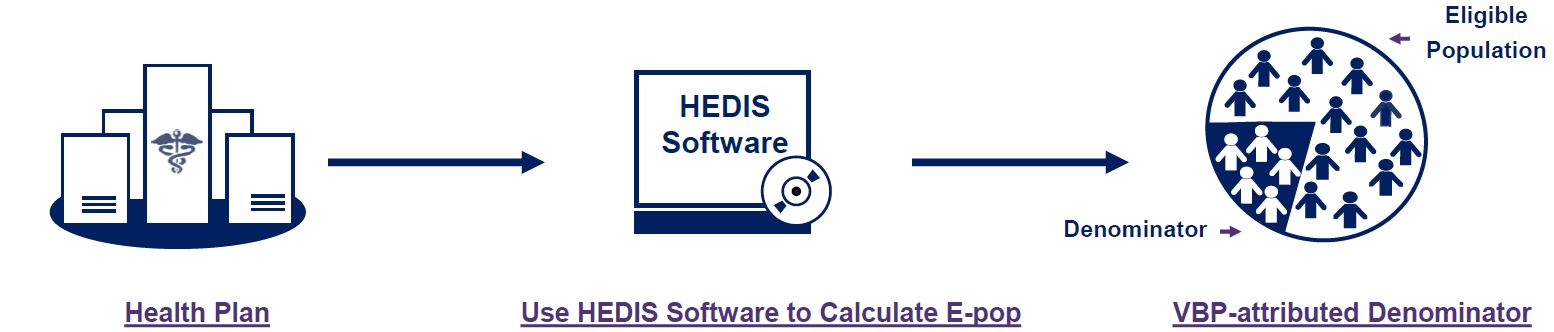
Health Plan
- Understand health plan ability to identify the eligible population without sampling using a new administrative method for Controlling High Blood Pressure
Use HEDIS Software to Calculate E–pop
- Age: 18–85 years of December 31
- Continuous Enrollment: Measure year (MY) with no more than one gap in continuous enrollment of up to 45 days
- Event/Dx: Two outpatient visits during first six months of MY or year prior w/ Dx of Hypertension (HTN)
- Exclusions: Members in hospice care, w/end–stage renal disease (ESRD), pregnant, or had nonacute inpatient admission during measure year
VBP–attributed Denominator
- Understand health plan ability to stratify eligible population to only include VBP–attributed members for the denominator
Sharing Member Data with VBP Contractors
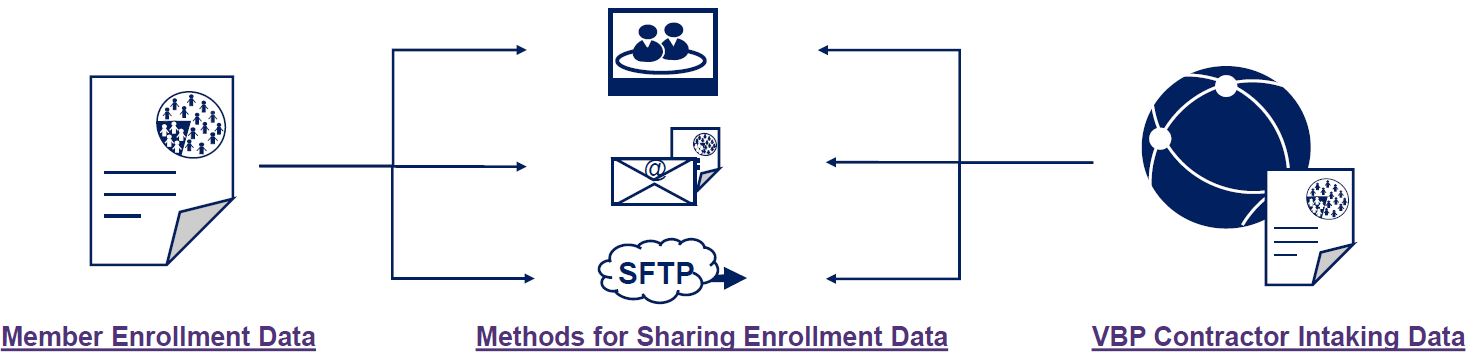
Member Enrollment Data
- Understand the manners in which health plans share member enrollment information with their VBP Contractors
Methods for Sharing Enrollment Data
How do they share data?
- MCO–owned provider portals
- Secure email
- SFTP sites
What data elements do they share?
- CIN, demographic, measures results for gap in care reports
What formats?
- Flat files, PDF, etc.
What frequency do they share data?
- Monthly, quarterly, etc.
VBP Contractor Intaking Data
- Understand VBP Contractor ability to intake member data
Aggregating, Extracting, and Sharing Clinical Data
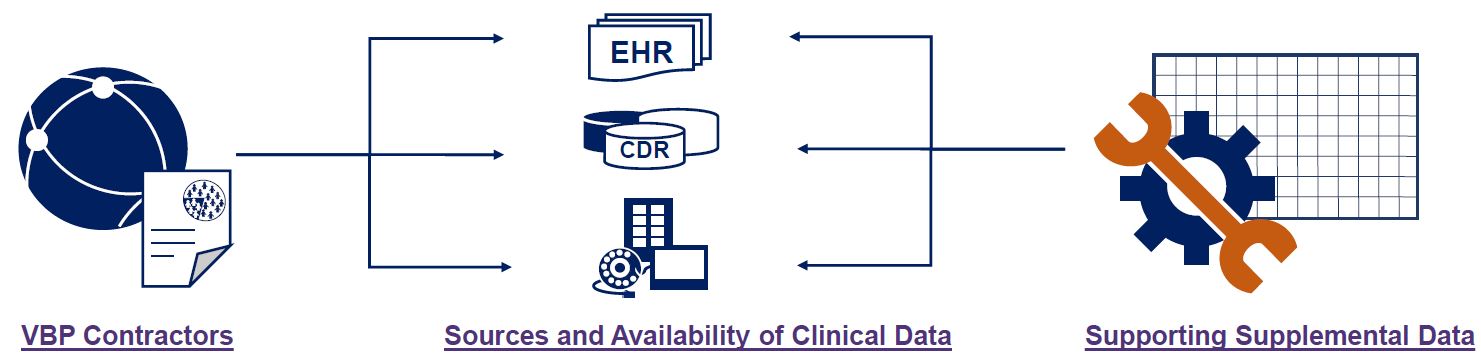
VBP Contractors
- Understand VBP Contractor ability to aggregate, extract, and configure clinical data to support measurement
Sources and Availability of Clinical Data
Sources of Clinical Data
- EHRs
- Clinical Data Repository (CDR)
- Third parties (e.g., QEs, data aggregators
Available Data
- Do these sources have data to use for measurement (e.g., BP values)?
Aggregating Data
- Can this data be aggregated?
Extracting Data
- Into what format is data extracted?
Supporting Supplemental Data
- Understand VBP Contractor ability to extract relevant clinical data and transform the data to support HEDIS measurement
Supplemental Data Feeds
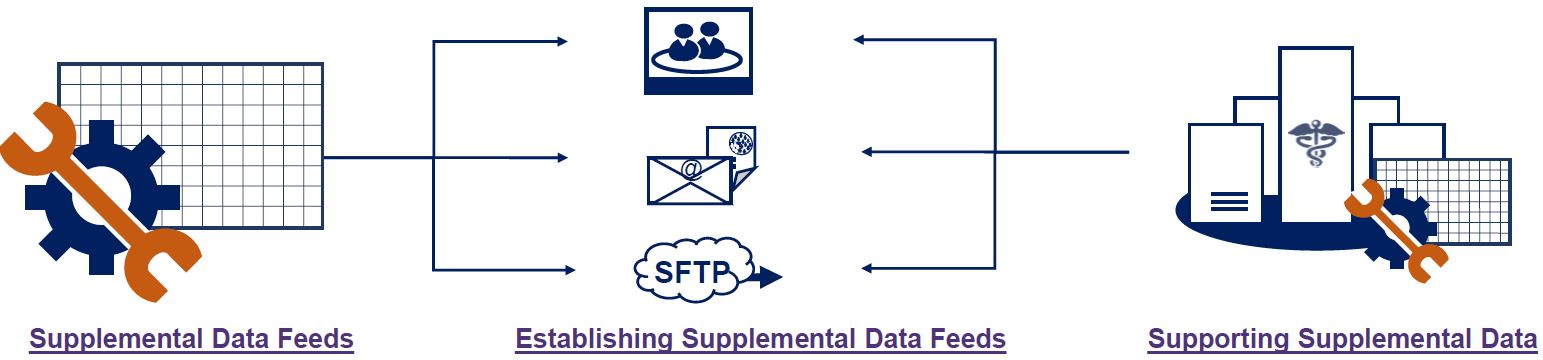
Supplemental Data Feeds
- Understand how clinical data from VBP Contractors needs to be configured for supplemental data for HEDIS
Establishing Supplemental Data Feeds
Intaking Supplemental Data
- MCO–owned provider portals
- Secure email
- SFTP sites
Data Format
- What formats are used for supplemental data (e.g., flat file)?
Data Elements
- What are the data elements that can be shared?
Frequency
- How often is this data taken in?
Supporting Supplemental Data
- Understand how MCOs can use these supplemental data feeds within their existing systems to support HEDIS
Supplemental Data Feeds
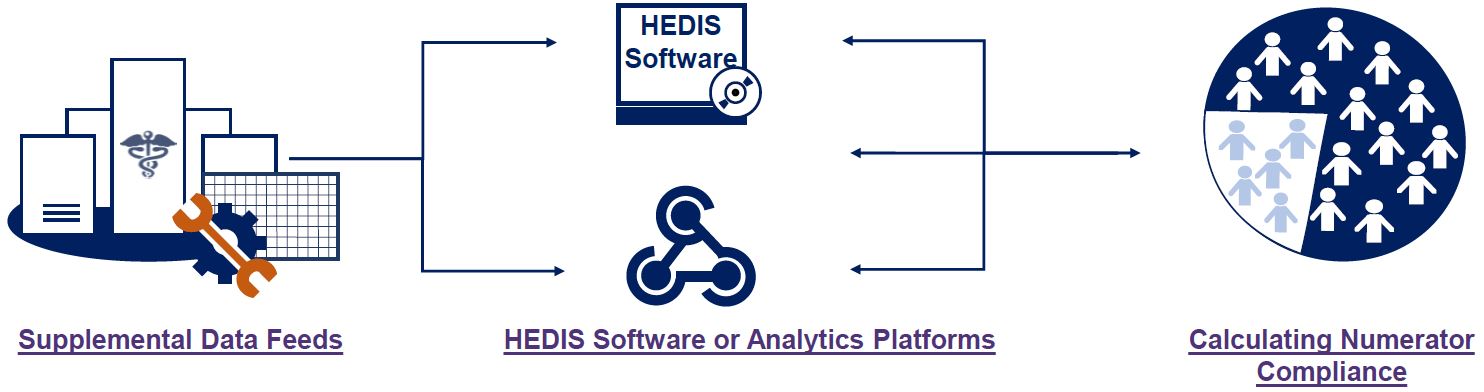
Supplemental Data Feeds
- Understand how clinical data from VBP Contractors needs to be configured for supplemental data for HEDIS
Establishing Supplemental Data Feeds
Intaking Supplemental Data
- MCO–owned provider portals
- Secure email
- SFTP sites
Data Format
- What formats are used for supplemental data (e.g., flat file)?
Data Elements
- What are the data elements that can be shared?
Frequency
- How often is this data taken in?
Supporting Supplemental Data
- Understand how MCOs can use these supplemental data feeds within their existing systems to support HEDIS
Supplemental Data Feeds
Supplemental Data Feeds
- Understand how health plans will intake this data to calculate numerator compliance
HEDIS Software or Analytics Platforms
Systems to intake supplemental data to calculate the measure
- Can MCOs use their HEDIS Software, analytics platform, or third party to help calculate measure results?
Calculating Numerator Compliance
- Understand how MCOs can use these systems to calculate numerator compliance
Next Steps
Systems to intake supplemental data to calculate the measure
- Can MCOs use their HEDIS Software, analytics platform, or third party to help calculate measure results?
Calculating Numerator Compliance
- Understand how MCOs can use these systems to calculate numerator compliance
Next Steps
| March | April | May | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Activities | Responsibility | W1 | W2 | W3 | W4 | W5 | W1 | W2 | W3 | W4 | W1 | W2 | W3 | W4 | W5 | |
|
|
3/9 | ||||||||||||||
|
|
4/6 | ||||||||||||||
|
|
4/13 | ||||||||||||||
|
|
5/4 | ||||||||||||||
|
|
|||||||||||||||
Next Steps
Next Steps
- The Pilot team will conduct quarterly interviews with the Pilot organizations during Year 2 of the program to ensure continued implementation.
- The Pilot Team will be reaching out to schedule Lessons Learned Webinars
- The Pilot Team will be reaching out to determine progress towards Tier One CBO contracts
- Quality Measure Test Project
- Work with Testing Participants to develop a project plan
- Work with Testing Participants to develop Current State Snapshot of the various activities supporting VBP quality measurement
- Formal Kickoff with all Testing Participants in late March to share relevant findings and provide additional project requirements
Failure to comply with the VBP Pilot Program requirements may result in recoupment of funds made available to VBP Pilot participants
Additional Reference Materials
VBP Support Materials
VBP Resource Library – Final CAG Reports:
- Path: DSRIP Homepage → Value Based Payment Reform → VBP Resource Library – Final CAG Reports
- Link: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_library/vbp_final_cag_reports.htm
VBP Resource Library:
- Path: DSRIP Homepage → Value Based Payment Reform → VBP Resource Library
- Link: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_library
Follow Us