Managed Long Term Care (MLTC) & Value Based Payment (VBP)
Discussion of Level 2
Stakeholders Meeting
- Presentation is also available in Portable Document Format (PDF)
February 20, 2018
Agenda
- Review of VBP Roadmap Arrangement for MLTC
- Discussion of Key Features of VBP
- Guiding Principles for the Discussion
- Discussion of Options for Level 2
- Implementation Considerations Discussion
- Next Steps
Review of VBP Roadmap Arrangement for MLTC
MLTC is a Designated Total Cost of Care Subpopulation Arrangement in the VBP Roadmap
| Integrated Physical & Behavioral Primary Care Includes social services interventions and community–based prevention activities |
|
| Maternity Care (including first month of baby) | Episodic |
| Chronic Bundle (Asthma, Diabetes, Depression and Anxiety, Substance Use Disorder, Trauma and Stressors...) |
Continuous |
| HIV/AIDS | |
| Managed Long Term Care (MLTC) | |
| Severe Behavioral Health/Substance Use Disorders (HARP Population) |
|
| Intellectually/Developmentally Disabled Population |
MLTC
Specialized Continuous Care – For these members, including MLTC, personalized goal setting and intensive care coordination become more dominant than disease management. In both examples of care, a focus on maximizing a member´s capability for self-management and personal autonomy in the most integrated settings (e.g. home and community) appropriate to a person´s needs, is central.
MLTC VBP Vision: Total Cost of Care
Goal: Improve population health through enhancing the quality of care for specific subpopulations that often require highly specific, intensive care.
- New York State Department of Health (DOH) has identified three subpopulations with their own distinct, dedicated managed care arrangements:
- MLTC;
- HIV/AIDS;
- HARP.
- A fourth subpopulation, to include specialty services provided by the Office for Persons with Developmental Disabilities – I/DD – is under development as these services are not included in managed care.
arrangements VBP Contractors
take responsibility for all care
needed by the Medicaid member.
– – – – – – – – – – – – – – – – – – – – –
Total Population
− TCGP
_____________________
Subpopulations
Acronyms: HARP = Health and Recovery Plans; TCGP = Total Care for the General Population; I/DD = Intellectual/Developmental Disabilities
|top of section| |top of page|Discussion of Key Features of VBP
Level 1 VBP Definition for Partially Capitated MLTC Plans
In anticipation, the State aims to treat potentially avoidable hospital use as ´quality outcomes´ for this subpopulation, improving the quality of life for these members, and rewarding MLTC providers when certain levels of reduced avoidable hospital use are reached. Such arrangements could be treated as Level 1 VBP arrangements, and would be eligible for financial incentives. Improved quality and reduced overall costs can also be realized by delaying or avoiding nursing home admissions through targeted interventions amongst the MLTC population residing at home."
New York State Department of Health, A Path toward Value Based Payment: New York State Roadmap for Medicaid Payment Reform, Annual Update June 2016: Year 2 (CMS–Approved April 2017), p. 18.
VBP Levels for Plans and VBP Contractors
Managed care plans can choose different levels of VBP with their VBP Contractors. Level 1 as a pay-for- performance contract is available only to partially capitated MLTC plans.
| VBP Levels 1, 2, and 2 in the NYS VBP Roadmap | |||
|---|---|---|---|
| MLTC Partial Level 1 | Level 1 VBP | Level 2 VBP | Level 3 VBP |
| Bonus for quality scores | Upside–only shared savings when quality scores are sufficient | Risk sharing (upside available when quality scores are sufficient) | Prospective capitation PMPM (with quality–based component) |
| Payment not tied to budget | FFS Retrospective Reconciliation | FFS Retrospective Reconciliation | Prospective total budget payments |
| Limited bonus payment or withhold | ↑ Upside Only | ↑ Upside & ↓ Downside Risk |
↑ Upside & ↓ Downside Risk |
- VBP Levels for Medicaid Advantage Plus (MAP), Fully Integrated Duals Advantage (FIDA), and Programs of All-Inclusive Care for the Elderly (PACE) comport to the selections available to Mainstream managed care
- At Level 2 VBP Contractors take on downside risk
Quality and Shared Savings for Mainstream Levels 1 & 2
| Quality Targets % Met | Level 1 VBP Upside only | Level 2 VBP Up– and downside when actual costs < budgeted costs | Level 2 VBP Up– and downside when actual costs > budgeted costs 25 |
|---|---|---|---|
| > 50% of Quality Targets Met | 50% of savings returned to VBP contractors | Up to 90% of savings returned to VBP contractors * | VBP contractors are responsible for up to 50% of losses |
| <50 % of Quality Targets Met | Between 10 – 50% of savings returned to VBP contractors (sliding scale in proportion with % of Quality Targets met) | Between 10 – 90% of savings returned to VBP contractors (sliding scale in proportion with % of Quality Targets met) | VBP contractors responsible for 50–90 % of losses (sliding scale in proportion with % of Quality Targets met) |
| Quality Worsens | No savings returned to VBP contractors | No savings returned to VBP contractors | VBP contractors responsible for up to 90% of losses * |
* Key Concept: Providers that deliver high quality care at the lower cost will grow more rapidly; ones that do not will shrink
Source: Roadmap June 2016: Year 2 CMS approved version. pg. 19
State – Plan – VBP Contractor Relationships
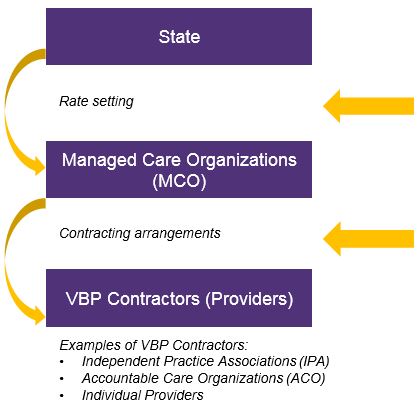 |
|
Types of VBP Contracting Entities – VBP Contractors
- Independent Practice Associations (IPAs)
- Accountable Care Organizations (ACOs)
- Individual Providers
- Hospital Systems
- Federally Qualified Health Centers (FQHC) and large medical groups
- Smaller providers
- Individual provider could either assume all responsibility and upside/downside risk or make arrangements with other providers; or
- Managed Care Organizations (MCOs) may want to create a VBP arrangement through individual contracts with these providers
MLTC VBP Level Targets & Penalties for Partial Plans
2018
If by 4/1/2018 less than 10% dollars of total MLTC plan expenditures are Level 1 or higher, a penalty of 0.5% on the marginal difference between 10% target for Level 1 and the total actual expenditures in Level 1 will be assessed
Penalty determined based on one quarter of spending for 2018
2019
If by 4/1/2019 less than 50% of total MLTC plan expenditures are in Level 1 or higher, a penalty of 1.0% on the marginal difference between 50% target for Level 1 and the total actual expenditure on Level 1 will be assessed
If by 4/1/2019 less than 5% of total MLTC plan expenditures are in Level 2 or higher, a penalty of 1.0% on the marginal difference between 5% target for Level 2 and the total actual expenditure on Level 2 will be assessed
Penalty determined based on annual spending for 2019 & 2020
2020
Level 1 target is 80%
Level 2 target is 15%
Guiding Principles for the Discussion
Principles to Guide the Discussion
- Level 2 must include some "downside" risk for providers/VBP Contractors
- 20% shared losses is the minimum for Level 2 per the VBP Roadmap
- The VBP Roadmap compliant arrangement definition for MLTC is a Total Cost of Care Subpopulation Arrangement. The intention is to incentivize care coordination across provider "silos"
- Single provider P4P contracts will not meet the definition
- Skilled Nursing Facilities (SNFs) will be included in the MLTC VBP (whether the Fiscal Year 2018–19 Executive Budget proposal passes or not) so efforts to integrate those services in total care arrangements continues to be a priority
- Lack of Medicare data/alignment is noted as a limiting factor
- MLTC Clinical Advisory Group (CAG) discussion focused on the creation of a lower risk "learning curve" option to allow for an interim step between P4P in Level 1 for partially capitated MLTC plans and Level 2 described in the VBP Roadmap for mainstream managed care plans
Discussion of Options for Level 2
Options Discussion
Option 1: PAH Included, Mainstream Level 2 Option
Option 1.a.: PAH Included, VBP Roadmap, Less Upside/Downside
Option 2: PAH Designated P4P, with Minimal Upside/Downside
Key for Considering the Options:
- The VBP Roadmap allows flexibility for Plans and VBP Contractors to negotiate shared savings and risk according to their own preferences. Hence, the "up to..." language in the Level descriptions.
- Continued use of the PAH measure as a separate P4P measure in Level 2 is a variable in creating the Level 2 definition. PAH may be "included" on the list of measures for Plan–to–VBP Contractor use. Or PAH may be separated and retained as a P4P measure.
- Risk levels vary in proportion to reward levels – the greater the upside, the greater the downside. One party to the contract should not bear significantly more risk in the relationship than the other.
- These options highlight some of the key variables – other combinations are possible.
Option 1: PAH Included, Mainstream Level 2 Option
Use of the PAH – Contracting parties could select PAH from the list of measures or not*
| Quality Targets % Met | Level 2 VBP Up– and Downside Actual Costs < Budgeted Costs | Level 2 VBP Up– and Downside Actual Costs > Budgeted Costs |
|---|---|---|
| Quality Improves >50% of Quality Targets Met |
Up to 90% of shared savings returned to VBP Contractor | VBP Contractors are responsible for up to 50% of losses |
| Quality Worsens | No savings returned to VBP Contractor | VBP Contractors responsible for up to 90% of losses |
*NYS will continue to pay VBP quality incentives based on PAH from NYS to MLTC plan
Example of Option 1: 90% Shared Savings/Losses
Scenario
- MLTC Plan & VBP Contractor agree to a 1,000–member arrangement based on 7 quality measures including the Community PAH
- The target budget for the attributed group of members is set at $47,000 for the 12–month contract
| Quality Targets % Met | Level 2 VBP Up– and Downside Actual Costs < Budgeted Costs | Level 2 VBP Up– and Downside Actual Costs > Budgeted Costs |
|---|---|---|
| Quality Improves >50% of Quality Targets Met • 4 of 7 Selected Measure Targets Met |
Actual Costs = $45,000 per member ($2,000 below $47,000 target budget) VBP Contractor would receive $1.8 million in shared savings (90% × $2,000 × 1,000–members) |
Actual Costs = $49,000 per member ($2,000 above $47,000 target budget) VBP Contractor would receive $1 million less (50% × −$2,000 × 1,000–members) |
| Quality Worsens | No shared savings for VBP Contractor | VBP Contractor would receive $1.8 million less (90% × −2,000 × 1,000 members) |
Option 1 – Pros and Cons
- Pros
- Fully aligns partially capitated MLTC with Mainstream managed care
- Provides substantial upside and opportunity for growth
- Ties losses to scale of the arrangement (budget) to align incentives to improve cost effectiveness
- Does not mandate the use of the PAH measure, allowing for flexibility in measure selection (NYS will continue to include the PAH in the VBP QI)
- Cons
- Allows providers to take on substantial risk
- Provides little opportunity to transition from MLTC Level 1 P4P environment
Option 1.a.: PAH Included, VBP Roadmap, Less Upside/Downside
Use of the PAH – Contracting parties could select PAH from the list of measures or not*
| Quality Targets % Met | Level 2 VBP Up– and Downside Actual Costs < Budgeted Costs | Level 2 VBP Up– and Downside Actual Costs > Budgeted Costs |
|---|---|---|
| Permissible Option in the Roadmap | ||
| >50% of Quality Targets Met | Up to 50% of shared savings returned to VBP Contractor | VBP Contractors are responsible for up to 20% of losses (minimum level to meet Level 2 definition) |
| Reduced Upside |
||
| Quality Worsens | No savings returned to VBP Contractor | VBP Contractors responsible for up to 50% of losses |
| Reduced Downside |
||
*NYS will continue to pay VBP quality incentives based on PAH from NYS to MLTC plan
Example of Option 1.a.: 50% Shared Savings/Losses
Scenario
- MLTC Plan & VBP Contractor agree to a 1,000 member arrangement based on 7 quality measures including the Community PAH
- The target budget for the attributed group of members is set at $47,000 for the 12–month contract
| Quality Targets % Met | Level 2 VBP Up– and Downside Actual Costs < Budgeted Costs | Level 2 VBP Up– and Downside Actual Costs > Budgeted Costs |
|---|---|---|
| Quality Improves >50% of Quality Targets Met • 4 of 7 Selected Measure Targets Met |
Actual Costs = $45,000 per member VBP Contractor would receive $1.0 million in shared savings (50% × $2,000 × 1,000 members) |
Actual Costs = $49,000 per member VBP Contractor would receive $400,000 less (20% × −$2,000 × 1,000 members) |
| Quality Worsens | No shared savings for VBP Contractor | VBP Contractor would receive $1.0 million less (50% × −2,000 × 1,000 members) |
Option 1.a – Pros and Cons
- Pros
- Risk is more limited – provides a step up for plans transitioning from P4P Level 1
- Permissible in the current the VBP Roadmap for partially capitated MLTC
- Ties losses to scale of the arrangement (budget) to align incentives to improve cost effectiveness
- Does not mandate the use of the PAH measure, allowing for flexibility in measure selection (NYS will continue to include PAH in the VBP QI)
- Cons
- More limited opportunity for growth
Option 2: PAH Designated P4P, with Minimal Upside/Downside
Use of the PAH – Contracting parties mandated to use PAH as a P4P Measures & Select Others*
| Quality Targets % Met | Level 2 VBP Up– and Downside Actual Costs < Budgeted Costs | Level 2 VBP Up– and Downside Actual Costs > Budgeted Costs |
|---|---|---|
| >50% of Quality Targets Met PAH Target Met |
Up to 20% of shared savings returned to VBP Contractor + PAH bonus payment | VBP Contractors responsible for PAH Penalty/Subtraction only |
| Reduced Upside |
||
| Quality Worsens PAH Target Not Met |
No savings returned to VBP Contractor No PAH bonus payment |
VBP Contractors responsible for up to 20% of losses (minimum to meet level 2 definition) + PAH Penalty/Subtraction |
| Reduced Downside |
*NYS will continue to pay VBP quality incentives based on PAH from NYS to MLTC plan
Example of Option 2: 20% Shared Savings/Losses + PAH P4P
Scenario
- MLTC Plan & amp; VBP Contractor agree to a 1,000 member arrangement based on 7 quality measures including the Community PAH
- The target budget for the attributed group of members is set at $47,000 for the 12 –month contract
- A $200 per member performance payment is conditioned on meeting PAH targets
| Quality Targets % Met | Level 2 VBP Up– and Downside Actual Costs < Budgeted Costs | Level 2 VBP Up– and Downside Actual Costs > Budgeted Costs |
|---|---|---|
| Quality Improves >50% of Quality Targets Met • 4 of 7 Selected Quality Measure Met & PAH Target Met |
Actual Costs = $45,000 per member VBP Contractor would receive $400,000 in shared savings + $200,000 bonus = total upside of $600,000 (20% × $2,000 × 1,000 members) + ($200 × 1,000 members) |
Actual Costs = $49,000 per member VBP Contractor would receive $200,000 less (PAH penalty) (−$200 × 1,000 members) |
| Quality Worsens | No shared savings for VBP Contractor | VBP Contractor would receive $400,000 less + a PAH penalty of $200,000 = total downside of $600,000 ((50% × −2,000 × 1,000 members) – ($200 per member) |
Option 2 – Pros and Cons
- Pros
- More limited downside risk for providers
- Two, separate potential opportunities for upside
- Against budget AND against PAH target
- VBP Contractors could negotiate to receive PAH bonuses even in the event that the other quality measure targets are not met
- Continues heightened emphasis on PAH measure to help prepare for care coordination that integrates Medicare
- Cons
- Minimal upside/opportunities to reinvest
- More complex measure methodology to include PAH as a separate measure
Implementation Considerations Discussion
Key Implementation Considerations
- Integrated care – constituting a Total Cost of Care Subpopulation Arrangement
- Shifting from P4P bonus payments to shared savings/losses budgeting – contracting options & target budgets
- Attribution of members to VBP Contractors
- Addressing size and scale considerations in moving to risk
- Social Determinants of Health (SDH) interventions in an MLTC context
Constituting a Total Cost of Care Subpopulation Arrangement
Goals of a Total Cost of Care Subpopulation Arrangement: Integration of care, care coordination across a continuum of services, and the most effective deployment of care resources (e.g., elimination of duplicative services, least restrictive/community–based care, etc.) and delivery of care centered on the individual, organized around the individual's needs and preferences.
- The State is committed to integration/alignment with Medicare and continued dialogue with CMS
- In the meantime, the VBP arrangement for partially capitated MLTC plans is total long –term care with the PAH measure as a P4P measure proxy for Medicare costs
- Efforts to "cross " provider silos and form provider networks are an important Level 2 feature and help prepare for a fully integrated/Medicare aligned approach
- Licensed Home Case Services Agencies (LHCSAs), Community Home Health Agencies (CHHAs), and SNFs comprise 80 –85% of total partially capitated MLTC plan spending and can form the basis for a total cost of care arrangement
Discussion of Provider Network Combinations
List of Services Covered in Partial Capitation MLTC Plans
Adult Day Health; Audiology/Hearing Aids; Care Management; Consumer Directed Personal Assistance Services; Dental Services; Home Care (nursing, home health aide, occupational, physical, and speech therapies); Home Delivered Meals and/or Meals Delivered in a Group Setting; Durable Medical Equipment; Medical Social Services; Non –Emergency Transportation to Receive Medical Services; Nursing Home Care; Nutrition; Vision Care; Personal Emergency Response System; Podiatry (Foot Care); Private Duty Nursing; Prostheses/Orthotics; Rehabilitation Therapies Outpatient; Respiratory Therapy; Social Day Care; Social/Environmental Supports (e.g., home modification)
- Home care agencies or nursing home groups are likely to partner with other service providers
- Small providers such as transportation, meal providers, and respiratory therapists can remain in the "downstream " for services rendered and do no have to take VBP arrangements on themselves
One Contracting Option for Total Cost of Care: An IPA or ACO Takes Responsibility for a Network
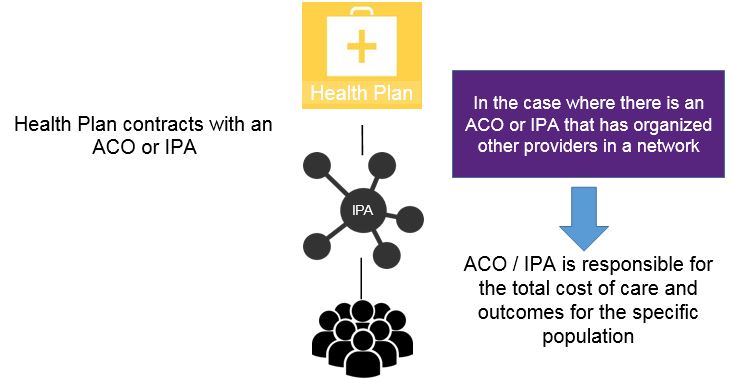
Note: ´ACO ´ refers to a NYS Medicaid ACO as defined under PHL § 2999–p
An Alternative Contracting Option to Provide for Total Cost of Care: MLTC Plan Creates the Budget
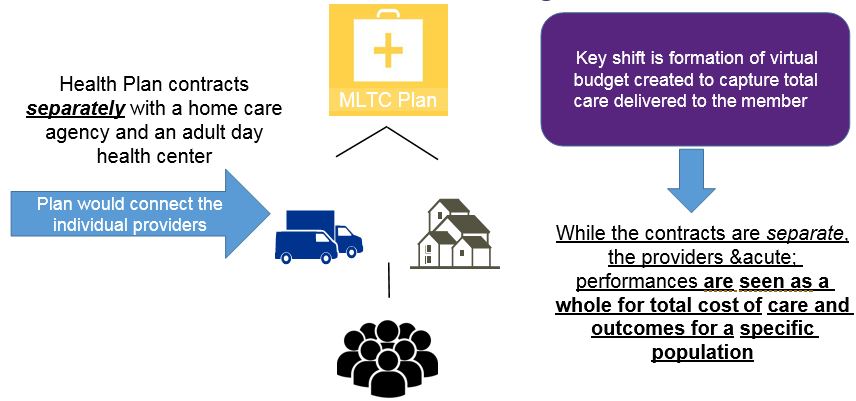
In practice, this option is often a temporary step during IPA / ACO formation.
Transitioning from P4P to Target Budgets – Key Concepts
- Historical claims data forms the basis for budget setting for the members/providers attributed to the VBP arrangement
- At Level 2 retrospective reconciliation is performed for same group of attributed members
- Transparency of data provides a level playing field
- Data sharing relationship should be explicitly described in VBP contract
- Methodology should be described in contracts
- Between MLTC plan and IPA/ACO
- And between each individual participating provider for MLTC plan –provider contracts and for IPA/ACO –provider contracts
- Methodology described in the VBP Roadmap is a guideline, not a requirement
- Contracting parties can determine appropriate method for their particular circumstances as long as the minimum definition are met
State Monitoring of Data Sharing
- The State will make available to providers: (1) the State to MCO rate schedules, and (2) stimulus and adjustment information
- The information provided by the State is not a requirement for contracting purposes
- For Level 2 and 3 arrangements, the State will monitor the data and information that is exchanged between MCOs and Lead VBP Contractors for the purpose of negotiating their target budgets and distribution of shared savings/loss
- Under development by the Division of Health Plan Contracting and Oversight (DHPCO) and DLTC
- The Survey is intended to capture the current status of data sharing
- Attribution is to the IPA or ACO
- A member can only be attributed to one VBP arrangement because the total cost of care budget is calculated at the member level
- Current attribution methodologies will remain in place for Level 1
- For Level 2, the Office of Quality and Patient Safety (OQPS) will need to identify providers/VBP contractor combinations by National Provider Identifier (NPI) or another unique identifier for an IPA/ACO group taking responsibility for a grouping of members together as a network
- DOH is investigating how to facilitate quality data collection for the variety of contracting parties/networks
- The size of the attributed population matters – larger samples provide a better understanding of cost trends and population behaviors
- Risk for smaller numbers of attributed members should be more limited
- The requirement can be fulfilled as plans submit Level 2 contracts
- A social determinants template and the contract with at least 1 Tier 1 CBO is required to be submitted
- Contracts with Tier 1 CBOs may be for "services rendered " and do not need to carry risk
- Many MLTC plans and providers are already providing SDH interventions
- These activities may include providing home modifications, nutrition, home delivered meals, facilitating community –based activities/integration, and any other home and community based services/supports
- Please submit any comments within the next two weeks, by Friday, March 2
- Comments may be submitted to mltcvbp@health.ny.gov
- The State ´s goal is to post Level 2 guidance to the VBP Resource Library by April 1
Data Sharing Survey
Attribution of Members to VBP Contractors
Key Distinctions for Level 2:
Scale Considerations for Risk Levels in VBP
Key:
To meet Roadmap targets, the key is to pursue Level 2 arrangements with VBP Contractors more capable of bearing downside risk. Risk can be more limited for smaller scale arrangements.
Remember: Only 5% of Expenditures are Required to Move to Level 2 by 2019
Level 2 and 3 Arrangements Require a Social Determinants of Health Intervention
Questions on SDH Interventions can be directed to: SDH@health.ny.gov
For more information, please visit the VBP Resource Library:
https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_library/index.htm
Next Steps
Next Steps
Appendix
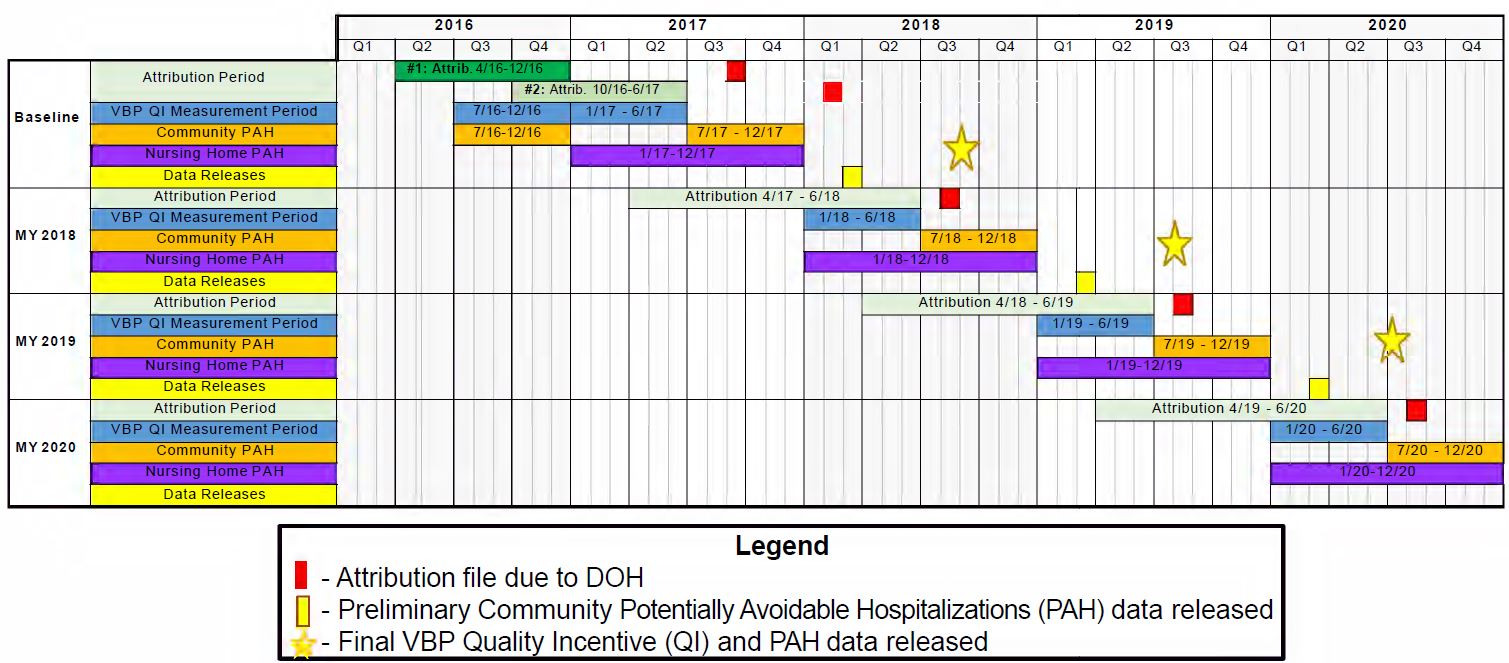
MLTC VBP Quality Measure Data Reporting Timeline
Thank you!
Please send questions and feedback to:
mltcvbp@health.ny.gov
Follow Us