Maternity Care Value Based Payment Arrangement
Measurement Year 2017 Fact Sheet
- Fact Sheet also available in Portable Document Format (PDF)
July 2017 NYS Medicaid Value Based Payment
Maternity Care Value Based Payment Arrangement
This fact sheet has been prepared to assist payers and providers to more thoroughly understand New York State's Medicaid Maternity Care Value Based Payment (VBP) Arrangement. It provides an overview of the Arrangement including a summary of the components of care, the underlying episodes of care, and the categories of measures recommended for use in Maternity Care Arrangements.
Introduction
The Maternity Care Arrangement is designed to allow the spectrum of maternity care providers to focus on prenatal and postpartum care for a mother and her baby. Quality measures related to each of these stages of care help reinforce the care connections built into the Arrangement and provide a standardized set of measures for maternity care providers statewide. Measures for the Arrangement include, for example, rates of postpartum complications, cesarean sections (C–sections), pre–term births and low–birth weight newborns. Providers who focus on health education, increased uptake of prenatal care, pre– and inter– conception counseling, appropriate C–section rates and resource utilization, screening for postpartum depression, evidence–informed home visits, and other evidence–based interventions have the opportunity to further improve maternity care and newborn outcomes, while realizing shared savings.
A key advantage of the Arrangement is that it puts maternity providers in the lead by creating a dedicated, all–inclusive budget for pregnancy, delivery, early postpartum, and newborn care. Providers can drive quality improvements by providing organized, integrated, and cost–effective care across the continuum from mother to baby. Another advantage of the Maternity Care Arrangement is that it provides an impetus to streamline the continuum of maternity care, which can be overlooked in larger scale, population–based healthcare initiatives. Finally, the attention and linkage to early outcomes for the newborn will help improve the well–being of the next generation of New Yorkers and curb future Medicaid costs.
This fact sheet provides an overview of New York State (NYS) Medicaid´s Maternity Care VBP Arrangement and is organized in two sections and an appendix:
- Section 1 describes the types of care included in the Maternity Care Arrangement and the method used to construct the episodes of care.
- Section 2 describes the quality measure selection process and the categories of measures recommended for use in Maternity Care Arrangements; and,
- The appendix contains a glossary of terms used in this document.
Section 1: Defining the Maternity Care Arrangement Episodes of Care
The Maternity Care Arrangement: Three Distinct Components of Care
The Maternity Care Arrangement creates a comprehensive, integrated view of maternity care, from "womb to crib", through three distinct components of care. Each component of the Arrangement consists of episodes of care, or groups of clinically related services provided by physicians, midwives and ancillary providers delivering care to the mother and newborn across all settings during a defined period.
As illustrated in Figure 1, the Maternity Care Arrangement consists of the following 3 components and underlying episodes:
- The Prenatal Care Component consists of a single episode (the Pregnancy Episode).
- The Delivery and Postpartum Care Component consists of a single episode (either the Vaginal or C–Section Delivery Episode).
- The Newborn Care Component consists of a single episode (the Newborn Episode).
Together, the three components of care reflect the prenatal care and services delivered up to 270 days prior to delivery (the Pregnancy Episode), the care provided to the mother from inpatient admission for delivery through 60 days after discharge (the Delivery Episode), and the care provided to the newborn from birth to 30 days after discharge (the Newborn Episode). (See Figure 1)
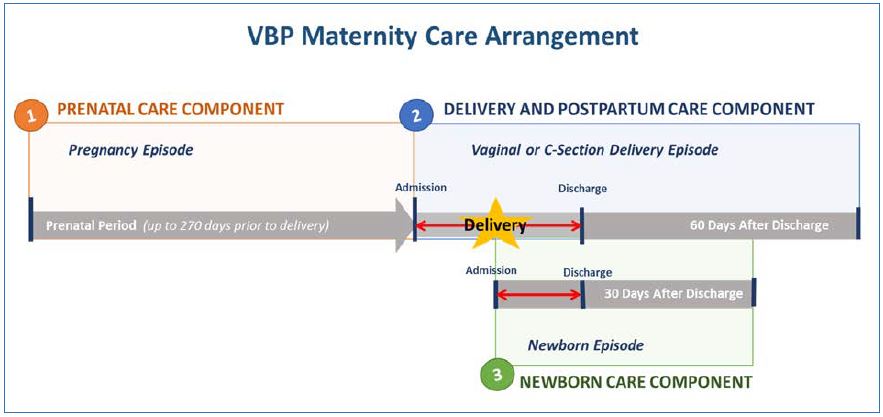
Figure 1: The Maternity Care Arrangement represents three components of maternity care including 1) prenatal care, 2) delivery and postpartum care, and 3) newborn care.
Constructing the Maternity Care Arrangement Episodes: Trigger Events, Time Windows, and Services
The episodes of care included in the Maternity Care Arrangement are constructed using a set of rules, based on the PROMETHEUS Analytics system (the grouper). The grouper governs what "triggers" or signals the existence of an episode and includes the logic describing when the episode begins and ends (the time window), and the services to be grouped to form the complete episode.
The Maternity Care Arrangement is driven by the delivery event, which triggers the process of identifying, linking, and constructing the episodes within the three components of care. The components of the Arrangement provide a view of the events which occurred prior to delivery, along with outcomes of the delivery and subsequent care. The procedure codes for delivery (Vaginal or C–section Delivery) are considered "trigger codes" for the episodes of care, initiating a review of claims from the components of maternity care to construct the episodes based on clinically relevant services.
The section below summarizes the logic for the episodes of care within the three components of the Maternity Care Arrangement, including the trigger events, time windows, and included service parameters for each episode. A more detailed review of the episode construction rules, definitions, and code sets are available on the Altarum Institute´s website.1
It is important to note that the time frame for the completion of the episodes of care within the Arrangement may span across contract years. The delivery episode completion date will determine the year for which the three components of care will be counted. Episodes may include services delivered in the year prior or subsequent to the contract year, consistent with the defined look back or look forward time periods as outlined in the figures below. Further, in order for a delivery and the associated components of care to be included in the Arrangement, each episode must be completed as described below.
The Underlying Episodes of the Maternity Care Arrangement
Prenatal Care Component
The Prenatal Care Component of the Maternity Care Arrangement includes one episode, called the Pregnancy Episode, which specifically targets prenatal care services.
Pregnancy Episode
- The Pregnancy Episode is triggered by the delivery (procedure codes for vaginal or C–section delivery), which serves as an indication that a pregnancy has occurred for the delivering mother.
- The Pregnancy Episode time window includes a look back window of 270 days prior to the admission for the delivery in order to capture all prenatal care services delivered from the beginning of the pregnancy to the admission for delivery.
- The Pregnancy Episode includes all prenatal care services such as office visits, laboratory tests, ultrasound examinations, and medications, as well as any pregnancy–related hospital admissions and complications up to delivery.
- The Pregnancy Episode will be considered complete with the delivery, which is considered the terminating or final event to close the Episode.
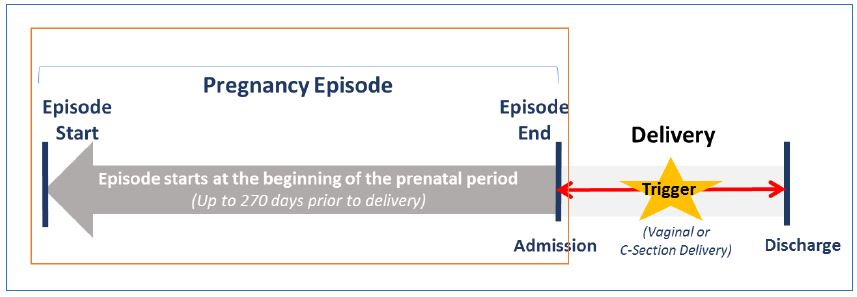
Figure 2: Pregnancy Episode example: The Pregnancy Episode spans the course of prenatal care from 270 days prior to delivery.
Delivery and Postpartum Care Component
The Delivery and Postpartum Care Component of the Maternity Care Arrangement, known as the Delivery Episode (either Vaginal or C–section Delivery), specifically targets services provided to the mother during the inpatient admission for delivery and the postpartum maternal care provided up to 60 days after discharge.
Delivery Episode (Vaginal or C–Section Delivery)
- The Delivery Episode (Vaginal or C–Section Delivery) is triggered by the procedure codes indicating either a Vaginal or C–section delivery.
- The time window for the Delivery Episode begins at admission for the delivery and extends to 60 days after discharge of the mother. The Episode includes all relevant services provided to the mother during this time window, including services provided during the inpatient stay for the delivery, as well as for postpartum care.
- The Delivery Episode (Vaginal or C–Section Delivery) is considered complete at the close of the time window, 60 days after discharge of the mother from the hospital.
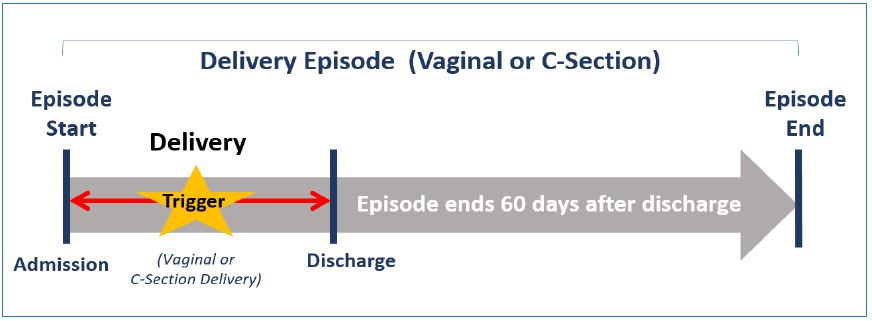
Figure 3: Delivery Episode example: The Delivery Episode (Vaginal or C–Section) includes services provided to the mother over the course of the inpatient admission for delivery through 60 days post–discharge for the mother.
Newborn Care Component
The Newborn Care Component of the Maternity Care Arrangement includes one episode, called the Newborn Episode, that specifically targets services provided to the newborn from birth, including the inpatient nursery and/or NICU stay, as well as care provided up to 30 days after discharge.
Newborn Episode
- The Newborn Episode is triggered by newborn diagnosis codes indicating a baby has been born either by vaginal delivery or C–Section.
- The Episode begins with the first service provided for the newborn as indicated by the initial Medicaid claim. The episode time window extends from this initial service to 30 days after discharge from the hospital for the newborn. All services provided to the newborn during the episode time window, including services during the inpatient stay, inclusive of any neonatal intensive care unit services, laboratory and diagnostic tests, and professional services (e.g. neonatologist, Primary Care Physician), are included in the Newborn Episode.
- The episode is considered complete at the close of the time window, 30 days after discharge.
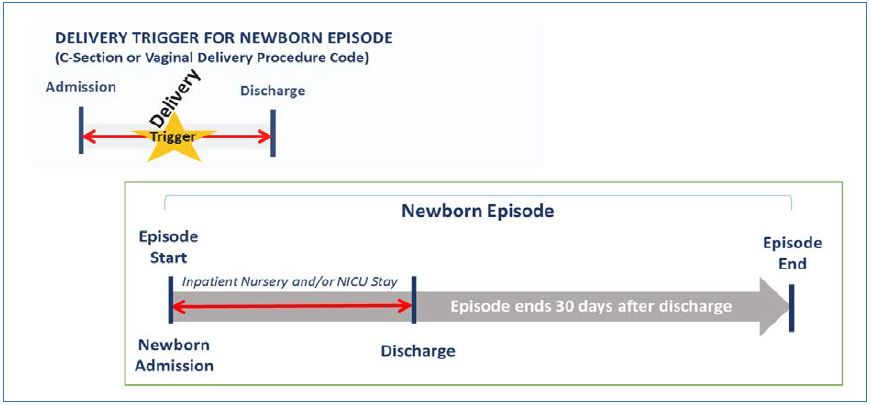
Figure 4: Newborn Episode example: The Newborn Episode is triggered by the delivery and includes all services provided to the newborn over the course of the initial inpatient stay and during the 30–day post–discharge period.
Member and Episode Eligibility
While the delivery is the triggering event for the Maternity Care Arrangement, not all deliveries occurring during the contract year will be included. Deliveries included in the Arrangement must meet the following requirements.
- Covered Deliveries: All deliveries covered by Medicaid Managed Care, as well as the associated prenatal, postpartum, and newborn care, are eligible for inclusion in the Maternity Care Arrangement with the following exceptions:
- Age: Medicaid mothers younger than 12 or older than 64 at the time of the delivery are excluded;
- Maternal Death: Deliveries resulting in the death of the mother are excluded, along with the associated prenatal care and care for the surviving newborn;
- Stillborn and Multiple Live Births: Deliveries resulting in stillborn or multiple live births are excluded from the Maternity Care Arrangement;
- Medicaid members for whom Medicaid is not the sole payer: Medicaid members with claims or encounters for which Medicaid is not the sole payer are excluded (e.g. dually eligible populations and members with Medicaid as payer of last resort on commercial premium); and,
- Members eligible for inclusion under a VBP Subpopulation Arrangement: Members eligible for inclusion under the HIV/AIDS, Health and Recovery Plan (HARP), Managed Long Term Care (MLTC), or Intellectually/Developmentally Disabled (I/DD) VBP Subpopulation Arrangements are excluded.
- Deliveries associated with three complete episodes: Deliveries must be associated with a complete Pregnancy (unless no prenatal care occurred),2 Delivery (Vaginal or C–section Delivery), and Newborn Episode to be included in the Maternity Care Arrangement. For example, a delivery and the care components will not be included in the Arrangement until completion of the 60–day, maternal post–discharge period associated with the Delivery Episode time window, even if both the Pregnancy and the Newborn Episodes are complete.
Member Attribution
State guidance for attribution recommends that the episodes within the Maternity Care Arrangement be attributed to the obstetrician or midwife who provides the plurality of the prenatal care.3 Provision of the majority of prenatal care services is determined by identification of the obstetrician or midwife associated with the greatest number of Evaluation and Management (E&M) visits for prenatal care prior to delivery. In the case of a tie (2 providers having the same number of qualifying E&M visits), the delivery and the 3 associated components of the Maternity Care Arrangement will be attributed to the provider associated with the higher cost of care.
In cases where there is no obstetrician or midwife identified as the billing provider for prenatal care services, the delivery and three associated components of care are attributed to the provider performing the delivery procedure.
VBP Contractors and the Medicaid Managed Care Organizations (MCOs) can adopt standards for attribution in their contracts not in alignment with the guidance above, so long as the contract receives State approval for meeting VBP contracting requirements.
Calculation of Episode Costs
Once the Maternity Care Arrangement episodes of care have been constructed, the costs (defined as the total amount paid by the Medicaid MCO for services) associated with each of the episodes will be combined to produce a total cost of care for the Maternity Care Arrangement. The aggregate costs can be further analyzed to identify and understand variation across the underlying episodes and by service type, leading to opportunities for improvement in quality of care and resource use.
Stop–Loss and High–Cost Components of the Maternity Care Arrangement
Certain factors, such as a neonatal intensive care unit (NICU) admission for a newborn, can easily skew the cost of the Newborn Care Component of the Arrangement, exposing providers to excessive risk. To help mitigate this risk, VBP Contractors in the Maternity Care Arrangement can consider adding stop–loss provisions to their contracts to exclude episodes of care with a total cost above a certain threshold.
Section 2: VBP Quality Measure Set for the Maternity Care Arrangement
The 2017 Maternity Care Quality Measure Set was created in collaboration with the Maternity Clinical Advisory Group (CAG). Measures recommended by the CAG were submitted to DOH for further feasibility review and, ultimately, to the VBP Workgroup, the group responsible for overall VBP design and final approval for New York State Medicaid. During the final review process, the Maternity Care quality measure set was aligned with existing measures in the Delivery System Reform Incentive Payment (DSRIP) Program, the State´s Vital Statistics maternity care measures, Quality Assurance Reporting Requirements (QARR) measures, and measures utilized by Medicare and Commercial programs in NYS, where appropriate. The measures were further categorized as Category 1, 2, or 3 based on reliability, validity, and feasibility, and by suggested use as either Pay–for–Reporting (P4R) or Pay–for–Performance (P4P).
The Maternity Care Quality Measure Set is intended to encourage providers to meet high standards of patient–centered, clinical care and coordination across multiple settings through pregnancy, delivery and postpartum periods, and newborn care from birth to the first 30 days post–discharge.
Measure Classification
In June 2016, the Maternity CAG published recommendations to the State on quality measures and support required for providers to be successful in improving the financial sustainability of New York State´s safety net. Additionally, the report addressed other implementation details related to a VBP Maternity Care Arrangement. Upon receiving the CAG recommendations, the State conducted additional feasibility review and analysis to define a final list of measures for inclusion during the VBP Measurement Year (MY) 2017. Each measure has been designated by the State as Category 1, 2, or 3 according to the following criteria:
- CATEGORY 1 – Approved quality measures that are felt to be both clinically relevant, reliable and valid, and feasible;
- CATEGORY 2 – Measures that are clinically relevant, valid, and probably reliable, but where the feasibility could be problematic. These measures will be further investigated during the VBP Pilot program; and,
- CATEGORY 3 – Measures that are insufficiently relevant, valid, reliable and/or feasible.
Note that measure classification is a State recommendation. Although Category 1 Measures are required to be reported, plans and VBP Contractors can choose the measures they want to link to payment, and how they want to pay on them (P4P or P4R) in their specific contracts.
Category 1
Category 1 quality measures, as identified by the Maternity CAG and accepted by the State, are to be reported by VBP Contractors. These measures are also intended to be used to determine the amount of shared savings for which VBP contractors would be eligible.4
The State classified each Category 1 measure as either P4P or P4R:
- P4P measures are intended to be used in the determination of shared savings amounts for which VBP Contractors are eligible.5 Measures can be included in both the determination of the target budget and in the calculation of shared savings for VBP Contractors; and,
- P4R measures are intended to be used by Medicaid MCOs to incentivize VBP Contractors for reporting data to monitor quality of care delivered to members under the VBP contract. Incentives for reporting will be based on timeliness, accuracy, and completeness of data. Measures can be reclassified from P4R to P4P through annual CAG and State review or as determined by the Medicaid MCO and VBP Contractor.
Categories 2 and 3
Category 2 measures have been accepted by the State based on agreement of measure importance, validity, and reliability, but flagged as presenting concerns regarding implementation feasibility. Some of these measures will be further investigated in the VBP pilots. The State requires that VBP Pilots select and report a minimum of two distinct, Category 2 measures per VBP Arrangement (or have a State and Plan approved alternative). VBP Pilot participants will be expected to share meaningful feedback on the feasibility of Category 2 measures when the CAGs reconvene during the Annual Review Cycle.
Measures designated as Category 3 were identified as unfeasible at this time or as presenting additional concerns including validity or reliability when applied to the attributed member population for the Maternity Care Arrangement. Several measures in the original CAG report were removed for small sample size at a VBP contractor level, or have already demonstrated high performance at a statewide level, and therefore are no longer in the Category 1 or 2 measure list. These Category 3 measures will not be tested in pilots or included in VBP Arrangements in 2017.
Annual Review
Measure sets and classifications are considered dynamic and will be reviewed annually. Updates will include additions, deletions, reclassification of measure category, and reclassification from P4R to P4P or P4P to P4R based on experience with measure implementation in the prior year. During 2017, the CAGs and the VBP Workgroup will reevaluate measures and provide recommendations for MY 2018. A full list of the 2017 Maternity Care measures is included in the NYS VBP Resource Library on the Department of Health (DOH) web site.6
Measures will be updated for 2018 per the annual measure review process. The measures and State– determined classifications provided in the "VBP Quality Measures" section of the Library are recommendations for MY 2017.
Appendix:
VBP Glossary
VBP Glossary
- Diagnosis codes: These are codes (as defined in the PROMETHEUS grouper) based on the International Classification of Diseases (ICD) that are used to group and categorize diseases, disorders, symptoms, etc. These codes help identify clinically related services to be included in the episode in conjunction with the relevant procedure codes. These codes may include trigger codes, signs and symptoms and other related conditions and are used to steer services into an open episode.
- Episode of Care: An Episode of Care includes groups of clinically related services (as defined in the PROMETHEUS grouper) delivered by physicians and ancillary providers across all settings of care during a defined period.
- Exclusions: Some episodes have specific exclusion criteria, which are either exclusions from analysis and contracting based on clinical reasons or exclusions from eligibility for Medicaid.
- Grouper: PROMETHEUS Analytics system. The rules for each episode are programmed into an analytic tool that runs on claims data in a systematic fashion. The analytic program – the grouper – governs what starts or "triggers" an episode, the length of time an episode will run, and the kinds of services that are grouped together to form the episode.
- Included Service: A service that is pulled into an episode by the PROMETHEUS Analytics system grouper is considered an included service.
- Look Back & Look Forward: From the point in which an episode is triggered, episode costs / volume are evaluated within the associated time window for a predetermined number of days before and after the trigger date. Costs, volume, and other episode components that fall within this range are captured within the episode.
- Procedure codes: These are codes used to identify clinically–related services to be included in the episode in conjunction with the typical diagnosis codes. Procedure codes include International Classification of Diseases (ICD) procedures, Healthcare Common Procedure Coding System (HCPCS) and Current Procedural Terminology (CPT) codes.
- Time window: This is the time that an episode is open for analytic purposes. It may include the trigger event, a look back period and a look forward period and could extend based on rules and criteria.
- Trigger code: A trigger code assigns a time window for the start and end dates of each episode (depending on the episode Type). Trigger codes can be ICD diagnosis or procedure codes, CPT codes, or HCPCS codes, and could be present on an inpatient facility claim, an outpatient facility claim, or a professional claim.
- VBP Contractor: An entity – either a provider or groups of providers – engaged in a VBP contract.
_____________________________________
1. Details on Episode of Care definitions and PROMETHEUS Analytics, including information on associated diagnostic and procedure codes, are available on the Altarum Institute´s website (Link) 1
2. Member receipt of prenatal care services is not a requirement for the construction and completion of a Pregnancy Episode. In the case of a delivery occurring for a mother who received no prenatal care, the delivery indicates that the pregnancy condition exists, triggering construction of the Pregnancy Episode. If no claims for prenatal care services are returned during the Pregnancy Episode time window, then the Episode will be closed as complete with a total cost for the Pregnancy Episode of $0. 2
3. Provider specialty is based on the provider´s specialty as registered in the National Plan & Provider Enumeration System (NPPES). 3
4. New York State Department of Health, Medicaid Redesign Team, A Path toward Value Based Payment: Annual Update, June 2016: Year 2, New York State Roadmap for Medicaid Payment Reform, June 2016, p. 34. (Link). 4
5. Ibid. 5
6. NYS Delivery System Reform Incentive Payment (DSRIP) – VBP Resource Library (Link) 6
Follow Us