Value Based Payment (VBP) Account Implementation: March Webinar
- Webinar also available in Portable Document Format (PDF)
Douglas G. Fish, MD
Medical Director, Division of Program Development & Management
Carlos Cuevas
Senior Policy Advisor
Logan Tierney
Health Programs Administrator
New York State Department of Health
March 16, 2017
Agenda
| Topic | Presenter | Duration |
|---|---|---|
| NEW: Program Flexibility and Resources | Carlos Cuevas | 10 min |
| VBP Pilot Quality Measure Sets: Measurement Year 2017 Updates | Doug Fish, MD | 30 min |
| MAPP Overview | Logan Tierney | 10 min |
| Open Forum | Carlos Cuevas | 10 min |
NEW: Program Flexibility and Resources
Carlos Cuevas
NEW: VBP Pilot Program Flexibility
As part of the Program, VBP Pilot Participants are required to:
- Submit a VBP contract (or contract addendum) by April 1, 2017, with an effective contract
date of no later than January 1 (effective date may be retroactive, for contracts signed
between January 1, 2017 and April 1, 2017)
Given feedback from pilot participants, particularly concerns around data sharing, the DOH is willing to establish a grace period allowing pilots to leave the program after submitting signed contracts.
Pilots that leave the program will become ineligible for Pilot Program Funding. The DOH will communicate the duration of the grace period by the end of the month.
Evaluation of Variations in Attribution and Target Budgets
The DOH will be issuing further guidance around Pilot attribution and target budgets questions. Current background on any discrepancies in information shared is as follows:
| Attribution | Target Budgets | |
|---|---|---|
| Attribution requirements were updated to better measure continuous enrollment. Updates to enrollment requirements included:
|
Target budgets may have been different from VBP calculations, as a result of the following factors:
|
Requirements for VBP Pilots Contracting
The following elements must be in alignment with the VBP Roadmap:
- VBP Arrangement Type and Level (On Menu)
- Attribution*
- Provider Network*
- Contract Period*
- Target Budget*
- Shared Savings / Losses Allocation*
- Quality Measures
- Exclusions*
- Financial Protections (e.g. Stop Loss)*
Further information is available in the VBP Pilot Contracting Webinar
* Negotiable contracting elements
Available Resources for Contracting
For further support in moving forward with VBP contracting, the following documents are now final and available on the DOH website:
- New York Department of Health Provider Contract Guidelines for Article 44 MCOs, IPAs, and ACOs
- Standard Clauses for Managed Care Provider/IPA/ACO Contracts
- Provider Contract Statement and Certification Form (DOH–4255)
These materials can be found here.
|top of section| |top of page|VBP Pilot Quality Measure Sets: Measurement Year 2017 Updates
Douglas G. Fish, MD
Quality Measure Updates
- Quality Measures – Introduction
- Measure Classification
- Categories 1, 2, and 3
- Pay for Performance (P4P) / Pay for Reporting (P4R)
- Quality Measure Sets – Updates
- Total Care for the General Population (TCGP) and Integrated Primary Care (IPC)
- Maternity
- Total Care for Special Needs Subpopulations
- HIV/AIDS
- Health and Recovery Plans (HARP)
- Final 2017 Measure Count
Value Based Payment Program (VBP) Measurement Year 2017 Quality Measure Sets
- During the first VBP Pilot webinar held on February 24, 2017, outcomes of the State´s VBP Measures feasibility review were presented. On March 3rd, the State met with Managed Care Organization (MCO) Medical Directors and their Quality Teams to gain additional feedback. On March 7th the final recommendations were presented and approved by the VBP Workgroup.
- The Measurement Year (MY) 2017 Quality Measure Sets for the TCGP and IPC arrangements have been completed. Maternity, HIV/AIDS Subpopulation, and Health and Recovery Plans (HARP) Subpopulation VBP measure sets have been updated. (Link)
- Additional measure sets supporting the Managed Long Term Care (MLTC) VBP arrangements are under final review.
MEASURE CLASSIFICATION
- In 2016, the CAGs published measure recommendations to the State for each VBP arrangement. Upon receiving the CAG recommendations, the State conducted further feasibility review and analysis to define a final list of measures for inclusion during MY 2017.
- The final measure sets include measures classified by category based on an assessment of reliability, validity, and feasibility; and according to suggested method of use (either P4R or P4P).
Categorizing and Prioritizing Quality Measures
CATEGORY 1
Approved quality measures that are felt to be both clinically relevant, reliable and valid, and feasible.
CATEGORY 2
Measures that are clinically relevant, valid, and probably reliable, but where the feasibility could be problematic. These measures should be investigated during the 2017 pilot program.
CATEGORY 3
Measures that are insufficiently relevant, valid, reliable and/or feasible.
Category 1 Measures
Category 1 quality measures as identified by the CAGs and accepted by the State are to be reported by VBP Contractors.
The State classified each Category 1 measure as either P4P or P4R:
Pay for Performance (P4P)
- Measures designated as P4P are intended to be used in the determination of shared savings amounts for which VBP Contractors are eligible.
- Performance on the measures can be included in both the determination of the target budget and in the calculation of shared savings for VBP Contractors.
Pay for Reporting (P4R)
- Measures designated as P4R are intended to be used by MCOs to incentivize VBP Contractors for reporting data to monitor quality of care delivered to members under the VBP contract.
- MCOs and VBP Contractors will be incentivized based on timeliness, accuracy & completeness of data reporting.
Measures can move from P4R to P4P through the annual CAG and State review process or as determined by the MCO and VBP Contractor.
Category 2 and 3 Measures
Category 2
- Category 2 measures have been accepted by the State based on agreement of measure importance, but flagged as presenting concerns regarding implementation feasibility.
- The State requires that VBP Pilots make a good faith effort to explore reporting feasibility for Category 2 measures, by including them in their contracting arrangements where possible.
- Plans should include a minimum of two Category 2 measures to report on in their contracting arrangements, or have a State and Plan approved alternative.
- VBP Pilot participants will be expected to share meaningful feedback on the feasibility of Category 2 measures when the CAGs reconvene. The State will discuss measure testing approach, data collection, and reporting requirements with VBP pilots at a future date.
Category 3
- Category 3 measures were identified as unfeasible at this time or as presenting additional concerns including accuracy or reliability when applied to the attributed member population for the VBP arrangement. These measures will not be tested in pilots or included in VBP at this time.
VBP Quality Measure Sets – Measurement Year 2017
- The 2017 VBP Measure Sets have been provided by the State as a recommendation; all Category 1 measures must be reported.
- Implementation is to be determined between the MCO and VBP Contractor.
- Measure sets and classifications are considered dynamic and will be reviewed annually.
- Updates will include additions, deletions, reclassification of measure category, and reclassification from P4R to P4P based on experience with measure implementation in the prior year.
- During 2017, the CAGs and the VBP Workgroup will re–evaluate measures and provide recommendations for Measurement Year 2018.
- An additional measure set supporting the MLTC VBP arrangement is under review and will be made available when completed.
VBP Roadmap* pg. 34
*A Path toward Value Based Payment: New York State Roadmap for Medicaid Payment Reform. Annual Update. June 2016.
VBP Quality Measure Set Annual Review
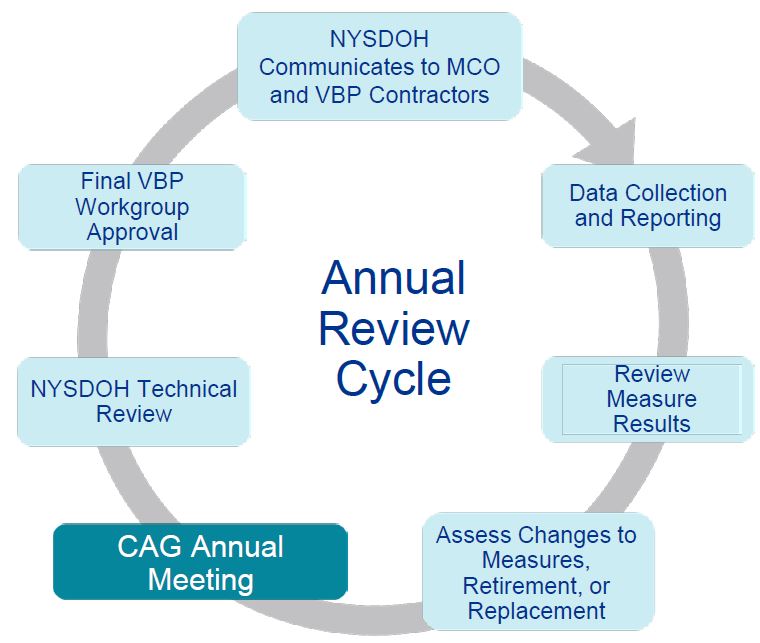
Annual Review
Clinical Advisory Groups will convene to evaluate the following:
- Feedback from VBP Contractors, MCOs, and stakeholders
- Evaluate any significant changes in evidence base of underlying measures and/or measurement gaps
- Review categorization of measures and make recommended changes
State Review Panel
- Review data, technical specification changes or other factors that influence measure inclusion/exclusion*
- Review measures under development to test reliability and validity
- Review measure categorizations from CAG and make recommendations where appropriate (Cat. 1 vs. Cat. 2; P4P vs. P4R)
*DOH policy for inclusion/exclusion criteria within VBP measure sets should mirror other NYSDOH programs
Value Based Payment Program
MY 2017 Measure Sets Updates
TCGP/IPC Measure Set
MY 2017 VBP Measure Set Updates
TCGP/ IPC Quality Measure Set Description & Uses
- TCGP and IPC measure sets were originally separate to allow for additional measures for the TCGP arrangement. There are no specific TCGP measures in 2017, therefore the IPC measure set acts as the main list of measures for TCGP.
- The IPC Measure set is the main list of measures for the IPC arrangement. It also completes the HARP and HIV/AIDs measure sets.
The IPC quality measure set is composed of measures which aim to address:
- Prevention
- Routine Sick Care
- 14 Chronic conditions, to include:
- Physical Health chronic conditions
- Pulmonary
- Diabetes
- Chronic Heart Disease
- Behavioral Health chronic conditions
- Depression & Anxiety
- Substance Use Disorder
- Bipolar Disorder
- Trauma & Stressor
- Physical Health chronic conditions
| VBP Arrangements Using the IPC Quality Measure Set |
|---|
| TCGP |
| IPC |
| HARP Subpopulation |
| HIV/AIDS Subpopulation |
TCGP/IPC – Final Categorization
The following measures were listed as TBD during the February 24, 2017 Pilot webinar. The final classifications are noted below.
| Measure | Measure Steward | Measure Identifier | Classification |
|---|---|---|---|
| Weight Assessment and Counseling for Nutrition and Physical Activity for Children and Adolescents | National Committee for Quality Assurance (NCQA) | NQF 24 | Cat 1 P4P |
| Use of spirometry testing in the assessment and diagnosis of COPD | NCQA | NQF 577 | Cat 1 P4R |
| Continuity of Care (CoC) from Detox or Inpatient Rehab to a lower level of SUD treatment (within 14 days). | NYS Office of Alcoholism and Substance Abuse Services (NYS OASAS) | – | Cat 2 |
| Readmission to mental health inpatient care within 30 days of discharge | NYS Office of Mental Health (OMH) | – | Removed from IPC, remains in HARP |
TCGP/IPC – Category 2 Measures
The draft list of Category 2 IPC measures presented on February 24, 2017 contained 5 measures. The following 6 are in addition to the original 5, bringing the total list to 11 available Category 2 IPC measures.
| Added | Measure Steward | Measure Identifier |
|---|---|---|
| Asthma: Assessment of Asthma Control – Ambulatory Care Setting | The American Academy of Allergy, Asthma & Immunology (AAAAI) | – |
| Avoidance of Antibiotic Treatment in adults with acute bronchitis | NCQA | NQF 58 |
| Continuity of Care (CoC) from Detox or Inpatient Rehab to a lower level of SUD treatment (within 14 days). | NYS OASAS | – |
| Home Management Plan of Care (HMPC) Document Given to Patient/Caregiver (process) | The Joint Commission | NQF 338 |
| Patient Self–Management and Action Plan | AAAAI | – |
| Use of Imaging Studies for Low Back Pain | NCQA | NQF 52 |
Maternity Measure Set
MY 2017 VBP Measure Set Updates
Maternity – Modification to Measures
The following measure was originally classified as a Category 2 Maternity measure. It has been removed and therefore is no longer in the 2017 measure set.
| Measure | Measure Steward | Category |
|---|---|---|
| Neonatal Mortality Rate | AHRQ | Removed |
Total Care for Special Needs Subpopulations
Total Care for Special Needs Subpopulations
Goal: Improve population health through enhancing the quality care for specific subpopulations that often require highly specific and costly care needs.
- Subpopulations include:
- HIV/AIDS
- Health and Recovery Plans (HARP)
- Managed Long Term Care (MLTC)*
- Intellectual and Developmental Disabilities (I/DD)*
- All services covered by the associated managed care plans are included, and all members fulfilling the criteria for eligibility to such plans are included.
- The Category 1 measure sets for HARP and HIV/AIDS Subpopulations include TCGP/IPC measures relevant to each subpopulation.
– – – – – – – – – – – – – – – – – – – – –
Total Population
− TCGP
_____________________
Subpopulations
* Arrangements are still being developed as of 3/16.
HIV/AIDS Measure Set
MY 2017 VBP Measure Set Updates
TCGP/IPC for HIV/AIDS– Measure Feasibility Summary
As communicated during the February 24, 2017 Pilot webinar, the HIV/AIDS measure set includes IPC measures relevant to this population. The following IPC measures are not included in the HIV/AIDS measure set:
| Measure | Rationale for removal | Category |
|---|---|---|
| Childhood Immunization Status | Small sample size + | Cat. 1 |
| Chlamydia Screening for Women | Similar measure already in HIV/AIDS measure set | Cat. 1 |
| Potentially Avoidable Complications in routine sick care or chronic care | There will be a specific HIV/AIDS PAC measure assessed for inclusion in 2018 | Cat. 1 |
| Weight Assessment and Counseling for Nutrition and Physical Activity for Children and Adolescents | Small sample size + | Cat. 1 |
| Avoidance of Antibiotic Treatment in adults with acute bronchitis | Measure excludes HIV/AIDS patients in calculation | Cat. 2 |
| Home Management Plan of Care (HMPC) Document Given to Patient/Caregiver (process) | Small sample size + | Cat. 2 |
| Topical Fluoride for Children at Elevated Caries Risk, Dental Services | Small sample size + | Cat. 2 |
| + The pediatric HIV/AIDS population in NYS is very small, therefore these measures cannot be applied to the VBP | ||
+ The pediatric HIV/AIDS population in NYS is very small, therefore these measures cannot be applied to the VBP Contractor level of measurement.
HARP Measure Set
MY 2017 VBP Measure Set Updates
TCGP/IPC for HARP– Measure Feasibility Summary
As communicated during the February 24, 2017 Pilot webinar, the HARP measure set includes IPC measures relevant to this population. The following IPC measures are not included in the HARP measure set:
| Measure | Rationale for removal | Category |
|---|---|---|
| Antidepressant Medication Management – Effective Acute Phase Treatment & Effective Continuation Phase Treatment | Not applicable to HARP + | Cat. 1 |
| Childhood Immunization Status | Pediatric measure* | Cat. 1 |
| Initiation and Engagement of Alcohol and other Drug Dependence Treatment (IET) | Not applicable to HARP + | Cat. 1 |
| Potentially Avoidable Complications in routine sick care or chronic care | There will be a specific HARP PAC measure assessed for inclusion in 2018 | Cat. 1 |
| Preventive Care and Screening: Screening for Clinical Depression and Follow–Up Plan | Not applicable to HARP + | Cat. 1 |
| Weight Assessment and Counseling for Nutrition and Physical Activity for Children and Adolescents | Pediatric measure* | Cat. 1 |
| Home Management Plan of Care (HMPC) Document Given to Patient/Caregiver (process) | Pediatric measure* | Cat. 2 |
| Topical Fluoride for Children at Elevated Caries Risk, Dental Services | Pediatric measure* | Cat. 2 |
+ HARP members are, by virtue of their eligibility for HARP, exempted from basic screening and follow–up measures more applicable to primary care. *HARP population is 21 years and older.
Final Measure Count
MY 2017 VBP Measure Sets
Measurement Year 2017
VBP Category 1 & 2 Measure Counts
| Category 1 P4P | Category 1 P4R | Category 1 Total | Category 2 P4R | |
|---|---|---|---|---|
| TCGP/IPC | 18 | 11 | 29 | 11 |
| HARP Complete | 18 | 14 | 32 | 9 |
| HARP IPC | 12 | 8 | 20 | 5 |
| HARP Specific | 6 | 6 | 12 | 4 |
| HIV/AIDS Complete | 17 | 13 | 30 | 14 |
| HIV/AIDS IPC | 15 | 10 | 25 | 8 |
| HIV/AIDS specific | 2 | 3 | 5 | 6 |
| Maternity | 2 | 7 | 9 | 9 |
Medicaid Access Patient Portal (MAPP) Tool
Logan Tierney
Goals of the MAPP Tools
1. Background
- Understanding the Data Set
2. Our Network and Attributed Members
- Knowing the population served
- Understanding the network and patient flows
3. Rankings
- How am I doing compared to state average?
- How am I doing compared to my peers?
- Maternity specific performance comparison
4. Looking for opportunities
- How do I understand our (lack of) efficiency and areas of improvement?
- Understanding our (lack of) quality performance and areas of improvement?
5. Performance monitoring
- How am I trending during the contract period on quality and actual costs vs expected?
| For Providers | For NYS / All | For MCOs |
|---|---|---|
|
|
|
VBP Specific Analytics in the MAPP Tool
- Future access to VBP Pilot Organizations, MCO and PPS users will include:
- Expected costs
- Potentially Preventable Readmissions (PPRs), Potentially Preventable Visits (PPVs),
- Risk Adjustments
- Pilots will receive interim reports prior to receiving MAPP access
- These reports should include attribution volumes, costs, and expected costs
Gaining Access to the MAPP Tool
DOH is developing a privacy and security model that will allow organizations with appropriate security plans and agreements to access:
- PHI within MAPP environment and extract member–level performance data for VBP arrangements
- Potentially provide PHI view–only and PHI–with–export access roles
- Real price data within MAPP environment to extract price information specific to provider and arrangement
To gain access, VBP Pilots will need to complete the following steps:
- Execute a Data Use Agreement (DUA) with the DOH
- Establish Health Commerce System (HCS) accounts
- Establish MAPP accounts
Next Steps and Support
- VBP Pilots are expected to sign contracts by 4/1/2017
- 2014 data and report have been made available
- 2015 data is under evaluation, availability is still to be determined
- All submitted contracts are subject to the grace period (period to be determined)
- Pilots can expect periodic check ins with the State to be scheduled
Additional Reference Materials
VBP Support Materials
VBP Resource Library – Final CAG Reports:
- Path: DSRIP Homepage → Value Based Payment Reform → VBP Resource Library – Final CAG Reports
- Link: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_library/vbp_final_cag_reports.htm
VBP Resource Library:
- Path: DSRIP Homepage → Value Based Payment Reform → VBP Resource Library
- Link: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_library
VBP Website:
- Path: DSRIP Homepage → Value Based Payment Reform
- Link: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_reform
Thank you for your ongoing engagement with the VBP Pilot Program.
For additional questions, please contact the VBP mailbox:
vbp@health.ny.gov
Follow Us