Chronic Heart Disease Bundle
Chronic Condition Clinical Advisory Group
Value Based Payment Recommendation Report
- Report is also available in Portable Document Format (PDF)
NYS Medicaid Value Based Payment
September 2016
Introduction
Delivery System Reform Incentive Payment (DSRIP) Program and Value Based Payment (VBP) Overview
The New York State (NYS or the State) DSRIP program aims to fundamentally restructure New York State´s healthcare delivery system, reducing avoidable hospital use by 25%, and improving the financial sustainability of New York State´s safety net.
To further stimulate and sustain this delivery reform, at least 80 – 90% of all payments made from Managed Care Organizations (MCOs) to providers will be captured within VBP arrangements by 2020. The goal of converting to VBP arrangements is to develop a sustainable system, which incentivizes value over volume. The Centers for Medicare & Medicaid Services (CMS) has approved the State´s multiyear VBP Roadmap, which details the menu of options and different levels of VBP that the MCOs and providers can select.
|top of page|Chronic Heart Disease Clinical Advisory Group (CAG)
CAG Overview
For many VBP arrangements, a subpopulation or defined set of conditions may be contracted on an episodic/bundle basis. Clinical Advisory Groups (CAGs) have been formed to review and facilitate the development of each subpopulation or bundle. Each CAG comprises leading experts and key stakeholders from throughout New York State, often including representatives from providers, universities, State agencies, medical societies, and clinical experts from health plans.
The Chronic Heart Disease CAG held a series of three meetings throughout the State and discussed key components of the Chronic Heart Disease VBP arrangement, including bundle definitions, risk adjustment, and the Chronic Heart Disease bundle quality measures. For a full list of meeting dates, times, and overview of discussion, please see Appendix A.
|top of page|Recommendation Report Overview and Components
The following report contains two key components:
Chronic Heart Disease Bundle Playbook
- The playbook provides an overview of the episode definition and clinical descriptions, including ICD–9 and ICD–10 codes:
- Arrhythmia, Heart Block, Conduction Disorders (ARRBLK)
- Coronary Artery Disease (CAD)
- Heart Failure (HF)
- Hypertension (HTN)
Chronic Heart Disease Bundle Quality Measure Summary
- The outcome measure summary provides a description of the criteria used to determine relevancy, categorization and prioritization of outcome measures, and a listing of the recommended outcome measures.
Chronic Heart Disease Bundle Playbook
Chronic Heart Disease Care Definition:
Arrhythmia, Heart Block, and Conduction Disorder Episode;
Coronary Artery Disease Episode;
Heart Failure Episode; and Hypertension Episode
Playbook Overview – Chronic Heart Disease Bundle
New York State´s VBP Roadmap1 describes how the State will transition 80 – 90% of all payments from MCOs to providers from Fee for Service (FFS) to Value Based Payments. "Bundles" or "episodes"2 group together the wide range of services performed for a patient with a specific condition. Episodes only include those services that are relevant to the condition, including services that are routine and typical for the care of the condition. The episode also takes into account services that are required to manage complications that could potentially occur during the course and care of the condition. Episodes open with a claim carrying a "trigger code." Sometimes a confirmatory claim is required in addition to the initial trigger code to confirm an episode exists. Once the episode is opened, it creates a time window where all relevant claims are attributed. Thus, an episode of care is patient–centered and time–delimited. It can be considered as a unit of accounting for budgeting purposes, unit of care for contracting purposes, and a unit for accountability for quality measurement purposes.
New York State uses the HCI3 (Prometheus)–bundled payment methodology, including the standard episode definitions to maximize compatibility and consistency within the State and nationally. More information on how the episodes are developed is available on HCI3´s Web site3. The HCI3–bundled payment methodology is also referred to as "the grouper."
This playbook describes the Chronic Heart Disease Bundle (Arrhythmia, Heart Block, and Conduction Disorder Episode; Coronary Artery Disease Episode; Heart Failure Episode; and Hypertension Episode). The table below provides an overview of the sections in this playbook.
| Section | Short Description |
|---|---|
| Description of Episode | Details on the Arrhythmia, Heart Block, and Conduction Disorder Episode; Coronary Artery Disease Episode; Heart Failure Episode; and Hypertension Episode, including episode triggers and time lines, covered services, exclusions, and potentially avoidable complications |
| Attachment A: Glossary | List of all important definitions |
| Attachment B: Workbooks with Codes for the Episode | Overview of all Arrhythmia, Heart Block, and Conduction Disorder Episode; Coronary Artery Disease Episode; Heart Failure Episode; and Hypertension Episode specific ICD–9 codes as well as their cross–walk to ICD–10 codes |
Description of Episodes - Chronic Heart Disease Bundle
The Arrhythmia, Heart Block, or Conduction Disorder Episode targets Medicaid–only members who have an Arrhythmia, Heart Block, or Conduction Disorder diagnosis.
The Coronary Artery Disease Episode targets Medicaid–only members who have a Coronary Artery Disease diagnosis.
The Heart Failure Episode targets Medicaid–only members who have a Heart Failure diagnosis.
The Hypertension Episode targets Medicaid–only members who have a Hypertension diagnosis.
|top of page|How are the different Chronic Heart Disease Bundle episodes triggered?

Arrhythmia, Heart Block, and Conduction Disorder Episode
The Arrhythmia, Heart Block, and Conduction Disorder Episode is initially triggered by either 1) an inpatient claim with arrhythmia, heart block, or conduction disorder as the principal diagnosis or 2) an outpatient or professional billing claim with an evaluation and management (E&M) service listing Arrhythmia, Heart Block, or Conduction Disorder as the diagnosis. The confirming trigger must adhere to the same parameters as the initial trigger and follow at least 30 days after the initial trigger.4
Coronary Artery Disease Episode
The Coronary Artery Disease Episode is initially triggered by either 1) an inpatient claim with Coronary Artery Disease as the principal diagnosis, 2) an outpatient or professional billing claim with an evaluation and management (E&M) service listing Coronary Artery Disease as the diagnosis, or 3) a combination of related episodes like percutaneous coronary intervention (PCI), complex coronary artery bypass grafting (CXCABG), or acute myocardial infarction (AMI) that have already been triggered separately. The confirming trigger must adhere to the same parameters as the initial trigger and follow at least 30 days after the initial trigger.4
Heart Failure Episode
The Heart Failure Episode is initially triggered by either: 1) an inpatient claim with Heart Failure as the principal diagnosis; 2) an outpatient or professional billing claim with an evaluation and management (E&M) service listing heart failure as the diagnosis; or, 3) a combination of related episodes, like percutaneous coronary intervention (PCI), complex coronary artery bypass grafting (CXCABG), or acute myocardial infarction (AMI) that have already been triggered separately. Each trigger needs a confirming trigger to be finalized. If the initial trigger claim was a professional billing claim, it must be followed by a confirming trigger claim (with the same parameters as the initial trigger) at least 30 days after the initial trigger.4 If the confirming trigger is a related episode like PCI or CXCABG, there is no minimum required time window between the confirming and initial triggers.
Hypertension Episode
The Hypertension Episode is initially triggered by either 1) an inpatient claim with Hypertension as the principal diagnosis, 2) an outpatient or professional billing claim with an evaluation and management (E&M) service listing hypertension as the diagnosis. The confirming trigger must adhere to the same parameters as the initial trigger and follow at least 30 days after the initial trigger.4
|top of page|Which services are included in the Chronic Heart Disease Bundle?
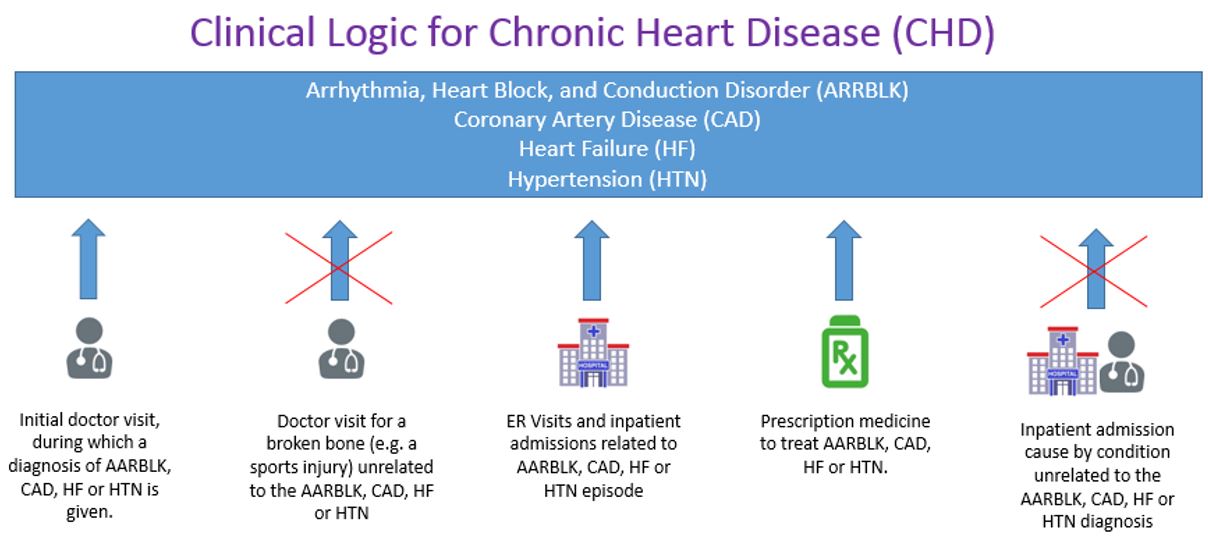
The Chronic Heart Disease Bundle includes all services (inpatient services, outpatient services, ancillary, laboratory, radiology, pharmacy, and professional billing services) related to the care for the specific episode (Arrhythmia, Heart Block, and Conduction Disorder Episode; Coronary Artery Disease Episode; Heart Failure Episode; or Hypertension Episode).5 The visual below provides an example of the services that are/are not included in an episode. The episode includes all care related to that episode, while it excludes encounters where services are provided for unrelated care as defined by the diagnoses (see crossed out services in the example below).
What are the exclusion criteria for the Chronic Heart Disease Bundle?
Some episodes have specific exclusion criteria; these are either exclusions from the episode based on clinical reasons or exclusions from eligibility for Medicaid. Episodes might be excluded from analysis if they are incomplete due to:
- Administrative Exclusion: Incomplete set of claims within the episode time window due to coverage/enrollment gap or lack of episode completion.
- Age: The Arrhythmia, Heart Block, and Conduction Disorder Episode; Coronary Artery Disease Episode; Heart Failure Episode; and Hypertension Episode excludes Medicaid members who are younger than 18 years or older than 65 years.
- Upper and Lower Cost Limit: To create adequate risk models, individual episodes where the episode cost is below the 1st percentile or higher than the 99th percentile are excluded.
- Coverage Gap: For the Arrhythmia, Heart Block, and Conduction Disorder Episode; Coronary Artery Disease Episode; Heart Failure Episode; and Hypertension Episode; continuous member/patient enrollment eligibility is checked for the episode period. If a patient has any enrollment gap during an episode with an episode window 90 days or less or a gap greater than 30 days during episodes with episode window greater than 90 days, then the episode is flagged as not meeting the coverage/enrollment gap criteria.
What is the timeline for an episode within the Chronic Heart Disease Bundle?
Starting from the moment the episode is triggered, there is a 30–day look–back period for care related to the Arrhythmia, Heart Block, and Conduction Disorder; Coronary Artery Disease; Heart Failure; or Hypertension. As Arrhythmia, Heart Block, and Conduction Disorder; Coronary Artery Disease; Heart Failure; and Hypertension are chronic episodes, episodes can be open until the patient is deceased. For reporting purposes, the episode can be assessed on a yearly rolling basis. However, if there are no services related to this episode in a given year, then the episode will not be triggered. If the patient becomes deceased, the date of death marks the end of the episode.

Potentially Avoidable Complications (PACs) related to Chronic Heart Disease Bundle episodes
The services within an episode are assigned as either typical or as potentially avoidable complications. In order to be considered a potentially avoidable complication, or PAC, services must include complication diagnosis codes that either (1) directly relate to the index condition or (2) indicate a failure in patient safety. PACs can occur as hospitalizations, emergency room visits, and professional services related to these hospitalizations, but they can also occur in outpatient settings. As the term indicates, a PAC does not mean that something has gone wrong: it means that a type of care was delivered related to a clinical event that may have been preventable. As such, the goal is not to reduce PACs to zero, but to reduce PACs as much as possible, and to benchmark the risk–adjusted occurrences of these PACs between VBP contractors and MCOs.
Additionally, from a quality perspective, PACs can be identified by failure to comply with patient safety guidelines, such as HACs (CMS defined Hospital–Acquired Conditions) and PSIs (Agency for Healthcare Research and Quality (AHRQ) defined Patient Safety Indicators). Likewise, failure to avoid other situations related to patient safety (e.g. avoidable infection or drug interaction) may also be considered a PAC.
The top 10 PACs for each episode (based on cost) in New York State Medicaid are:
| Arrhythmia, Heart Block, and Conduction Disorder |
|---|
| 1. Pneumonia |
| 2. Acute CHF / pulmonary edema |
| 3. Sepsis |
| 4. Stroke |
| 5. Acute esophagitis, acute gastritis, duodenitis |
| 6. Acute myocardial infarction |
| 7. Respiratory failure |
| 8. Diabetes, poor control |
| 9. Fluid electrolyte acid base problems |
| 10. Acute renal failure |
| Coronary Artery Disease |
|---|
| 1. Acute myocardial infarction |
| 2. Acute CHF / pulmonary edema |
| 3. Stroke |
| 4. Sepsis |
| 5. Pneumonia |
| 6. Percutaneous coronary intervention |
| 7. Diabetes, poor control |
| 8. Complex coronary artery bypass grafting |
| 9. Malfunction / complication of heart device |
| 10. Hypotension / syncope |
| Heart Failure |
|---|
| 1. Acute CHF / pulmonary edema |
| 2. Acute myocardial infarction |
| 3. Sepsis |
| 4. Respiratory failure |
| 5. Pneumonia |
| 6. Stroke |
| 7. Acute renal failure |
| 8. Malfunction / complication of =heart device |
| 9. Urinary tract infection |
| 10. Fluid electrolyte acid base problems |
| Hypertension |
|---|
| 1. Stroke |
| 2. Diabetes, poor control |
| 3. Pneumonia |
| 4. Acute myocardial infarction |
| 5. Sepsis |
| 6. Acute esophagitis, acute gastritis, duodenitis |
| 7. Acute CHF / pulmonary edema |
| 8. Acute renal failure |
| 9. Hypotension / syncope |
| 10. GI Bleed |
Chronic Heart Disease Bundle episode roll up
Arrhythmia, Heart Block, and Conduction Disorder Episode
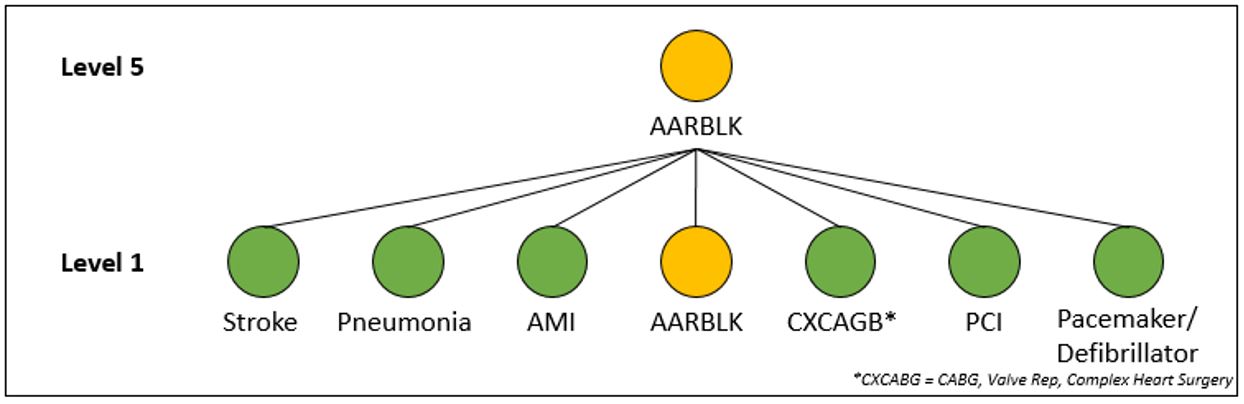
The overarching clinical logic of HCI3´s PROMETHEUS Analytics© allows a member to have multiple concurrent open episodes that can be linked together when clinically relevant. Episodes can be analyzed individually based on their included services or rolled up into more comprehensive bundles through clinical association.
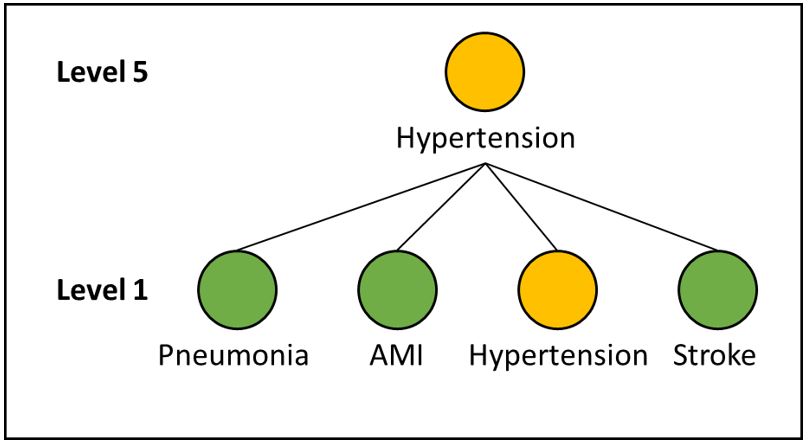
The HCI3 grouper looks at episodes at different levels. At level 1, all episodes are analyzed individually. At higher levels (2 to 5), different episodes are rolled up under one specific episode as PACs.
The costs for complex heart surgery/coronary artery bypass graft (CXCABG), percutaneous coronary intervention (PCI), and pacemaker/defibrillator episodes are rolled up into the Arrhythmia, Heart Block, and Conduction Disorder Episode as both PACs and typical costs at that level.
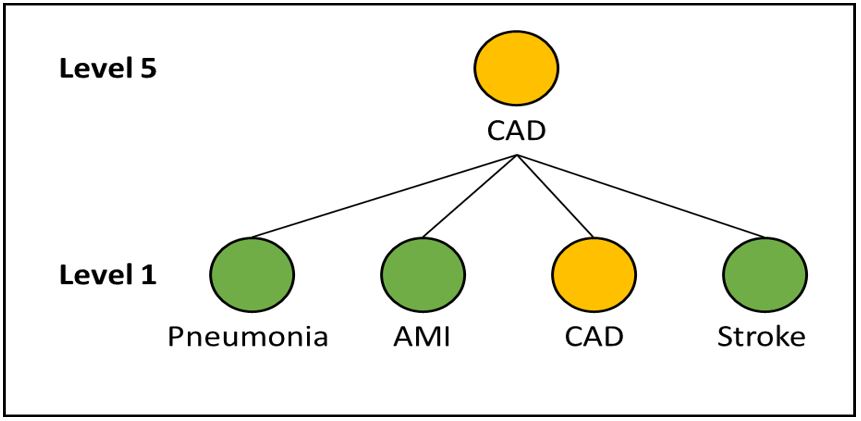
Coronary Artery Disease Episode
Specifically for coronary artery disease at level 5, acute myocardial infarction (AMI), stroke, and pneumonia are rolled up as PACs under the Coronary Artery Disease Episode.
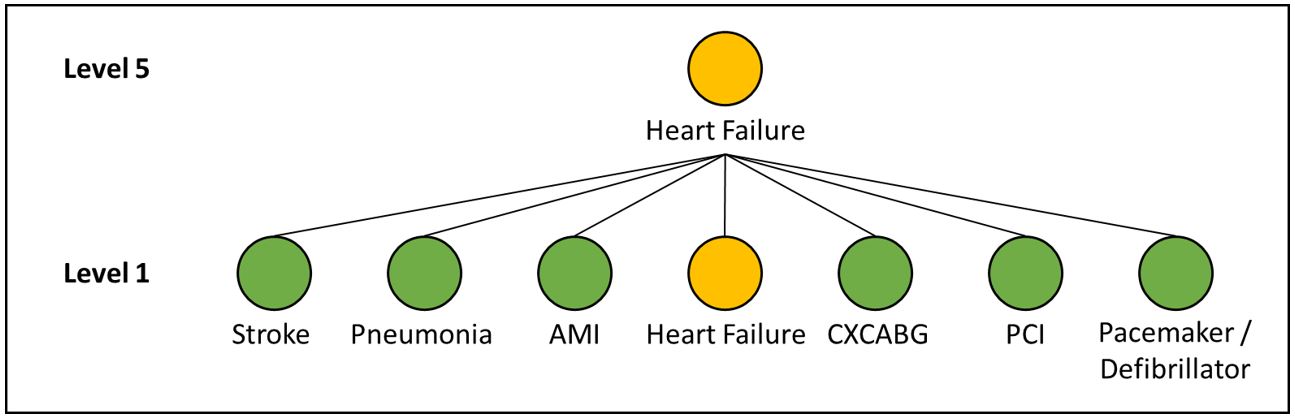
Heart Failure Episode
Specifically for heart failure, at level 5, CHF–related acute myocardial infarction (AMI), pneumonia, and stroke episodes are rolled up as PACs under the Heart Failure Episode. Complex heart surgery/Coronary Artery bypass grafting (CABG), percutaneous coronary intervention (PCI), and pacemaker/defibrillator episodes are rolled up into the Heart Failure Episode as both PACs and typical costs at that level.
Hypertension Episode
Specifically for hypertension, at level 5, acute myocardial infarction (AMI), stroke, and pneumonia are rolled up as PACs under the Hypertension Episode.
Which subtypes of the Chronic Heart Disease Bundle exist?
"Subtypes" are subgroupings that could help stratify a population for analytic purposes and are used for functions such as risk adjustment. A few examples of common subtypes are below:
Arrhythmia, Heart Block, and Conduction Disorder Episode
- Atrial flutter / fibrillation
- Complication of implanted device, graft
- Electrophysiology studies
- Heart aneurysm and other sequelae of AMI
Coronary Artery Disease Episode
- Previous coronary artery bypass grafting (CABG)
- Percutaneous coronary intervention
- Unstable angina
Heart Failure Episode
- Cardiomyopathy
- Diastolic heart failure
- Hypertensive heart disease with heart failure
- Hypertensive heart disease with heart failure and Chronic Kidney Disease (CKD)
- Pulmonary heart disease
Hypertension Episode
- Hypertensive heart disease
- Renovascular and other secondary hypertension
The overview of all subtypes can be found in Attachment B.
|top of page|How is the risk adjustment for the Chronic Heart Disease Bundle done?
Separate risk adjustment models are created for "typical" services and for "potentially avoidable complications." Risk factors that are taken into account include patient demographics, pre–existing co–morbidities, and subtypes.6 Using these factors, the episode grouper calculates an "expected" total cost that is unique for every individual patient. The difference between the actual cost and the expected cost determines the savings/losses incurred in the care for that individual patient. 7
|top of page|ICD–9 and ICD–10 Codes
A list of all relevant codes contained in each HCI3 episode definition can be found here.8
|top of page|Attachment A: Glossary
- Complication Code: These are ICD–9 and ICD–10 diagnosis codes, which are used to identify a Potentially Avoidable Complication (PAC) services during the episode time window.
- Diagnosis Codes: These are unique codes based on ICD–9 (or ICD–10) that are used to group and categorize diseases, disorders, symptoms, etc. These identify clinically–related inpatient, outpatient, and professional typical services to be included in the episode in conjunction with the relevant procedure codes. These may include trigger codes, signs and symptoms and other related conditions and are used to steer services into an open episode.
- Episode: An episode of medical care that spans a predefined period of time for a particular payer–provider–patient triad, as informed by clinical practice guidelines and/or expert opinion. The episode starts after there is a confirmed trigger for that episode (e.g. a diagnosis).
- Episode Type: Episodes are grouped into four main categories:
- Chronic Condition – care for a chronic medical condition.
- Acute Condition – care for an acute medical condition.
- Procedural (Inpatient (IP) or Outpatient (OP)) – a surgical procedure and its follow–up care; the procedure may treat a chronic or acute condition.
- Other Condition – care for pregnancy and cancer episodes.
- In addition, there is one generic episode type included:
- System–Related Failures – inpatient and follow–up care for a condition caused by a systemic patient–safety failure.
- Exclusions: Some episodes have specific exclusion criteria, which are either based on clinical or administrative (eligibility/coverage) criteria.
- ICD–10 Codes: The ICD–9 diagnosis codes and the ICD–9 procedure codes for the above categories of codes have been cross–walked to ICD–10 codes leveraging the open–source GEM (Generalized Equivalence mapping) tables published by CMS.
- Index Condition: The index condition refers to the specific episode that the PAC relates to.
- Initial and Confirming Triggers: An initial trigger initiates an episode based on diagnosis and / or procedure codes found on institutional or non–institutional claims. For many episodes, a second trigger, the confirming trigger, is necessary to actually trigger the episode. Sometimes an episode itself could serve as a trigger for another episode, e.g., pregnancy episode in delivery episode.
- Clinical Association: HCI3´s PROMETHEUS Analytics© allows episodes to be connected to one another based on clinical relevance. For any individual patient, conditions and treatments, all of which trigger different episodes, are often related to one another from a clinical perspective. Episodes can be linked together for the analysis of their costs as either typical or complication.
- Look–Back & Look–Forward: From the point at which an episode is triggered, episode costs / volume are evaluated within the associated time window for a predetermined number of days before and after the trigger date. Costs, volume, and other episode components that fall within this range are captured within the episode.
- Pharmacy Codes: These are codes used to identify relevant pharmacy claims to be included in the episode. HCI3´s PROMETHEUS Analytics© groups pharmacy NDC codes into higher categories using the National Library of Medicine´s open–source RxNorm system of drug classification.
- Potentially Avoidable Complication (PAC): An episode contains services that are assigned as either typical or as potentially avoidable complications. In order to be considered a potentially avoidable complication, or PAC, services must include complication diagnosis codes that either (1) directly relate to the index condition or (2) indicate a failure in patient safety. PACs can occur as hospitalizations, emergency room visits, and professional services related to these hospitalizations, but they can also occur in outpatient settings. As the term indicates, a PAC does not mean that something has gone wrong: it means that a type of care was delivered related to a clinical event that may have been preventable. As such, the goal is never to reduce PACs to zero, but to reduce PACs as much as possible, and to benchmark the risk–adjusted occurrences of these PACs between VBP contractors and MCOs.
Additionally, PACs can be identified by failure to comply with patient safety guidelines, such as HACs (CMS defined Hospital–Acquired Conditions) and PSIs (Agency for Healthcare Research and Quality (AHRQ) defined Patient Safety Indicators). Likewise, failure to avoid other situations related to patient safety (e.g. avoidable infection or drug interaction) may also be considered a PAC. - Procedure Codes: These are codes used to identify clinically–related services to be included in the episode in conjunction with the typical diagnosis codes. These include CPT, HCPCS, and ICD–9 and ICD–10 procedure codes.
- Roll–Ups: Some episodes are associated with each other through HCI3´s PROMETHEUS Analytics© clinical logic and grouped under an ´umbrella´ episode, including the grouped episode´s costs/volume.
- Subtypes (code): Episodes often have subtypes or variants, which are useful to adjust for the severity of that episode, and reduce the need to have multiple episodes of the same type.
- Time–Window: This defines the time that an episode is open. It includes the trigger event, a look–back period and a look–forward period and could be extended based on rules and criteria.
- Trigger Code: A trigger code is the diagnosis or procedure code indicating the condition in question is present or procedure in question has occurred. Trigger codes are used to open new episodes and assign a time window for the start and end dates of each episode (depending on the episode type). Trigger codes can be ICD–9 or ICD–10 diagnosis or procedure codes, CPT or HCPCS codes, and could be present on an inpatient facility, outpatient facility, or professional claim.
Attachment B: Workbooks with Codes for the Chronic Heart Disease Bundle
| Arrhythmia, Heart Block, and Conduction Disorder Episode: | |
|---|---|
| The file below includes all ICD–9 Arrhythmia, Heart Block, and Conduction Disorder–specific codes. | The files below includes all ICD–10 Arrhythmia, Heart Block, and Conduction Disorder–specific codes. |
| ARRBLK: ICD–9 codes | Coming Soon |
| Coronary Artery Disease Episode: | |
|---|---|
| The file below includes all ICD–9 Coronary Artery Disease–specific codes. | The files below includes all ICD–10 coronary artery disease–specific codes. |
| CAD: ICD–9 codes | Coming Soon |
| Heart Failure Episode: | |
|---|---|
| The file below includes all ICD–9 Heart Failure–specific codes. | The files below includes all ICD–10 heart failure–specific codes. |
| CHF: ICD–9 codes | Coming Soon |
| Hypertension Episode: | |
|---|---|
| The file below includes all ICD–9 Hypertension–specific codes. | The files below includes all ICD–10 hypertension–specific codes. |
| Hypertension: ICD–9 codes | Coming Soon |
|top of page|
Chronic Heart Disease Quality Measure Summary
Chronic Heart Disease Clinical Advisory Group (CAG)
Quality Measure Recommendations
Introduction
Over the course of three meetings, the Chronic Heart Disease CAG has reviewed, discussed, and provided feedback on four individual Chronic Heart Disease bundles that will inform value based payment contracting for levels one through three. The Chronic Heart Disease bundles include the following conditions: Arrhythmia, Heart Block, and Conduction Disorders (ARRBLK); Coronary Artery Disease (CAD); Heart Failure (HF); and Hypertension (HTN). All bundles related to Chronic Heart Disease include a significant overlap of quality measures that are relevant for several conditions simultaneously. As a result, a single Chronic Heart Disease CAG and summary document was assembled to ensure both the unique attributes specific to each bundle, as well as areas of overlap (such as quality measures), were captured.
A key element of these discussions was the review of the current, existing, and new outcome and process measures used to measure the quality of care related to the Chronic Heart Disease bundles. This document summarizes the discussion of the CAG and their categorization of quality measures.9
Selecting quality measures: criteria used to consider relevance:10
In reviewing potential quality measures for utilization as part of a VBP arrangement, a number of key criteria have been applied across all Medicaid member subpopulations and disease bundles. These criteria, and examples of their specific implications for the Chronic Heart Condition VBP arrangement, are the following:
Clinical relevance
Focused on key outcomes of integrated care process
i.e. outcome measures (postpartum depression) are preferred over process measures (screening for postpartum depression); outcomes of the total care process are preferred over outcomes of a single component of the care process (e.g. the quality of one type of professional´s care)
For process measures: crucial evidence–based steps in integrated care process that may not be reflected in the patient outcomes measured
i.e. focus on postpartum contraceptive care is key but will not be captured in outcomes of current maternity episode
Existing variability in performance and/or possibility for improvement
i.e., blood pressure measurement during pregnancy is unlikely to be lower than >95% throughout the State
Reliability and validity
Measure is well established by reputable organization
By focusing on established measures (owned by e.g. NYS Office of Patient Quality and Safety (OQPS), endorsed by the National Quality Forum (NQF), Healthcare Effectiveness Data and Information Set (HEDIS) measures and/or measures owned by organizations such as the Joint Commission, the validity and reliability of measures can be assumed to be acceptable.
Outcome measures are adequately risk–adjusted
i.e. measuring ´% preterm births´ without adequate risk adjustment makes it impossible to compare outcomes between providers
Feasibility
Claims–based measures are preferred over non–claims based measures (clinical data, surveys)
i.e. ease of data collection data is important and measure information should not add unnecessary burden for data collection
When clinical data or surveys are required, existing sources must be available
i.e. the vital statistics repository (based on birth certificates) is an acceptable source, especially because OQPS has already created the link between the Medicaid claims data and this clinical registry
Data sources preferably are patient–level data
Measures that require random samples (e.g. sampling patient records or using surveys) are less ideal because they do not allow drill–down to patient level and/or adequate risk–adjustment, and may add to the burden of data collection. An exception is made for such measures that are part of DSRIP/QARR.
Data sources must be available without significant delay
i.e. data sources should not have a lag longer than the claims–based measures (which have a lag of six months). This is an issue with the vital statistics repository, for example, which have a one year lag (at least for the NYC data).
Meaningful and actionable to provider improvement in general
Measures should not only be related to the goals of care, but also something the provider can impact or use to change care.
|top of page|Categorizing and prioritizing quality measures
Based on the above criteria, the CAG discussed the quality measures in the framework of three categories:
- Category 1 – Category 1 comprises approved quality measures that are felt to be clinically relevant, reliable, valid, and feasible.
- Category 2 – Category 2 quality measures were felt to be clinically relevant, valid, and probably reliable, but where the feasibility could be problematic. These quality measures will likely be investigated during the 2016 or 2017 pilots but would likely not be implementable in the immediate future.
- Category 3 – Category 3 measures were decided to be insufficiently relevant, valid, reliable, and/or feasible.
Ultimately, the use of these measures, particularly in Category 1 and 2 will be developed and further refined during the 2016 (and possibly 2017 pilots). The CAG will be re-assembled on a yearly basis during at least 2016 and 2017 to further refine the Category 1 and 2 measures.
The HCI3 grouper creates condition–specific scores for Potentially Avoidable Complications (PACs) for each condition. The ´percentage of total episode costs that are PACs is a useful measure to look for potential improvements; it cannot be interpreted as a quality measure. PAC counts however, can be considered clinically relevant and feasible outcome measures.
______________________________________________________
1. https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/docs/vbp_roadmap_final.pdf. 1
2. The terms can be used interchangeably. Sometimes, the term "bundle" is used to refer to a combination of individual episodes. 2
3. http://www.hci3.org/content/online–courses 3
4. Attachment B lists all codes for the Arrhythmia, Heart Block, and Conduction Disorder Episode; Coronary Artery Disease Episode; Heart Failure Episode; and Hypertension Episode. 4
5. Attachment B lists all codes for the Arrhythmia, Heart Block, and Conduction Disorder Episode; Coronary Artery Disease Episode; Heart Failure Episode; and Hypertension Episode 5
6. For details on risk adjustment, visit the HCI3 Web site (http://www.hci3.org/content/online–courses) 6
7. The overall total savings/losses per bundle are calculated by adding all these savings/losses at the individual episode level. 7
8. Please note that these codes may be different than those found in the Episode table below which contains codes being used specifically for NYS. 8
9. The following sources were used to establish the list of measures to evaluate: existing DSRIP/QARR measures; AHRQ PQI/IQI/PSI/PDI measures; CMS Medicaid Core set measures; other existing statewide measures; NQF-endorsed measures; measures suggested by the CAG. 9
10. After the Measurement Evaluation Criteria established by the National Quality Forum (NQF), 10
Chronic Heart Disease CAG Recommended Quality Measures – Category 1 and 2
| # | Bundle | Measure | Measure Steward/Source | |
|---|---|---|---|---|
| Category 1 | 1 | ARRBLK, CHF | Heart failure: left ventricular ejection fraction assessment (Outpatient Setting) * | American College of Cardiology |
| 2 | CHF, CAD, HTN | Ischemic Vascular Disease (IVD): blood pressure control* | National Committee for Quality Assurance | |
| 3 | CHF, CAD, HTN | Controlling high blood pressure* | Centers for Medicare & Medicaid Services | |
| 4 | CHF | Post-discharge appointment for heart failure patients* | The Joint Commission | |
| 5 | CHF | Post-discharge evaluation for heart failure patients* | The Joint Commission | |
| 6 | CHF | Heart failure: Angiotensin-Converting Enzyme (ACE) inhibitor or Angiotensin Receptor Blocker (ARB) therapy for Left Ventricular Systolic Dysfunction (LVSD) * | American College of Cardiology | |
| 7 | CHF | Heart Failure: beta-blocker therapy for Left Ventricular Systolic Dysfunction (LVSD) * | American College of Cardiology | |
| 8 | CAD, CHF | CAD: Angiotensin-Converting Enzyme (ACE) inhibitor or Angiotensin Receptor Blocker (ARB) therapy–diabetes or Left Ventricular Systolic Dysfunction (LVEF < 40%)* | American College of Cardiology | |
| 9 | CAD, CHF | CAD: beta-blocker therapy–prior Myocardial Infarction (MI) or Left Ventricular Systolic Dysfunction (LVEF <40%)* | AMA-convened Physician Consortium for Performance Improvement | |
| 10 | CAD, CHF, HTN | Proportion of Days Covered (PDC): three rates by therapeutic category (% of patients who met the Proportion of Days Covered (PDC) threshold of 80 percent during the measurement year for RAS antagonists, diabetes medication or statins) * | Pharmacy Quality Alliance | |
| 11 | ARRBLK, CAD, CHF, HTN | Proportion of patients with a chronic condition that have a potentially avoidable complication during a calendar year. | Bridges To Excellence | |
| Category 2 | 12 | ARRBLK, CAD, CHF, HTN | Assessment of thromboembolic risk factors (CHADS2) * | American College of Cardiology |
| 13 | ARRBLK, CAD, CHF, HTN | Medical assistance with smoking cessation | National Committee for Quality Assurance | |
| 14 | CHF | Hospital 30-day, all-cause, risk- standardized mortality rate (RSMR) following heart failure (HF) hospitalization for patients 18 and older. | Centers for Medicare & Medicaid Services | |
| 15 | CHF | In hospital heart failure mortality rate* | Agency for Healthcare Research and Quality | |
| *= NQF Endorsed Bundle Key: Arrhythmia, Heart Block, Conduction Disorders (ARRBLK), Coronary Artery Disease (CAD), Heart Failure (HF), Hypertension (HTN). |
||||
CAG categorization and discussion of measures
| Topic | Bundle | # | Quality Measure (* = NQF Endorsed) | Type of Measure | Measure Steward/ Source | DSRIP | QARR | HEDIS | Data Required | Quality Measure Categorization & Notes | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Medicaid Claims Data | Clinical Data 1 | Category | Notes | |||||||||
| Prevention/Monitoring | ARRBLK, CAD, CHF, HTN | 1 | Cholesterol management for patients with cardiovascular conditions | Process | National Committee for Quality Assurance | X | X | NO | YES | 3 | At the time of this CAG meeting, Measures 1 and 2 were outdated (DSRIP and HEDIS are in the process of retiring these measures). The new guidelines are more static and only focused on whether or not the screening is performed. The CAG recommends examining if there are other lipid control measures that are more compliant with the new guidelines during the pilot phase. CMS is using an outlier for MCOs' compliance with statins. | |
| Prevention/Monitoring | ARRBLK, CAD, CHF, HTN | 2 | Chronic stable CAD: lipid control* | Process | American College of Cardiology | NO | YES | 3 | Discussed above in Measure #1 | |||
| Prevention/Monitoring | ARRBLK, CHF | 3 | Heart failure: left ventricular ejection fraction assessment (Outpatient Setting) * | Process | American College of Cardiology | NO | YES | 1/2 | The CAG feels strongly about measuring the LVEF value; it should be used for both quality measures and risk adjustment. During the pilot period, the possibilities of incorporating the LVEF value with the claims data will be explored. | |||
| Prevention/Monitoring | ARRBLK, CHF | 4 | Heart failure: symptom and activity assessment* | Process | American College of Cardiology | NO | YES | 3 | Collecting the necessary data to calculate this measure will be a large effort (for the provider, MCO, and the State) because it is mainly based on clinical records. The CAG believes that given all the other quality measures, this measure is not worth the effort. It is easier to get claims data of tests that were ordered based upon patients symptoms. | |||
| Prevention/Monitoring | CHF, CAD, HTN | 5 | Ischemic Vascular Disease (IVD): blood pressure control* | Process | National Committee for Quality Assurance | NO | YES | 1 | The CAG believes this is a good measure and recommend measuring it. Three important points of attention for the pilot phase are:
|
|||
| Prevention/Monitoring | CHF, CAD, HTN | 6 | Controlling high blood pressure* | Process | Centers for Medicare & Medicaid Services | X | X | X | NO | YES | 1 | The CAG recommends using this measure. |
| Prevention/Monitoring | ARRBLK, CAD, CHF, HTN | 7 | Assessment of thromboembolic risk factors (CHADS2) * | Process | American College of Cardiology | NO | YES | 2 | The CAG expects:
|
|||
| Prevention/Monitoring | CHF, CAD, HTN | 8 | Optimal vascular care (% patients who have ischemic vascular disease with optimally managed modifiable risk factors (blood pressure, tobacco-free status, daily aspirin use)) * | Process | MN Community Measurement | NO | NO | 3 | Collecting the data necessary for this measure takes a lot of effort because it requires data from both clinical records and surveys. Given the other measures in this set, the CAG recommends not to use this measure. | |||
| Prevention/Monitoring | ARRBLK, CAD, CHF, HTN | 9 | Medical assistance with smoking cessation | Process | National Committee for Quality Assurance | X | X | X | NO | NO | 2 | The CAG is concerned that this measure is complicated because the data collection is done using patient surveys and may not be worth the effort. The CAG suggests examining if similar data can be collected through claims data. There are already codes for counseling smoking cessation which could be used for the numerator. However, the CAG questions if the data reporting is reliable. Another important qualification would be to see how the denominator can be defined. There are some options used in the field, but the reliability of these are questionable; estimating based on sample size may have too much potential for error (e.g., issues from under reporting). |
| Admission | CHF | 10 | Heart failure admission rate* | Process | Centers for Medicare & Medicaid Services, PQI | YES | YES | 3 | This measure is captured in Measure #14 (Proportion of patients with a chronic condition that have a potentially avoidable complication during a calendar year) and is therefore excluded. | |||
| Admission | CHF | 11 | Hospital 30-day, all-cause, risk-standardized readmission rate (RSRR) following heart failure hospitalization* | Outcome | Centers for Medicare & Medicaid Services | YES | YES | 3 | The CAG does not recommend using this measure. The concern is that the denominator is readmission for any cause as opposed to cases related specifically to heart failure. | |||
| Admission | CAD | 12 | Angina without procedure admission rate | Process | Prevention Quality Indicators | X | X | YES | YES | 3 | This measure is captured in Measure #14 (Proportion of patients with a chronic condition that have a potentially avoidable complication during a calendar year) and is therefore excluded. | |
| Admission | HTN | 13 | Hypertension admission rate | Process | Prevention Quality Indicators | YES | YES | 3 | This measure is captured in Measure #14 (Proportion of patients with a chronic condition that have a potentially avoidable complication during a calendar year) and is therefore excluded. | |||
| Treatment | ARRBLK, CAD, CHF, HTN | 14 | Proportion of patients with a chronic condition that have a potentially avoidable complication during a calendar year. | Outcome | Bridges To Excellence | YES | YES | 1 | This measure captures Measures #10, 12, 13 and will be used instead of each individually. | |||
| Treatment | CHF | 15 | Hospital 30-day, all-cause, risk-standardized mortality rate (RSMR) following heart failure (HF) hospitalization for patients 18 and older. | Outcome | Centers for Medicare & Medicaid Services | YES | YES | 2 | The CAG suggests keeping this measure. However the measurement will need improved transition of care, which will lead to more coordination between outpatient and inpatient care. | |||
| Treatment | CHF | 16 | In hospital heart failure mortality rate* | Outcome | Agency for Healthcare Research and Quality | YES | YES | 2 | Mortality is not included in the PACs for episodes. The CAG believes it is an important measure to capture and recommend examining this during the pilot phase, because the mortality aspect can be vague. There are cases where someone who goes into the hospital with CHD may not want aggressive care. This could give a wrong impression of the results for this measure. | |||
| Treatment | CHF | 17 | Post-discharge appointment for heart failure patients* | Process | The Joint Commission | NO | YES | 1 | The CAG believes it is important to look at the cooperation between inpatient and outpatient care. The CAG recommends investigating whether it is possible to collect the necessary data through clinical data, since there are new codes that capture this type of care. | |||
| Treatment | CHF | 18 | Post-discharge evaluation for heart failure patients* | Process | The Joint Commission | NO | YES | 1 | The CAG believes it is important to look at the cooperation between inpatient and outpatient care. The CAG recommends investigating whether it is possible to collect the necessary data through clinical data, since there are new codes that capture this type of care. | |||
| Treatment | CAD, CHF | 19 | Cardiac stress imaging not meeting appropriate use criteria: Testing in asymptomatic, low risk patients* | Process | American College of Cardiology | NO | YES | 3 | ||||
| Treatment | CHF | 20 | Cardiac Rehabilitation Patient Referral From an Inpatient Setting* | Process | American College of Cardiology | NO | YES | 3 | The CAG considers this measure to be a low priority. First, there is a lack of consistency between facilities. Second, there are various reasons beyond the provider's capability that influence an individual's adherence to rehabilitation regiments. For example, lack of ancillary services or transportation issues. | |||
| Treatment | CHF | 21 | Cardiac Rehabilitation Patient Referral From an Outpatient Setting* | Process | American College of Cardiology | NO | YES | 3 | The CAG considers this measure to be a low priority. First, there is a lack of consistency between facilities. Second, there are various reasons beyond the provider's capability that influence an individual's adherence to rehabilitation regiments. For example, lack of ancillary services or transportation issues. | |||
| Treatment | CAD | 22 | Bilateral cardiac catheterization rate* | Process | Agency for Healthcare Research and Quality | YES | YES | 3 | ||||
| Medication | ARRBLK, CAD, CHF, HTN | 23 | Aspirin discussion and use (% of patients who are currently taking aspirin on a daily or bi-daily basis) | Process | National Committee for Quality Assurance | X | X | NO | NO | 3 | The CAG recommends excluding this measure from the set. The main reason is that there is a large group of patients who refuse aspirin therapy, and the provider has no influence over this. | |
| Medication | CHF, CAD, HTN | 24 | Ischemic Vascular Disease (IVD): use of aspirin or another antithrombotic* | Process | National Committee for Quality Assurance | NO | YES | 3 | The CAG recommends to exclude this measure from the set. The main reason is that there is a large group of Medicaid members who refuse aspirin therapy, and the provider has no influence over this. | |||
| Medication | CHF | 25 | Heart failure: Angiotensin- Converting Enzyme (ACE) inhibitor or Angiotensin Receptor Blocker (ARB) therapy for Left Ventricular Systolic Dysfunction (LVSD)* | Process | American College of Cardiology | NO | YES | 1 | The CAG recommends using this measure. | |||
| Medication | CHF | 26 | Heart Failure: beta-blocker therapy for Left Ventricular Systolic Dysfunction (LVSD)* | Process | American College of Cardiology | NO | YES | 1 | The CAG recommends using this measure. | |||
| Medication | CAD, CHF | 27 | CAD: Angiotensin- Converting Enzyme (ACE) inhibitor or Angiotensin Receptor Blocker (ARB) therapy - diabetes or Left Ventricular Systolic Dysfunction (LVEF < 40%)* | Process | American College of Cardiology | NO | YES | 1 | The CAG recommends using this measure. | |||
| Medication | CAD | 28 | Chronic Stable CAD: antiplatelet therapy (aspirin) * | Process | American College of Cardiology | NO | YES | 3 | The CAG recommends to exclude this measure from the set. The main reason is that there is a large group of Medicaid members who refuse the therapy. Providers have little to no influence over this. | |||
| Medication | CAD, CHF | 29 | CAD: beta-blocker therapy— prior Myocardial Infarction (MI) or Left Ventricular Systolic Dysfunction (LVEF <40%)* | Process | AMA-convened Physician Consortium for Performance Improvement | NO | YES | 1 | The CAG recommends using this measure. | |||
| Medication | CAD, CHF, HTN | 30 | Proportion of Days Covered (PDC): 3 rates by therapeutic category (% of patients who met the Proportion of Days Covered (PDC) threshold of 80% during the measurement year (at least 91 days) for RAS antagonists, diabetes medication or statins) * | Process | Pharmacy Quality Alliance | YES | YES | 1 | The CAG recommends using this measure. | |||
Appendix A:
Meeting Schedule
| Date | Agenda | |
|---|---|---|
| CAG #1 | 8/27/2015 | Part I
|
| CAG #2 | 10/7/2015 | Part I – Short Review and Questions from Previous CAG Meeting Part II – Quality Measures for Chronic Heart Episodes |
| CAG#3 | 10/20/2015 | Short Review and Questions from Previous CAG Meeting |
______________________________________________________
1. Clinical data refers to non-claims data and is information that is often captured on a patient's individual chart or record. 1
|top of page|
Follow Us