Value Based Payment Quality Improvement Program (VBP QIP)
Update Webinar
- Webinar also available in Portable Document Format (PDF)
February 15, 2017
Today´s Agenda
VBP QIP Program Updates
VBP QIP Financing
- The April 2016 rate package was approved at the end of 2016.
- Managed Care Organizations (MCOs) should have received the funds on December 28, 2016.
- MCOs should distribute funds in accordance with their contracts.
- The official recoupment of advances is currently taking place and may occur in multiple cycles
- For any VBP QIP financing questions, please contact bmcr@health.ny.gov
VBP QIP MCO Governance Documents
- Department of Health (DOH) will release the Group 2 MCOs´ Governance Documents by Thursday, February 23rd, 2017.
- DOH will provide feedback to MCOs, which can be used to solidify their approach for overseeing VBP QIP.
- Updates to the governance documents must be submitted by DOH by Friday, March 24th, 2017.
VBP QIP Facility Plan Guidance Document Updates
P4P Measure Changes
- DOH has removed VTE–1 from the menu because CMS removed the measure from the hospital IQR Program as of January 1, 2016.
| # | Measure Name | Data Steward | Focus Area/Domain |
|---|---|---|---|
| 1 | Acute MI Mortality (IQI #15) | AHRQ | Mortality |
| 2 | Stroke Mortality (IQI #17) | AHRQ | Mortality |
| 3 | Pneumonia Mortality (IQI #20) | AHRQ | Mortality |
| 4 | CAUTI Rate per 10,000 Patient Days (Population Rate) | NHSN | Hospital Acquired Conditions |
| 5 | CLABSI per 10,000 Patient Days (Population Rate) | NHSN | Hospital Acquired Conditions |
| 6 | CDI Healthcare Facility – Onset Incidence Rate per 10,000 Patient Days | NHSN | Hospital Acquired Conditions |
| 7 | Falls with Injury | National Quality Forum | Hospital Acquired Conditions |
| 8 | 3–Hour Sepsis Bundle 4 | NYSDOH | Hospital Acquired Conditions |
| 10 | Prevalence Rate of Facility – Acquired Pressure Ulcers of Stage 2 or Higher per 100 Patients | National Quality Forum | Hospital Acquired Conditions |
| 11 | Episiotomy Rate | Christiana Care Health System | Maternity |
| 12 | Primary C–Section (IQI #33) | AHRQ | Maternity |
| 13 | Avoidable ED Use | 3M | Utilization |
| 14 | Avoidable Admissions | 3M | Utilization |
Measure removed
Acronyms: AHRQ (Agency for Healthcare Research and Quality), NHSN (National Healthcare Safety Network)
Pay for Performance (P4P) Measure Denominators
- DOH worked with hospital and plan associations to conduct further analysis on denominators across facilities for the menu of measures.
- The analysis did not reveal any significant issues that would prohibit facilities from meeting thresholds of 30 across a rolling annual calculation for most measures on the menu.
- A denominator of 30 is required for a measure to be deemed valid in a reporting period.
- For questions on VBP QIP quality measures, please email the SPARCS BML at sparcs.submissions@health.ny.gov with "VBP QIP Measures" in the title.
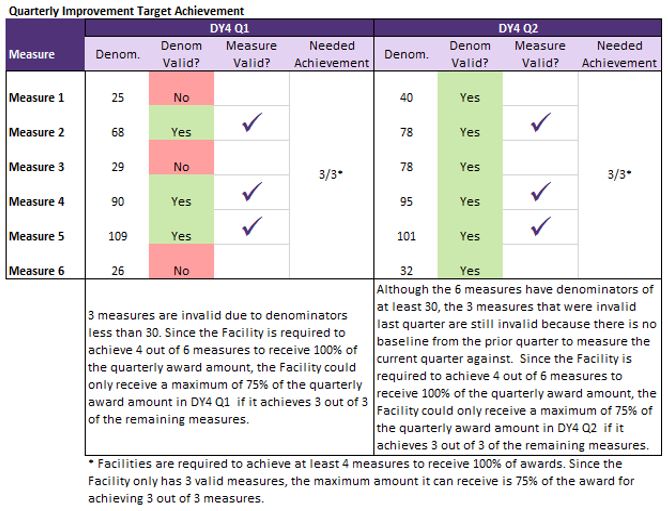
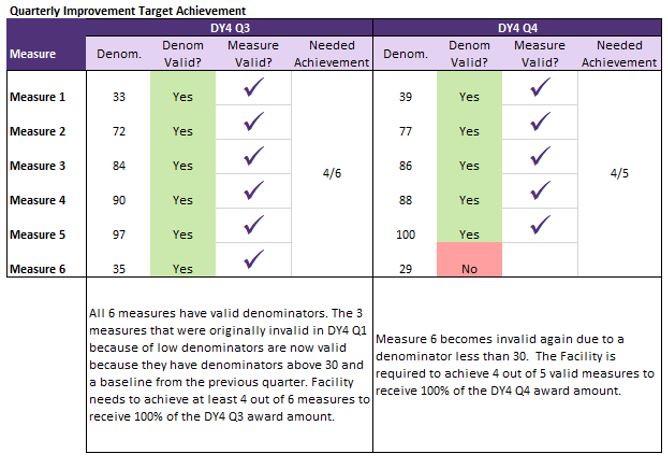
Invalid Denominators
- If a Facility selects a measure where the denominator is less than 30 for a given reporting period, the measure´s performance cannot count as achieved for the reporting period.
- If multiple denominators are invalid during the same reporting period, more of the valid measures will need to be achieved for a facility to earn full payment for the period. Performance for at least 4 measures will need to be achieved in a reporting period for the facility to earn full payment for that period.
- If 3 or more measures have invalid denominators during a reporting period, the facility will earn up to the amount of achieved valid measures. Since less than 4 valid measures can be achieved, unearned P4P dollars will be available through the AIT.
- A measure with a rolling annual denominator less than 30 during a quarterly reporting period will not be valid in the next quarterly reporting period either, because there will not be a valid rolling annual quarter to serve as a baseline.
Please see example on next slide...
Invalid Denominators Example
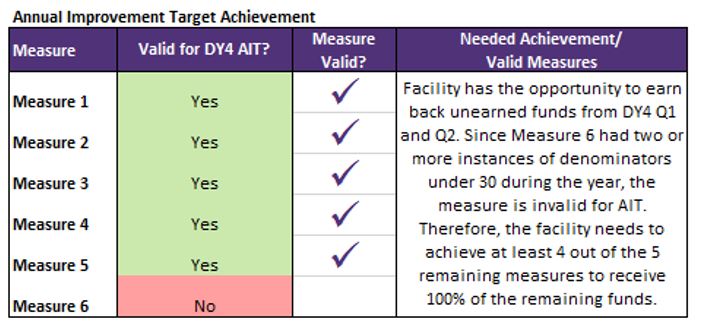
Annual Improvement Target Requirements
- For Demonstration Year (DY) 4 and DY5, the following criteria must be met for a measure to be considered achieved in AIT:
- The Annual Measurement Period result must be better than the Annual Baseline Period result (performance improves over the baseline); AND
- The facility must achieve a result for the Annual Measurement Period that is better than the New York State (NYS) mean results for the specific measure as per the most recently published report by the specified data source (AHRQ, NHSN, National Quality Forum, etc.).
AIT Measures for Comparison
- The mean data in the chart below is the most recent data available for illustrative purposes only.
- The Office of Quality and Patient Safety (OQPS) will release the NYS mean results for DY4 in June 2017. Mean data will be pulled based on the most recent data available as of May 1, 2017.
| # | Measure Name | Data Steward | Focus Area/Domain | Units | Data Source | Period | Rate, Mean (30+ or More Disch) for Illustration Only* |
|---|---|---|---|---|---|---|---|
| 1 | Acute MI Mortality | AHRQ | Mortality | Rate per 1000 Discharges | NYSDOH (SPARCS) | 2014 | 84.26046203 |
| 2 | Stroke Mortality | AHRQ | Mortality | Rate per 1000 Discharges | NYSDOH (SPARCS) | 2014 | 90.30177843 |
| 3 | Pneumonia Mortality | AHRQ | Mortality | Rate per 1000 Discharges | NYSDOH (SPARCS) | 2014 | 39.96730851 |
| 4 | CAUTI Rate | NHSN | Hospital Acquired Conditions | CAUTI Rate per 10,000 Patient Days | CMS | 2015 | 12.7655862 |
| 5 | CLABSI Rate | NHSN | Hospital Acquired Conditions | CLABSI Rate per 10,000 Patient Days | CMS | 2015 | 9.994533256 |
| 6 | CDI Healthcare Facility Rate | NHSN | Hospital Acquired Conditions | CDI Rate per 10,000 Patient Days | CMS | 2015 | 6.025167055 |
| 7 | Falls with Injury | National Quality Forum | Hospital Acquired Conditions | TBD* | |||
| 8 | 3–Hour Sepsis Bundle | NYSDOH | Hospital Acquired Conditions | NYSDOH | TBD** | ||
| 9 | Prevalence Rate of Facility – Acquired Pressure Ulcers of Stage 2 or Higher per 100 Patients | National Quality Forum | Hospital Acquired Conditions | Stage III or IV pressure ulcers or unstageable (secondary diagnosis) per 1,000 discharges among surgical or medical patients ages 18 years and older | NYSDOH (SPARCS), PSI #03 | 2014 | 0.739666475 |
| 10 | Episiotomy Rate | Christiana Care Health System | Maternity | Per 100 Vaginal Deliveries | NYSDOH | 2014 | 15.871 |
| 11 | Primary C– Section (IQI #33) | AHRQ | Maternity | Rate per 1000 Deliveries | NYSDOH (SPARCS) | 2014 | 189.0981354 |
| 12 | Avoidable ED Use | 3M | Utilization | Rate per 100 Discharges | NYSDOH (SPARCS) | 2014 | 72.2285794 |
| 13 | Avoidable Admissions | 3M | Utilization | rate per 100 Admissions | NYSDOH (SPARCS) | 2014 | 23.9662787 |
* This benchmark is currently unavailable and will be released in the future.
Alternate Measure AIT Requirements
- If alternate measures are selected, the facility is responsible for the calculation.
- The facility should use NYS specific data. If State specific data is unavailable, the national mean for the measure can be used.
- In DY4, the facility should use the most recent published reports at May 1, 2017.
- In DY5, the facility should use the most recent published reports at May 1, 2018.
- The paired MCO is responsible for confirming the data sources used for alternate measures.
- For questions on VBP QIP quality measures, please email the SPARCS BML at sparcs.submissions@health.ny.gov with "VBP QIP Measures" in the subject.
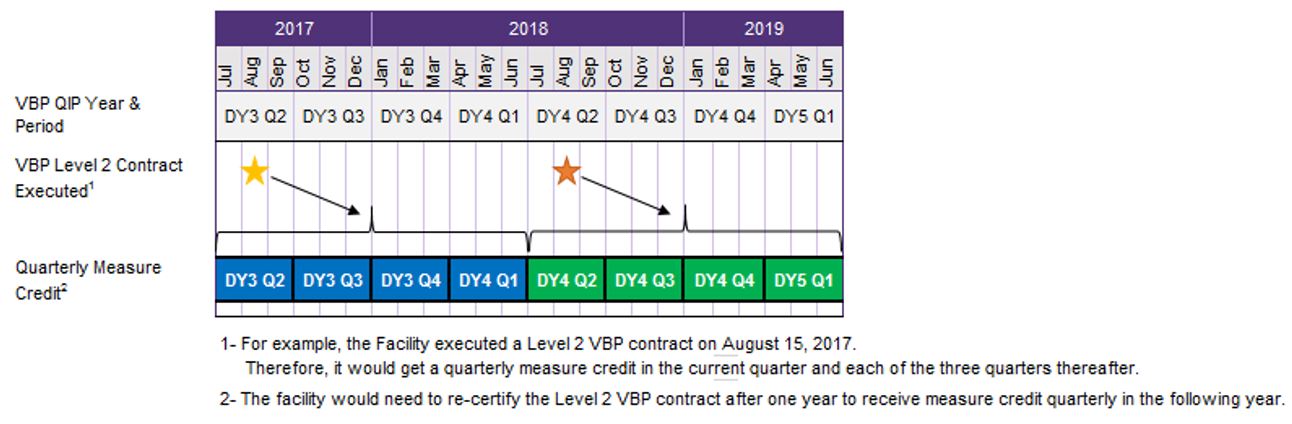
Measure Credits for Quarterly Improvement Target
- Quarterly measure credits will be earned in the quarter the requirement is met and the three subsequent quarters.
- Only one measure credit can be earned per year.
- Unused credits cannot be carried over into future DYs.
- If the Level 2 VBP contract extends through later years, the Facility is required to re-certify that a contract is in place to earn a measure credit for the next year.
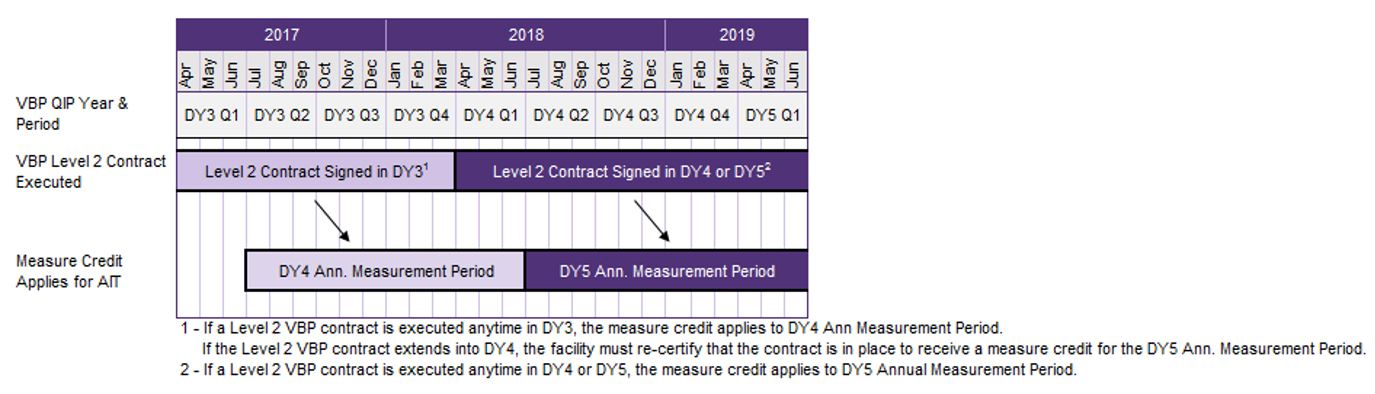
Measure Credits for AIT
- If a Facility has unawarded P4P funds for not meeting its full Quarterly Improvement Target (QIT) during DY4 or DY5, the Facility has a second opportunity to earn these funds by meeting AIT requirements.
- If a Facility has an executed Level 2 or higher VBP contract during DY3, the facility can earn an additional measure credit applied to the DY4 AIT measures. If the Facility has an executed Level 2 or higher VBP contract in DY4 or DY5, the facility can earn an additional measure credit applied to the DY5 AIT measures.
- A Facility can only receive up to ONE measure credit per QIT and AIT calculation.
DY3 Timeline and Q&A
VBP QIP DY3 Timeline
| Milestone | Due Date |
|---|---|
| DOH reviews VBP QIP MCO Governance Document and distributes Scorecard to MCOs (Group 2) | February 23, 2017 |
| VBP QIP – VBP Contracting Webinar (DATE CHANGE) | March 1, 2017 |
| VBP QIP DY3 Guidance Released | March 10, 2017 |
| Facilities submit their updated, MCO approved, Facility Plan to DOH | March 15, 2017 |
| MCOs submit a revised VBP QIP Governance Document to DOH for review (Group 2) | March 24, 2017 |
| Facilities must provide paired MCO with LOI to sign Level 1 VBP contracts with one MCO | April 1, 2017 |
| Facilities must provide paired MCO with list of Medicaid MCOs which the facility expects to enter into VBP contracts with by April 1, 2018 | April 1, 2017 |
| Facilities must have at least one Level 1 VBP contract signed | July 1, 2017 |
| Facilities must provide paired MCO with outstanding LOIs for Medicaid MCOs to contract | July 1, 2017 |
| Facilities must have Medicaid MCO contracts where at least 80% of total Medicaid MCO contracted payments to the Facility are tied to Level 1 VBP components | April 1, 2018 |
Important Information
VBP Support Materials
VBP Resource Library:
- Path: DSRIP Homepage → Value Based Payment Reform → VBP Resource Library
- Link: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_library
VBP Website:
- Path: DSRIP Homepage → Value Based Payment Reform
- Link: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_reform
Thank you for your continued support with VBP QIP!
- The next VBP QIP Update Webinar is scheduled for March 1st from 3:00 pm – 4:00 pm.
- For questions on VBP QIP quality measures, please email the SPARCS BML at sparcs.submissions@health.ny.gov with "VBP QIP Measures" in the title.
- For questions on VBP QIP financing, please contact bmcr@health.ny.gov.
- For other questions on VBP QIP, please contact the VBP QIP inbox at (vbp_qip@health.ny.gov).
Follow Us