Value Based Payment Quality Improvement Program (VBP QIP)
Update Webinar
- Webinar also available in Portable Document Format (PDF)
January 27, 2017
Today´s Agenda
- VBP QIP Program Updates
- VBP QIP Facility Plan Guidance Document
- – P4P Quality Measurement
– P4R VBP Contracting
– Penalties and Measure Credits
– VBP QIP Facility Plan Next Steps
- – P4P Quality Measurement
- DY3 Timeline and Q&A
VBP QIP Program Updates
VBP QIP Financing
- DOH recently received approval for the April 2016 rate package.
- These rates contain funding retro to April 1, 2016 and for the remainder of (SFY) 2016–17 on prospective basis.
- Managed Care Organizations (MCOs) should have received the funds on Wednesday, December 28, 2016.
- The official recoupment of advances should occur in late January or early February 2017 and may occur in multiple cycles.
Note: Department of Health (DOH) recouped advances made to MCOs in error before it had loaded the April 2016 rate package. DOH rectified this issue to ensure that MCOs have sufficient funds to implement the program.
- Please e–mail bmcr@health.ny.gov with any questions that you may have regarding this issue.
VBP QIP MCO Governance Documents
- DOH is set to release their reviews of the Group 2 MCOs´ Governance Documents by Friday, February 17th, 2017.
- DOH will provide feedback to MCOs, which they can use to further solidify their approach for overseeing their VBP QIP program.
- Based upon review, MCOs may update their Governance Documents. Updates will need to be submitted to DOH by Friday, March 24th, 2017.
VBP QIP DY 3 Guidance Packet
- Similar to the VBP QIP Demonstration Year (DY) 2 Guidance Packet that DOH distributed to participants, DOH plans on releasing a VBP QIP DY3 Guidance Packet.
- This document is meant to restate the purpose of the program and provide VBP QIP participants information they need to progress into the third year of the program.
- The Packet is expected to be released by Friday, March 10th, 2017.
VBP QIP Facility Plan Guidance Document
VBP QIP Facility Plan Guidance Document
- DOH distributed Facility Plan "Guidance" Document to program participants earlier today, January 27th, 2017.
- The purpose of this document was to provide participants with guidance on creating Facility Plans and to clarify programmatic parameters around Facility Plan elements.
- Guidance provided in the document includes:
- Program Payments
- Measure Selection
- Measure Reporting
- Measure Evaluation
- VBP Contracting Requirements
- Penalties and Measure Credits
- Program Schedule and Frequently Asked Questions (FAQs)
VBP QIP Annual Payment Distribution
- The Guidance document is broken out into Pay for Reporting (P4R) and Pay for Performance (P4P) activities.
- P4R activities are designed to assess progress made towards VBP contracting arrangements.
- P4P activities are designed to capture improvements in quality through measurement of performance outlined in the Facility Plan.
DY3 DY4 DY5 VBP Contracting Progress (P4R) % 50%
(Paid in Q1 & Q2)20% 0% Performance Improvement (P4P) % 50%
(Paid in Q3 & Q4)80% 100%
- DOH encourages partners to adopt this payment distribution for DY3– DY5.
- P4P payment thresholds should not fall below percentages above for each DY.
- For example, a MCO could accept a Facility Plan with a split of 40% P4R, 60% P4P because it meets the minimum P4P threshold of 50%.
VBP QIP Quarterly Payment Distribution
- As the program progresses, the percentage of funds available for P4R will decrease and become increasingly weighted towards performance measures on quality outcomes.*
- The first two (2) quarters of DY3 will be paid solely based on P4R and the last two (2) quarters will be paid solely based on P4P.
- In DY4, P4R and P4P will occur simultaneously with 20% of funds flowing through P4R and 80% of funds flowing for P4P.
- In DY5, all funds will flow through P4P.
*All percentages are a proportion of annual payments.DY3 DY4 DY5 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 VBP Contracting
Progress (P4R) %25% 25% 20% (split across 4 qtrs.) 0% 5% 5% 5% 5% Performance
Improvement
(P4P) %25% 25% 20% 20% 20% 20% 25% 25% 25% 25%
P4P – Quality Measurement
P4P Measure Requirements
- Each VBP QIP Facility Plan is expected to contain six (6) quality measures for P4P evaluation.
- DOH advises that Facility Plans contain no more than six measures as partners should focus on improving targeted areas.
- Once selected, the facility will be assessed based on the performance on these quality measures for the remainder of the program.
- This is barring a significant change to the structure of the organization.
- DOH recommends that facilities [in consultation with their Performing Provider Systems (PPS)] get to select measures in which it will be assessed.
- The facility´s paired MCO must agree to the measures selected for the Facility Plan.
P4P Recommended Measures
- OQPS has researched measures that would appropriate to implement at the facility level based on:
- Nationally recognized measures (e.g. NQF, NCQA, AHRQ, CMS, CDC)
- Avoidable hospital use measures
- Measures tracking Hospital Acquired Infections
| # | Measure Name | Data Source | Focus Area/Domain |
|---|---|---|---|
| 1 | Acute MI Mortality (IQI #15) | AHRQ | Mortality |
| 2 | Stroke Mortality (IQI #17) | AHRQ | Mortality |
| 3 | Pneumonia Mortality (IQI #20) | AHRQ | Mortality |
| 4 | CAUTI Rate per 10,000 Patient Days (Population Rate) | NHSN | Hospital Acquired Conditions |
| 5 | CLABSI per 10,000 Patient Days (Population Rate) | NHSN | Hospital Acquired Conditions |
| 6 | CDI Healthcare Facility – Onset Incidence Rate per 10,000 Patient Days | NHSN | Hospital Acquired Conditions |
| 7 | Falls with Injury | National Quality Forum | Hospital Acquired Conditions |
| 8 | 3–Hour Sepsis Bundle* | NYSDOH | Hospital Acquired Conditions |
| 9 | VTE–1 Venous Thromboembolism Prophylaxis | Joint Commission | Hospital Acquired Conditions |
| 10 | Prevalence Rate of Facility – Acquired Pressure Ulcers of Stage 2 or Higher per 100 Patients | National Quality Forum | Hospital Acquired Conditions |
| 11 | Episiotomy Rate | Christiana Care Health System | Maternity |
| 12 | Primary C–Section (IQI #33) | AHRQ | Maternity |
| 13 | Avoidable ED Use | 3M* | Utilization |
| 14 | Avoidable Admissions | 3M* | Utilization |
*See guidance document for potential concerns for selecting these measures.
Acronyms: NQF: National Quality Forum; NCQA: National Committee for Quality Assurance; AHRQ: Agency for Healthcare Research and Quality; CMS: Centers for Medicare & Medicaid Services; CDC: Centers for Disease Control and Prevention; OQPS: Office of Quality and Patient Safety
P4P Measure Alternatives
- DOH recommends that facilities have the option to choose a maximum of two (2) alternate quality measures.
- The MCO must agree to an approach to using alternate measures.
- Recommended criteria for alternate measure selection:
- Other nationally recognized measures not included in the measure menu on the previous slide.
- Measures similar to nationally recognized measures that are currently in use at the facility as part of quality improvement efforts.
- For example, this may include measures with facility– defined specifications related to length of stay or hospital acquired infections.
- If an alternate measure is chosen, the facility must document:
- The reasons for selecting alternate measure(s); and
- How data related to the measures will be collected and reported to the paired MCO.
P4P Measure Selection Considerations
- When selecting measures, facilities and PPS should consider the following:
- Measure must have true opportunity for improvement.
- If the facility is already performing well in the area, it may be harder to demonstrate continuous improvement in later periods.
- Measure should align with the goals of the DSRIP project plan of the PPS.
- Measures should relate to initiatives described in the Facility´s Transformation Plan submitted to the HEAPA.
- Measures should impact a significant population receiving care at the facility.
- Facilities should choose measures with denominators that consistently impact more than 30 patients per year.
- Measure must have true opportunity for improvement.
Acronym: HEAPA: Department of Health Division of Health Economics and Provider Assistance; PPS: DSRIP: Delivery System Reform Incentive Payment
P4P Measure Selection Partnership
- Facilities and paired PPS are expected to collaboratively select the six (6) P4P quality measures.
- A facility´s selected measures should align to the PPS´ DSRIP goals.
- The paired PPS should provide non–financial support and guidance to the facility.
- Both parties should benefit from the collaboration.
| PPS Benefits | Facility Benefits |
|---|---|
|
|
Visual of P4P Measure Selection Process
- The figure below shows the proposed measure selection process.

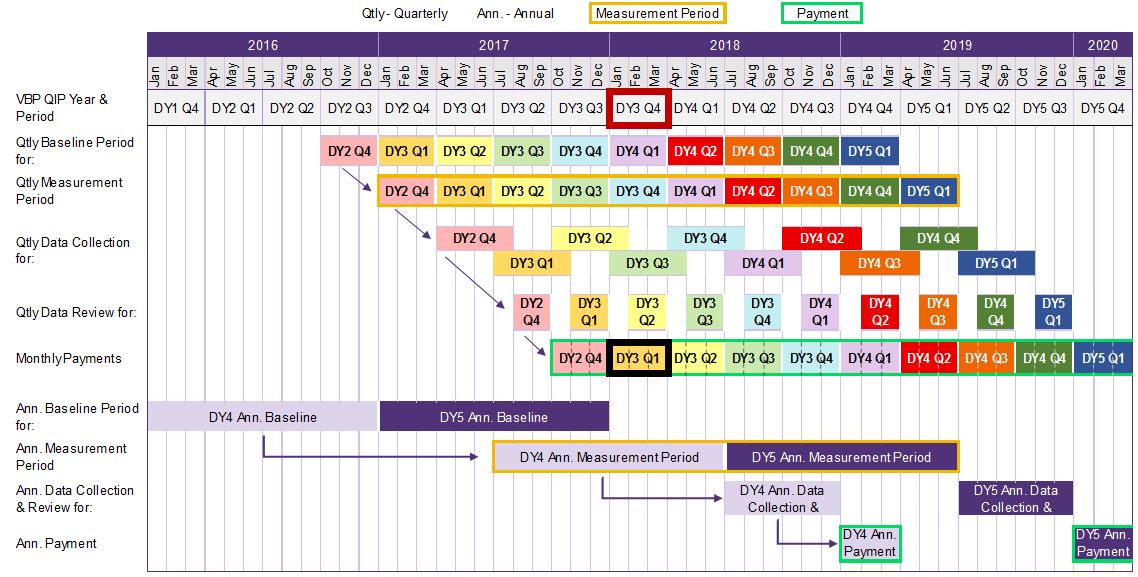
P4P Recommended Reporting/Evaluation Timeline
180 days from quarterly measurement period end to MCO notification of decision
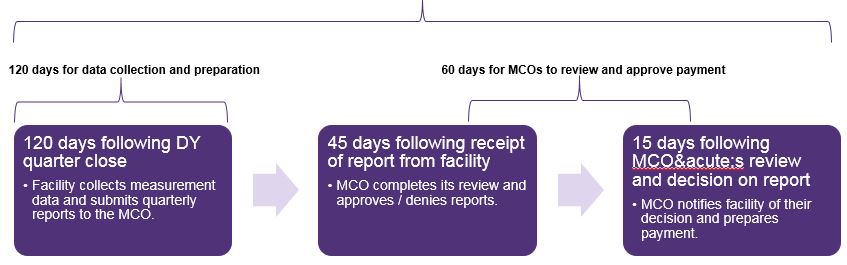
P4P Measure Reporting
- Facilities must report P4P measures four (4) times a year following the close of each DY quarter.
- DOH recommends facilities have 120 days after DY quarter end to collect data and report to the MCO.
- Quarterly reports with attestations should be signed by a senior leader within the facility and provided to the MCO.
- P4P results will be provided using a "rolling annual" calculation.
- A "rolling annual" process is being utilized to minimize the impact of unusual variations for a quarter and minimize issues related to low denominators.
- Additionally, it is recommended for each measure the facility includes the measure collection specifications in their Facility Plan.
- At a minimum, this should describe how the facility pulls, aggregates, and reports measurement information.
P4P Measure Evaluation
- Facilities and paired MCOs are required to:
- Agree to a methodology for reporting Quarterly Improvement Targets (QITs) and Annual Improvement Targets (AITs).
- Agree to a methodology for calculating, reviewing, and approving the results for each measure in each reporting period.
- The MCO is the final authority for whether or not a measure has been met.
- DOH recommends a 180 day collection and reporting window.
- Facilities may have 120 days to collect data and submit report to the paired MCO.
- MCOs may have 60 days following initial receipt for evaluation and payment approval.
- This could include reviewing quarterly reports and determining decisions on measure achievement within 45 days of initial receipt and preparing payment and communicating the decision 15 days to the facility thereafter.
P4P Measure Quarterly Improvement Target (QIT)
- P4P measures will be assessed quarterly.
- The most recently completed quarter´s rolling annual results will be compared to the immediately preceding DY quarter´s rolling annual results for each measure.
- Quarterly improvement will be considered achieved for a given measure if the most recently completed quarter´s rolling annual results indicate maintaining or improving the level of quality over the preceding quarter´s annual rolling results.
- Quarterly award amounts will start flowing P4P in DY3 Q3.
- This gives facilities more time to get reporting systems up to speed.
- However, note that the DY3 Q3 payment is tied to only reporting baselines to the MCO in DY2 Q4.
- Hence, actual performance will drive payment starting in DY3 Q4.
P4P Measure Quarterly Payments
- A facility would receive 100% of its quarterly P4P award if at least four (4) of its six (6) measures are maintained or improved compared to the preceding quarter´s rolling annual results.
- P4P award amounts for a quarter will be reduced by 25% for each P4P measure that is not achieved below four (4) measures.
-
Measures Achieved 4+ 3 2 1 0 Percentage of Quarterly P4P Awarded Earned 100% 75% 50% 25% 0%
-
- Although performance is measured on a quarterly basis, VBP QIP payments are still expected to be paid on a monthly basis.
P4P Quarterly Example
Let´s look at the DY3 Q4 payment date as an example.
As you can see, payments made in DY3 Q4 are based on payments earned for DY3 Q1 performance achievement.
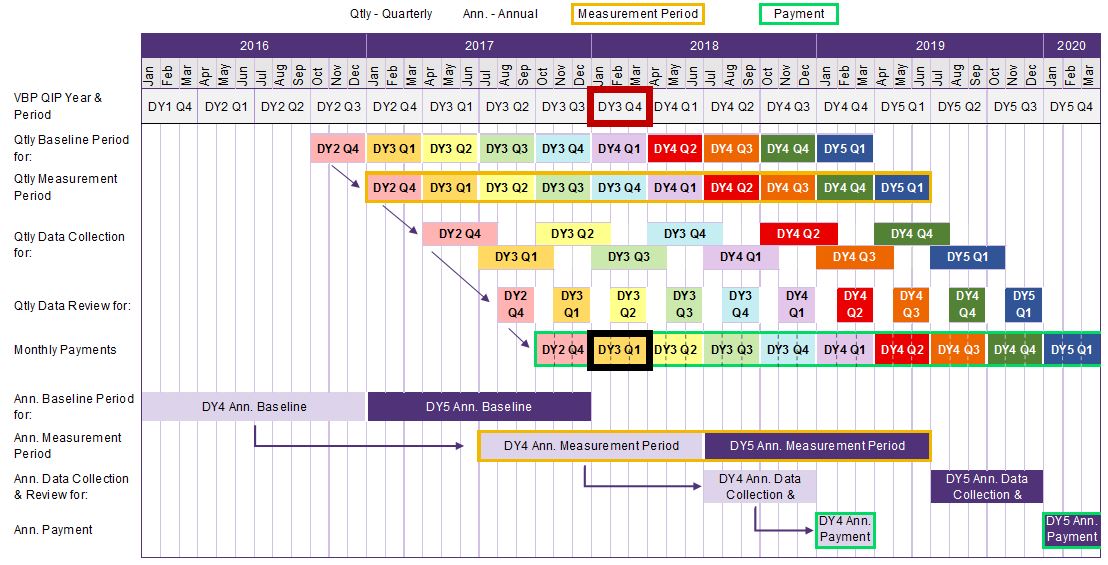
The measurement period for DY3 Q1 is based on "rolling annual results." Therefore, the period includes the three (3) months in DY3 Q1 (Apr – Jun 2017) + the nine (9) preceding months.
Hence, the "rolling annual results" for DY3 Q1 should encompass July 2016 – June 2017.
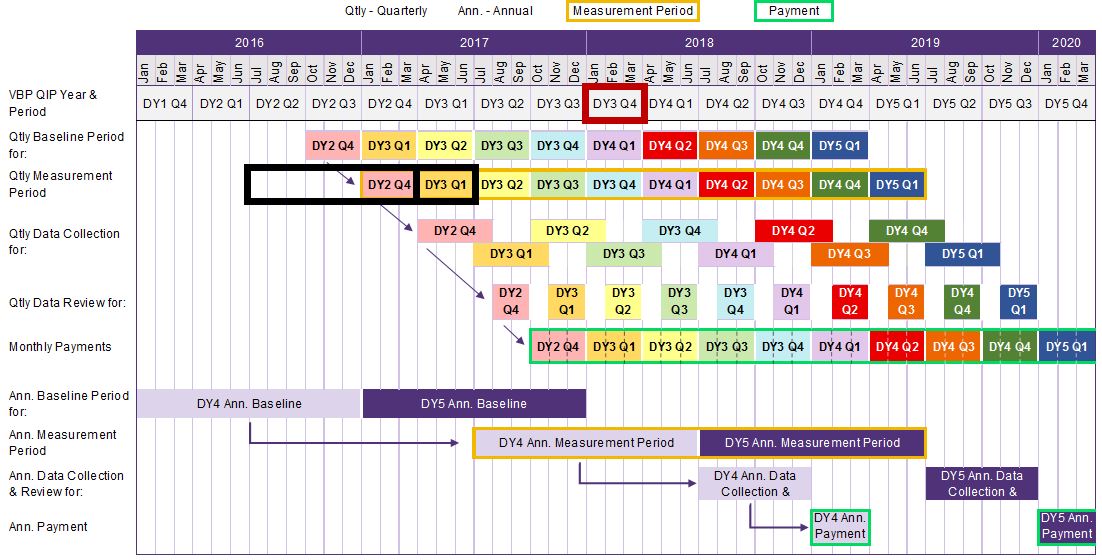
The rolling annual results for DY3 Q1 will be measured against the immediately preceding DY quarter´s rolling annual results.
Therefore, DY3 Q1 will be compared against the prior quarter (DY2 Q4) + nine preceding months (or Apr – Mar 2017)
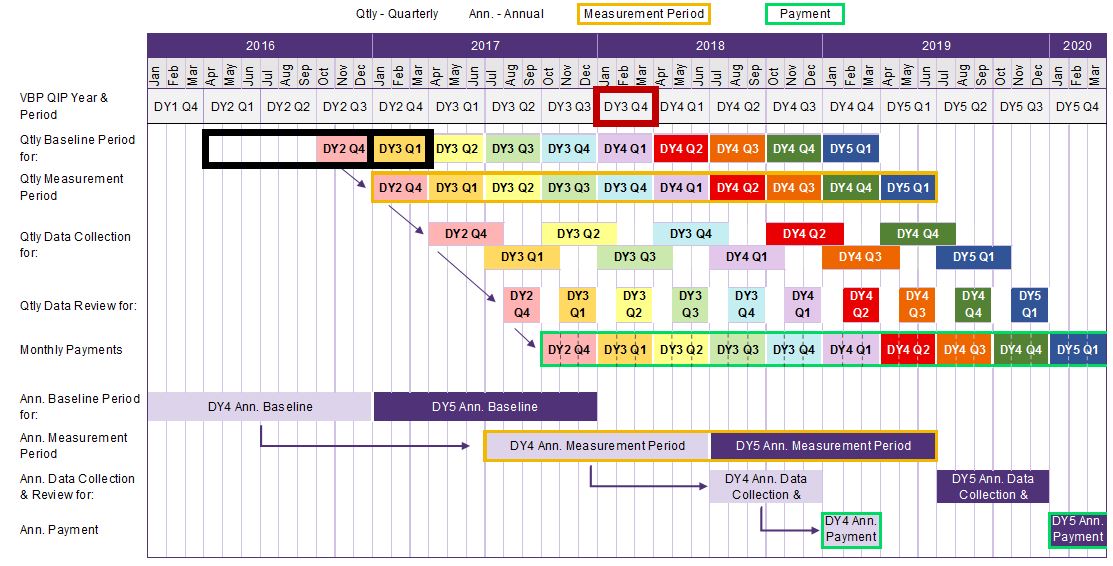
DOH proposes the facility has 120 days to collect and report measure data to their paired MCO.
In this example, the facility has until Oct 31, 2017 to submit the DY3 Q1 measurement report to their paired MCO.
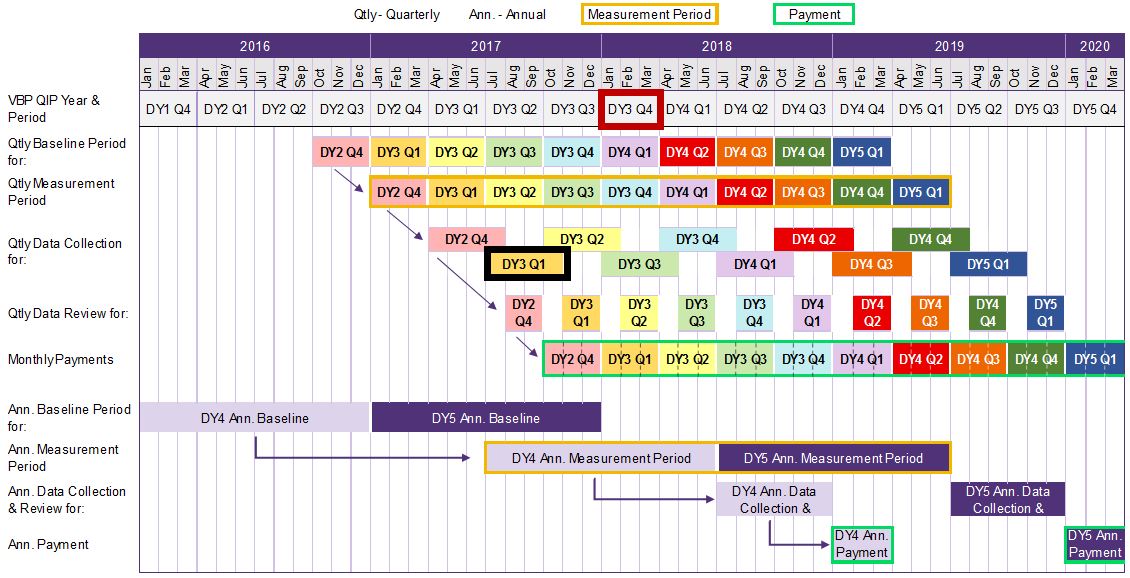
DOH proposes for MCOs to complete their review and approve reports no later than 45 days after initial report submission. This leaves 15 days for MCOs to prepare payment.
In this example, MCO should review reports by December 15, 2017 and prepare payment by December 31, 2017.

Although performance is measured on a quarterly basis, payments should be paid monthly.
In this example, if DY3 Q1 required measurement was achieved, the MCO would pay the facility three payments – Jan, Feb, and Mar 2018.
P4P Measure Annual Improvement Target (AIT)
- At the end of DY4 and DY5, a facility may earn back its unearned P4P award dollars through the achievement of the AIT for that DY.
- If a facility meets four (4) of their (6) AITs, the facility is entitled to the full potential P4P award at the end of the year.
- If a facility fails to meet four (4) of the (6) AITs, the potential annual award will be reduced by 25% for each measure missed below four (4) measures.
Measures Achieved 4+ 3 2 1 0 Percentage of Quarterly P4P Awarded Earned 100% 75% 50% 25% 0%
- Note that unearned P4R funds cannot be earned back by achieving AITs.
DOH is working with hospital and plan association representatives to develop reasonable guidelines for paired facilities and MCOs to utilize in setting AIT targets and expects to release these guidelines by the end of February 2017.
P4P Annual Example
In DY4 and DY5, facilities have an opportunity to earn P4P dollars that may have gone unawarded in quarterly performance periods.
In this example, if the facility meets its AIT for DY4, it will be paid monthly payments for the DY4 funds previously unearned.
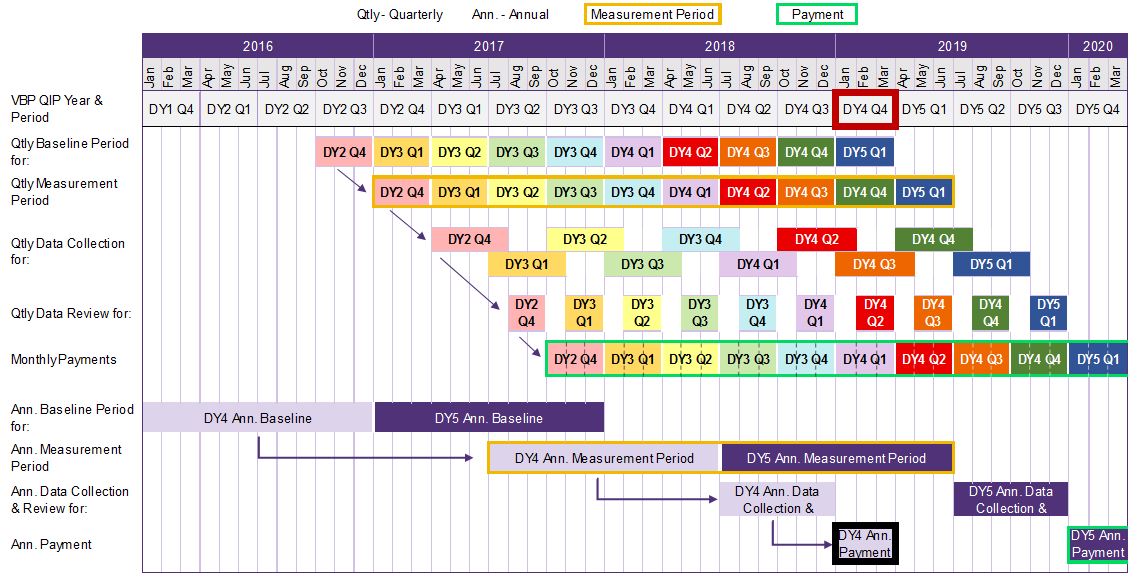
The DY4 AIT baseline period is six months before the start of the AIT measurement period, allowing facilities and MCOs to establish AIT baseline data for the AIT measurement period.
The DY4 annual measurement period is six months before the annual payment date to give the facility time to collect and report data.
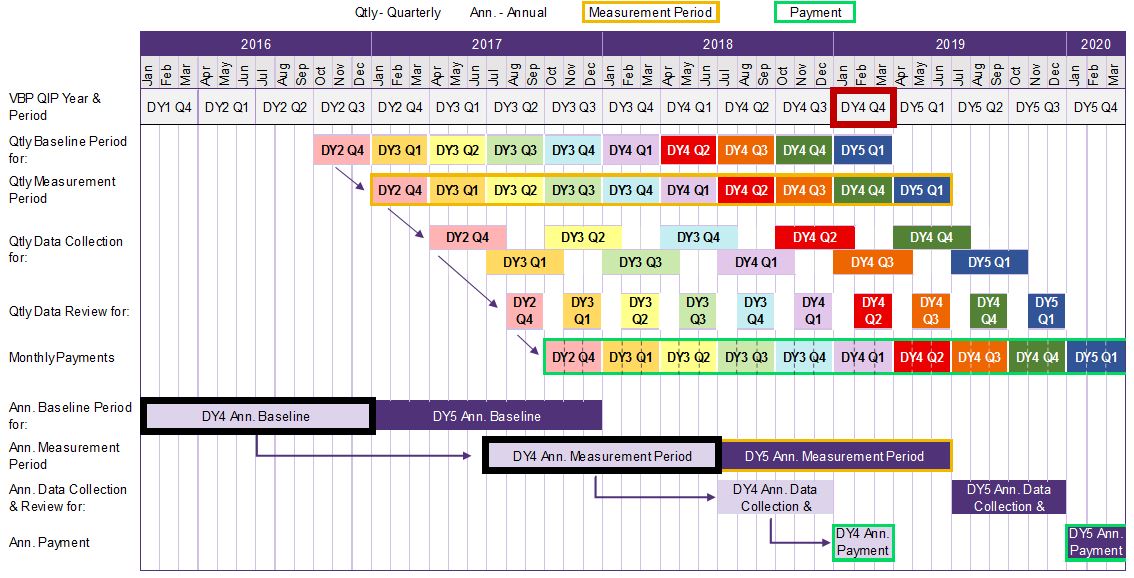
DOH proposes 180 days for data collection, reporting, and payment preparation.
In this example, the facility has 120 days (or by September 30, 2018) to collect and report measure data to their paired MCO.
In this example, MCO should review reports by December 15, 2017 and prepare payment by December 31, 2017.
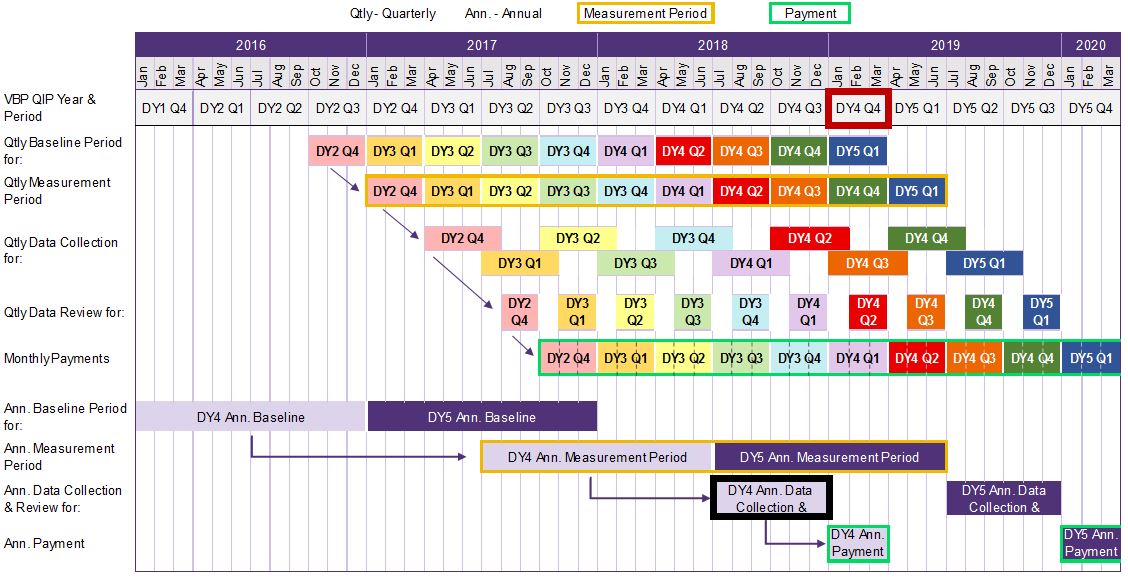
If the AIT in DY4 is considered achieved, the MCO should pay the facility monthly installments of the previously unearned DY4 funds in Jan, Feb, and Mar 2019.

P4R – VBP Contracting
P4R Requirements for DY3 Q1
- P4R milestones drive 100% of payments*** in DY3 Q1 by meeting the milestones listed below.
- In order to receive the full DY3 Q1 payment, a VBP QIP facility must provide their VBP QIP paired MCO with following by April 1, 2017:
Letter of Intent (LOI) documenting that it will enter into a qualified VBP contract with one Medicaid MCO by July 1, 2017*; and + List of MCOs that the facility intends to initiate VBP contracts with by April 1, 2018 and provide documentation that those MCOs have been notified of this intention.**
- In order to receive the full DY3 Q1 payment, a VBP QIP facility must provide their VBP QIP paired MCO with following by April 1, 2017:
*MCO can be different than the paired MCO.
**When taken in aggregate, this list of MCOs should allow the facility to meet the goal of having 80% Medicaid Managed Care funds for the facility contain a VBP component.
***Partial payment may be awarded if at least one of the two requirements is met.
P4R Requirements for DY3 Q2
- P4R milestones also drive 100% of payments* in DY3 Q2 by meeting the milestones listed below.
- In order to receive the full DY3 Q2 payment, a VBP QIP facility must meet the following requirements* by July 1, 2017:
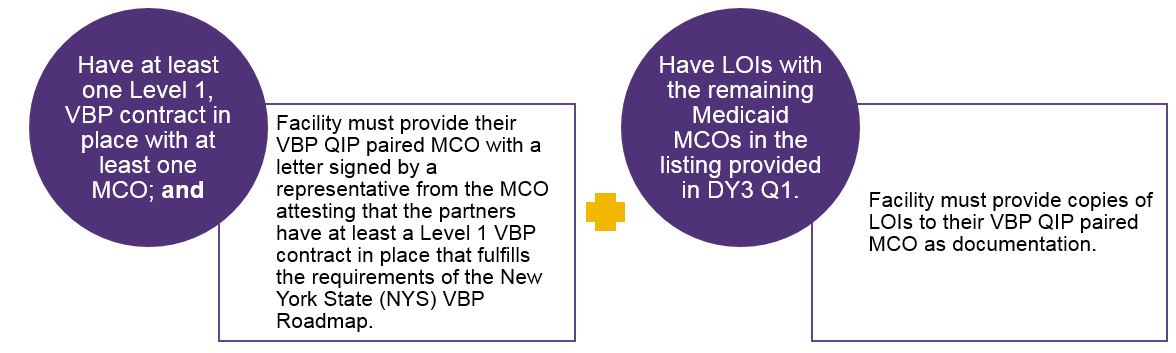
*Partial payment may be awarded if at least one of the two requirements is met.
P4R Requirements in DY4 and DY5
- In order to receive DY4 payments, a VBP QIP facility must have Medicaid MCO contracts where at least 80% of total Medicaid MCO contracted payments to the facility are tied to Level 1 VBP components by April 1, 2018.
- Facility must provide to their VBP QIP paired MCO a letter signed by a representative from each MCO attesting that the partners have at least a Level 1 VBP contract in place that fulfills the requirements of the NYS VBP Roadmap.
- In DY4, facilities can earn P4R payments in all quarters by having and maintaining qualifying Level 1 VBP contract and working towards higher levels of VBP.
- In DY5, the facility must comply with the DY4 P4R requirement, or it is at risk for a 50% reduction in DY5´s P4P payment amount.
P4R Roles
| PPS Role | MCO Role |
|---|---|
|
|
Note that although PPS and MCOs play an important role in VBP contracting for VBP QIP, it is ultimately the facility´s responsibility to enter into Level 1 VBP contracts per program requirements.
Penalties and Measure Credits
P4R Penalties
- For facilities that do not meet the specified VBP contracting expectations (P4R), DOH advises partners abide by the following penalties:
VBP Contract By DY3 (April 1) By DY3 (July 1) By DY4 (April 1) By DY5 (April 1) No LOI with at least 1 MCO Penalty – – – No list of Intended VBP contracting MCOs w/ documentation Penalty – – – No Level 1 VBP Contract with at least 1 MCO – Penalty – – No LOIs with Remaining VBP Contracting MCOs – Penalty – – VBP arrangements are not present in components that drive at least 80% of dollars for the facility´s Medicaid MCO contracts – – Penalty Penalty DY Payment Date Penalty 3 DY3 Q1 Penalty if not met:
25%–50% of P4R Funds in DY3
(50%–100% DY3 Q1 Payment)DY3 Q2 Penalty if not met:
25%–50% of P4R Funds in DY3
(50%–100% DY3 Q2 Payment)4 DY4 Value Lost if Not Met:
100% of P4R Funds in DY45 DY5 50% of P4P Funds in DY5
- In case of issues, facilities should document their contracting progress.
Unearned P4R funds due to penalties for not meeting VBP contracting deliverables cannot be made–up through performance on the facility´s AIT.
P4R Measure Credits
- Facilities that meet certain VBP milestones earlier will be granted a measure credit.
- Measure credits can be used by a facility to help meet their performance targets for VBP QIP P4P quality measures.
- A measure credit will be applied to both the calculation of VBP QIP quarterly and annual measurement achievement by adding an additional measure to the numerator of the calculation.
- For example, if a facility applies for measure credit at the beginning of the year, the measure credit would be applied to all four (4) quarterly performance assessments and the annual assessment.
- In DY3, DY4, and DY5, measure credit may be earned if the facility is part of at least one (1) Level 2 or higher qualified VBP contract.
VBP Contract By DY3 By DY4 By DY5 Level 2 or Higher qualified VBP Contract Measure Credit Measure Credit Measure Credit
VBP QIP Facility Plan – Next Steps
- DOH highly recommends that partners review the guidance document and consider making updates to their Facility Plans based on the provided recommendations.
- DOH scheduled meetings for next week with each MCO and their paired PPS and facilities to discuss the document.
- Revised Facility Plans are due back to DOH by Wednesday, March 15th, 2017.
- Documents are to be submitted to the VBP QIP inbox (vbp_qip@health.ny.gov).
- If you have NOT received the Facility Plan Guidance Document, please e–mail the VBP QIP inbox (vbp_qip@health.ny.gov) and DOH will send it to you as soon as possible.
DY3 Timeline and Q&A
VBP QIP DY3 Timeline
| Milestone | Due Date |
|---|---|
| DOH distributes the Facility Plan Guidance Packet to VBP QIP partners | Jan 27, 2017 |
| DOH hosts Facility Plan Discussions with MCO/PPS/Facility Partnerships | Jan 30 – Feb 3, 2017 |
| Monthly VBP QIP Update Webinar | Feb 15, 2017 |
| DOH reviews VBP QIP MCO Governance Document and distributes Scorecard to MCOs (Group 2) | Feb 17, 2017 |
| VBP QIP DY3 Guidance Released | Mar 10, 2017 |
| Facilities submit their updated, MCO approved, Facility Plan to DOH | Mar 15, 2017 |
| MCOs submit a revised VBP QIP Governance Document to DOH for review (Group 2) | Mar 24, 2017 |
| Facilities must provide paired MCO with LOI to sign Level 1 VBP contracts with one MCO | Apr 1, 2017 |
| Facilities must provide paired MCO with list of Medicaid MCOs which the facility expects to enter into VBP contracts with by April 1, 2018 | Apr 1, 2017 |
| Facilities must have at least one Level 1 VBP contract signed | Jul 1, 2017 |
| Facilities must provide paired MCO with outstanding LOIs for Medicaid MCOs to contract | Jul 1, 2017 |
| Facilities must have Medicaid MCO contracts where at least 80% of total Medicaid MCO contracted payments to the facility are tied to Level 1 VBP components. | Apr 1, 2018 |
Important Information
| VBP Support Materials |
VBP Resource Library:
|
Thank you for your continued support with VBP QIP!
- The next VBP QIP Update Webinar is scheduled for Wednesday, February 15th from 2:00 pm – 3:00 pm.
- Please let DOH of any topics that you would like discussed during next month´s webinar by submitting your requested topics to the VBP QIP inbox (vbp_qip@health.ny.gov).
For any further questions, please contact the VBP QIP inbox: vbp_qip@health.ny.gov
|top of section| |top of page|
Follow Us