Project Implementation Plan Guidance and Reporting Requirements
- Presentation is also available in Portable Document Format (PDF)
Content requirements and expectation for the July 31 PPS Quarterly Report submission & Overall First Impressions of Organizational Implementation Plans.
July 14, 2015
Quarterly Report/Project Implementation Plans:
General Instructions
- The revised Domain 1 and Project Implementation Plans (IPs) serve as the first Quarterly Report.
- PPS will be required to submit revised Domain 1 Implementation Plans, inclusive of all organizational and project 2.a.i sections, and Implementation Plans for all PPS selected projects into MAPP.
- Revised Domain 1 and new Project Implementation Plans should address IA review and comments.
- Implementation Plan work steps, referred to as tasks in MAPP, should provide a solid framework of all the activities the PPS must accomplish to successfully achieve each milestone.
- If the PPS has previously completed work steps that materially impact the IA’s understanding of how the submitted work steps accurately reflect what needs to be accomplished, the Implementation Plan should reflect progress made to date.
- For example: workforce strategy milestone "Perform detailed gap analysis between current state assessment of workforce and projected future state," if the PPS has already completed the gap analysis please identify this progress in your IP. As a result the 1st work step may be different than a PPS who is not as far along.
- All speed and scale commitments in your Implementation Plans must match the Project Plan Application commitments submitted in January.
IA Summary Comments of Submitted Implementation Plans
- PPS will not be required to demonstrate milestone completion until the defined benchmark date OR speed and scale commitments. PPS should consider defined benchmark dates when determining implementation timelines and ensure activities are scheduled and staged appropriately.
- Implementation Plans should not reiterate the milestone’s goals, but rather clearly identify the specific work steps the PPS will take to complete the milestone.
- Roles and Responsibilities should include names of people who will be responsible for an activity and specifically what their role will be. Several Implementation Plans included many TBDs in this sections; positions, if unfilled, could present a risk to the project completion.
- Stakeholder Engagement Sections should:
- Identify PPS collaboration in overlapping regions/projects
- Include the specific organization and individual names as well as state agencies such as developmental disabilities, behavioral health, substance abuse and Local Government Units (LGUs), etc.
- Progress Reporting responses should include more details regarding how the activities supporting the milestone will be tracked and the process by which adjustments of work steps will be made depending on initial results.
IA Considerations When Reviewing Implementation Plans
General Reviewer guidelines – the following were into consideration:
- Does the implementation plan adequately address each appropriate step in the planning, development, and completion of the Milestone?
- Do the work steps have appropriate timelines associated with them and consistent with any prescribed completion dates?
- Does the implementation plan include steps to determine the success of the plan at regular intervals and change course if it is not working?
- Does this description demonstrate the PPS’ plan to successful completion of the requirement?
Example: Workforce Strategy Section*
MILESTONE: Perform detailed gap analysis between current state assessment of workforce and projected future state
| 1. Perform detailed workforce analysis which will identify transferrable skills between jobs to be reduced vs. jobs needed; current positions that will require re–deployment and/or training; and available skill sets currently available within PPS via work force surveys, workforce workgroup, and online tools such as Health Workforce New York. | DY1, Q2 |
| 2. Confirm staff eligible for re–deployment given project selection and DSRIP goals, and review existing HR policies and labor agreements. | DY1, Q3 |
| 3. Identify non–traditional methods for recruiting necessary staff to fill workforce gaps (ex: telemedicine; sub–contracting with community–based partners or joint employment possibilities with current/future employers). | DY1, Q3 |
| 4. Identify those "hard–to–fill" positions that cannot be filled through re–deployment or non–traditional methods. | DY1, Q3 |
| 5. Create, implement, and advertise DSRIP job board and identify other job sites for posting | DY1, Q3 |
| 6. Create recruitment plan and timeline for new hires. | DY1, Q3 |
| 7. Implement strategy to fill for those positions that are difficult to recruit, train, or retain. | DY1, Q3 |
| 8. Complete workforce budget analysis to establish revised workforce budget for the duration of DSRIP. | DY2, Q2 |
| 9. Finalize current state assessment and obtain PPS governance approval. | DY2, Q3 |
* This section will become available in the DY1 Q2 report and finalized by PPS within the DY1 Q3 submission.
Example: Governance Section
MILESTONE: Establish a clinical governance structure, including clinical quality committees for each DSRIP project
| 1. Develop and finalize charter for Clinical Governance Committee. The charter will describe the responsibilities of the Subcommittee, the process for appointing members to the specific Project Operations Subcommittees, and decision–making process of the Committee/Subcommittee and reporting structure. | DY1, Q2 |
| 2. Solicit and appoint members of the Clinical Governance Committee. | DY1, Q2 |
| 3. Seek PPS Executive Committee and Steering Committee approval of the charter. | DY1, Q2 |
| 4. Appoint PPS Chief of Clinical Program Implementation. | |
| 5. Devise communication plan to ensure all providers and partners understand the Clinical Governance Committee will provide clinical governance and quality oversight for all DSRIP projects in conjunction with the PPS Medical Director and PPS Chief of Clinical Program Implementation. | DY1, Q2 |
| 6. Convene Project Operations Subcommittees, review charter, and initiate subcommittee work. | DY1, Q3 |
| 7. Establish work groups by project or project groups – as determined by Subcommittee to support development of detailed clinical guidelines, operations and provider engagement. | DY1, Q4 |
| 8. Develop and finalize initial clinical guidelines for each project. Project Operations Subcommittees and Clinical Governance Committee will approve clinical guidelines. | DY1, Q4 |
| 9. Establish process and schedule to review and revise/update clinical guidelines on an as needed basis. | DY1, Q4 |
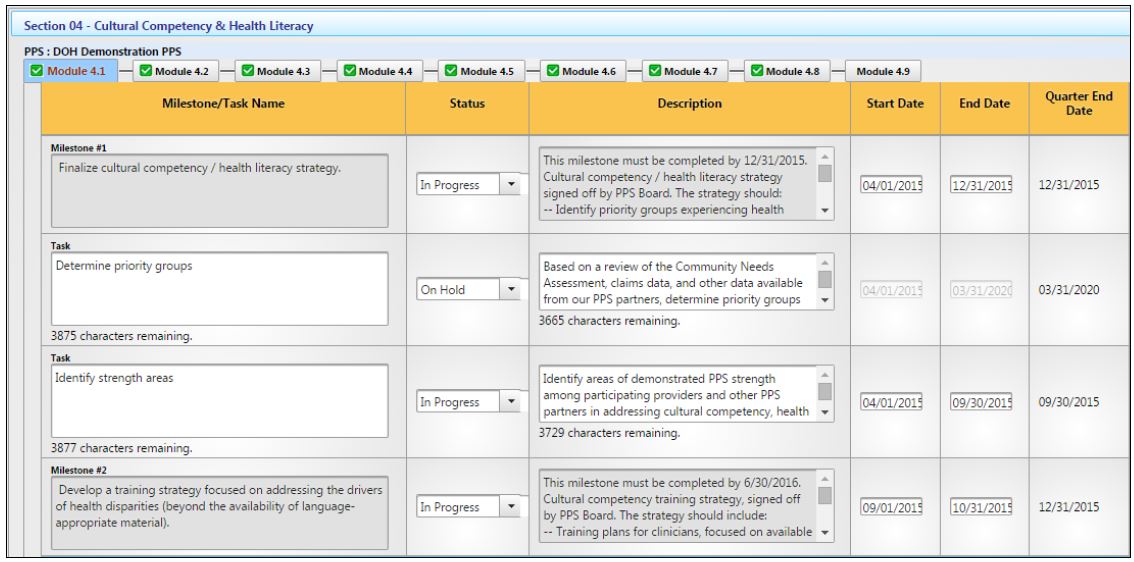
Example: Cultural Competency and Health Literacy Section
MILESTONE: Finalize cultural competency / health literacy strategy.
| 1. Based on a review of the Community Needs Assessment, claims data, and other data available from our PPS partners, determine priority groups experiencing health disparities and needs for cultural competency and health literacy strategy. | DY1,Q2 |
| 2. Identify areas of demonstrated PPS strength among participating providers and other PPS partners in addressing cultural competency, health literacy and health disparities | DY1, Q2 |
| 3. Develop a cultural competency and health literacy strategy document, which includes the following minimum components and takes into consideration unique attributes PPS attributed patients and identifies key factors to improve access to quality primary, behavioral health, and preventive care | DY1, Q3 |
| 4. Devise cultural competent assessments and tools to assist patients with self–management aligned with PPS clinical planning around patient self–management | DY1, Q4 |
| 5. Define plans for two–way communication with the population and community groups through specific community forums | DY1, Q4 |
| 6. Collect community–based interventions ("best–practice") to reduce health disparities and improve outcomes. | DY2, Q2 |
| 7. Present strategy document to PPS Subcommittee and Stakeholder Engagement Subcommittees. | DY1, Q3 |
| 8. Strategy document reviewed and approved by Executive Committee. | DY1, Q3 |
Example: Population Health Management Section
MILESTONE: Finalize PPS–wide bed reduction plan.
| 1. Identify relevant data on opportunities to reduce avoidable inpatient hospitalization rates for the PPS overall and for the hubs, including individual hospitals within each hub. | DY2, Q1 |
| 2. Identify most significant clinical conditions by geographic area and specific hospital where a reduction in beds is possible (review rates of inpatient stays associated with avoidable hospital admissions). | DY2, Q1 |
| 3. Review DSRIP project interventions and estimate potential impact on potential bed reduction based Step 2. | DY2, Q2 |
| 4. Identify workforce impact and training needs where potential exists to reduce beds based on data on both avoidable hospital admission and DSRIP project impact. | DY2, Q2 |
| 5. Develop training plans based on workforce needs to reduce beds and shift care to outpatient settings, based on data on avoidable hospital admissions (Step 2) and DSRIP project impact. | DY2, Q3 |
| 6. Document bed reduction plan for review by the PPS Executive Committee based on data on avoidable hospitalizations, DSRIP project impact and other key factors. | DY2, Q4 |
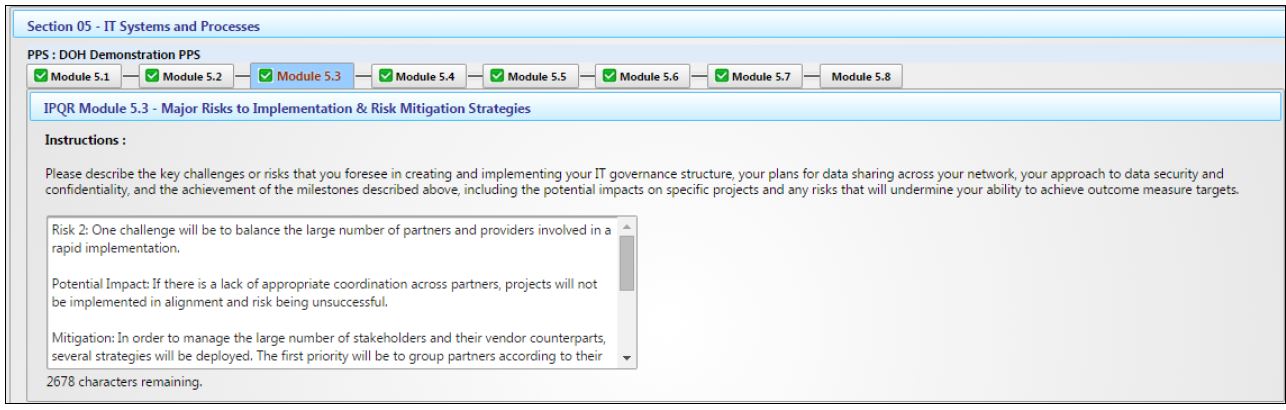
Example: IT Systems and Processes Section
SECTION: Major Risks to Implementation & Risk Mitigation Strategies.
General Reviewer guidelines – the following was taken into consideration:
Does the implementation plan describe the key challenges or risks in implementing the governance structure and processes in achieving the milestones?
Risk 2: One challenge will be to balance the large number of partners and providers involved in a rapid implementation.
Potential Impact: If there is a lack of appropriate coordination across partners, projects will not be implemented in alignment and risk being unsuccessful.
Mitigation: In order to manage the large number of stakeholders and their vendor counterparts, several strategies will be deployed. The first priority will be to group partners according to their "HIT readiness" via the current state assessment and gap analysis. PPS will address these cohorts collectively to provide the most relevant feedback based on a partner´s current status. PPS will also leverage the experience of the most advanced partners to share " lessons learned" and provide "peer–to–peer" support to those partners that are late adopters of IT.
This approach will enable a top–down and bottom–up strategy allowing for immediate benefits to all partners. PPS will support providers and partners with vendor engagement support to ensure: 1) vendor timelines and capabilities are in–line with the DSRIP goals and 2) that the collective influence of the partners is used as leverage to ensure timely alignment of IT adoption.
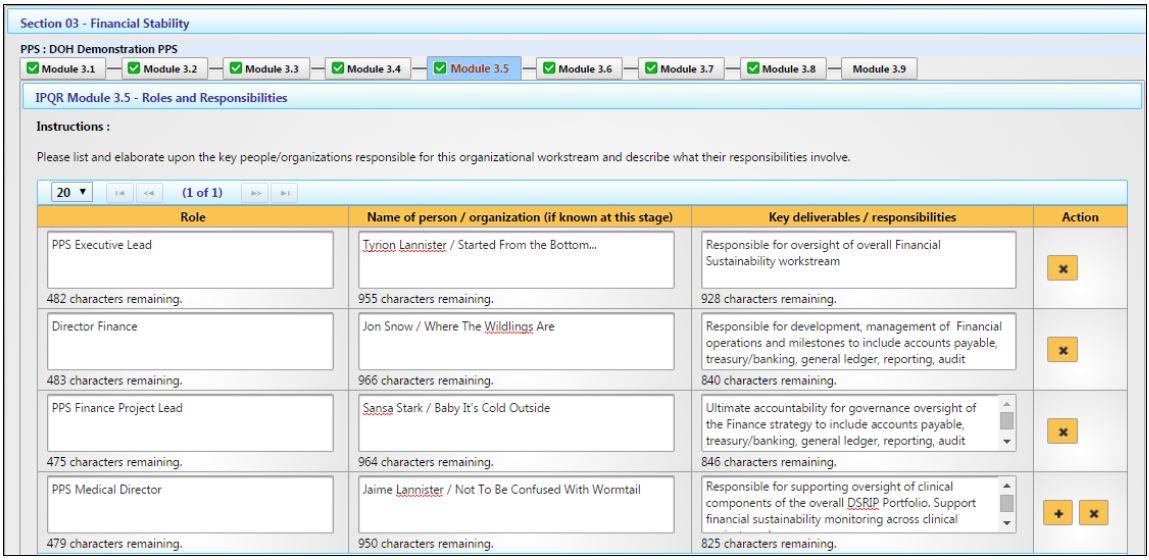
Example: Financial Sustainability Section
SECTION: Roles and Responsibilities
The ´Roles & Responsibilities´ table is intended to capture those individuals responsible for driving/managing the work stream
| Role | Name of person / organization | Key deliverables / responsibilities |
|---|---|---|
| PPS Executive Lead | Tyrion Lannister | Responsible for oversight of overall Financial Sustainability Work stream |
| Director Finance | Jon Snow | Responsible for development, management of Financial operations and milestones to include accounts payable, treasury/banking, general ledger, reporting, audit |
| PPS Finance Project Lead | Sansa Stark | Ultimate accountability for governance oversight of the Finance strategy to include accounts payable, treasury/banking, general ledger, reporting, audit |
| PPS Medical Director | Jaime Lannister | Responsible for supporting oversight of clinical components of the of overall DSRIP Portfolio. Support financial sustainability monitoring across clinical projects and programs. |
| Compliance Officer | Joffrey Baratheon | Lead Compliance Program, including chairing Sub–Committee; implementing Work Plan; training; hotline; monitoring; investigations; promoting culture of ethics and compliance with DSRIP requirements. |
| Financial Sustainability Team | Catelyn Stark | Lead development of Financial Sustainability including Budget and Funds Flow milestones |
| MCO Relations Team Lead | Stannis Baratheon | Lead liaison to MCO Partners |
| MCO/Value Based Payment Workgroup | Robb Stark | Will oversee the development and implementation of the VBP Roadmap support the Team Lead in negotiations with MCO partners |
| Director, Project Management Office | Cersei Lannister | Project Management Office will champion consistent project management practices and methodologies, in addition, will support the DSRIP project stakeholders to as a source for project management expertise, support communications, and align requirements within multiple projects. |
| PPS Director, Network Development & Performance | Christopher Robbins | Responsible for the Workforce & Community Engagement milestones as well as the Performance Evaluation, reporting, and Management structure for the PPS |
Example of a Response Requiring More Information
SECTION: Progress Reporting.
The financial sustainability work stream will be considered successful based on the demonstrated ability to:
- Identify and monitor the PPS partner organizations who are identified as financially fragile during the course of the DSRIP period
- Seamlessly implement and ensure compliance to all financial controls and the PPS compliance requirements
- Establish and execute the PPS´ plans to transition to the targeted volume of Medicaid value–based payment revenues.
Project Requirements: Development and Submission of Work Steps
- The DY1 Q1 Quarterly Report will require a baseline entry of project requirement timelines, PPS–defined sub–steps, and implementation status.
- Reporting will be required for the project requirements and metrics outlined in Domain 1 Project Requirements: Milestones & Metrics.
- For each Project Requirement, the PPS must develop and define sub–steps that:
- Demonstrate progression towards and achievement of project requirements
- Provide the IA with clear understanding of the significant tasks which must be completed along the pathway of successful project requirement completion
- Provide start and end dates (in accordance with project requirement timeframes)
- Provide implementation status of each sub–step (i.e. Complete, In Progress, On Hold)
High–Level Overview of Submitted Implementation Plans: 2.a.i
- Work steps were not clear how the PPS will formally transform their PPS provider network into a high–performing Integrated Delivery System (IDS). Work steps should include how the development of contracts, MOUs or other agreements will be finalized.
- While the PPS includes terms such as "partner" and "leverage" Health Homes (HHs)– it is expected the PPS will provide more detail which HHs they will engage as stakeholders and how this will be accomplished. The IA would like to encourage more steps identifying how the collaborations with HHs will occur.
- Work steps should include how the PPS will develop population health management activities (particularly policies and protocols) as well as how these activities will be conveyed to the project teams and ensure compliance.
- Work steps should include areas of engaging patient stakeholders in achieving milestones.
- Work steps should provide enough information to exhibit how the PPS will accomplish some very challenging milestone. More work steps in terms of how the technical and clinical integration challenges will be overcome are expected.
Project 2.a.i: Milestones and Work Steps
Project Requirement #1: All PPS providers must be included in the Integrated Delivery System. The IDS should include all medical, behavioral, post–acute, long–term care, and community–based service providers within the PPS network; additionally, the IDS structure must include payers and social service organizations, as necessary, to support its strategy.
General Reviewer guidelines – the following are points were taken into consideration:
- Have they considered that different providers (and/or provider types) will need to be considered differently, due to factors such as work already done to date, overall readiness, etc.?
- Are the steps identified specific enough to demonstrate the PPS’ plan to successful completion of the project requirement?
- Is the target completion date attached to each step; a) consistent with the due date prescribed by the IA, b) appear to be reasonable and/or realistic given the step described?
- Will the steps identified within project requirement take requirement to 100% completion?
- Do the steps align to the project requirement’s "metric/deliverable" identified in the Domain 1 Project Requirements Milestones and Metrics?
- Will these steps, if completed, arrive at a successful completion of the project requirement?
| 1. Complete full provider list of all PPS participants, defined by Provider type, with NPI and Practice name | DY1, Q3 |
| 2. Develop list of elements that will need to be part of each provider agreement/contract to develop draft contract | DY1, Q3 |
| 3. Post PPS provider network directory on web site; maintain periodic audit trail report of log of changes to network list | DY1, Q3 |
| 4. Create a process to track all executed Provider contractual agreements | DY1, Q3 |
| 5. Initiate strategy to engage PPS providers and partners in formal participation agreements (MOUs/contracts). In addition to all providers in PPS network, will include payers/MCO and social service organizations, as necessary to support strategy. | DY1, Q4 |
| 6. Finalize all participation agreements (MOUs/contracts). | DY2, Q1 |
| 7.Create a process that tracks provider performance compared to contract terms/requirements, including corrective actions | DY2, Q2 |
| 8. Engage key internal unit level PPS partners to participate in IDS project | DY2, Q2 |
| 9. Plan established to monitor PPS provider performance periodically and report to the PPS governance, with correction action and performance improvement initiatives as needed | DY2, Q3 |
| 10. Collect provider network lists, periodic reports demonstrating changes to the network list and contractual agreements | DY2, Q4 |
| 1. PPS will identify and engage participating providers and will facilitate stakeholder meetings with key representatives to offer further information on their role and need for involvement in the project | DY1, Q3 |
| 2. PPS will execute contracts or participation agreements with partnering providers. | DY1, Q4 |
| 3. PPS will include payers and social service agencies as necessary and appropriate to further IDS implementation strategies. | DY2, Q2 |
IA Comment: Activities described do not provide nearly enough information to exhibit how the PPS will accomplish this very difficult milestone. These three work steps restate the intention of the milestone and not specific enough to demonstrate the PPS' plan to successful completion of the project requirement.
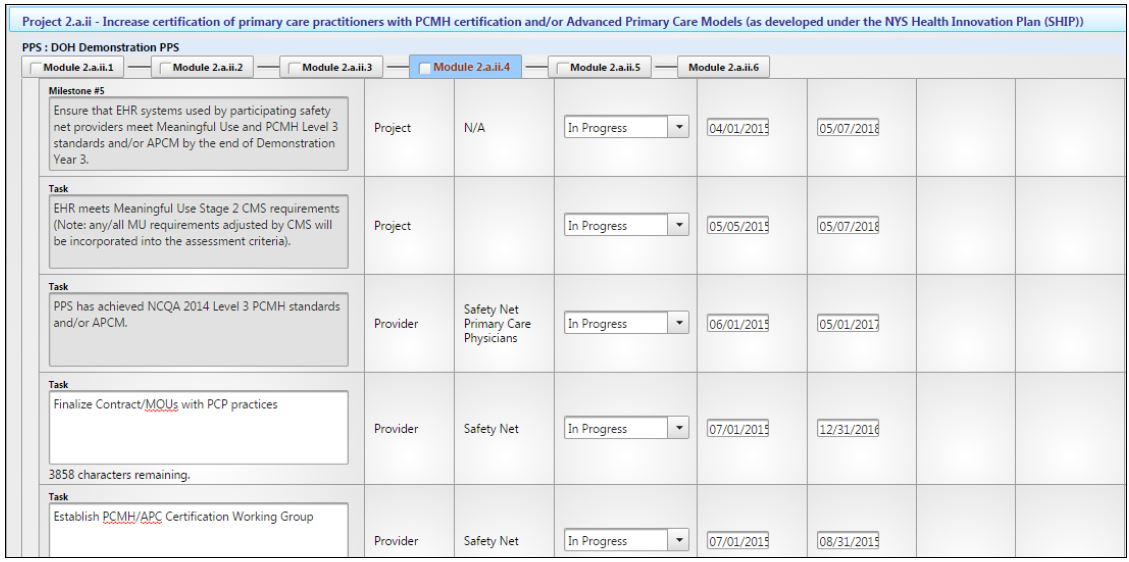
Project 2.a.ii: Milestones and Work Steps Example
Project Requirement #5: Ensure that EHR systems used by participating safety net providers meet Meaningful Use and PCMH Level 3 standards and/or APCM by the end of Demonstration Year 3.
| Target Completion Date | |
|---|---|
| 1: Finalize Contract/MOUs with PCP practices | 12/31/2016 |
| 2: Establish PCMH/APC Certification Working Group | 8/31/2015 |
| 3: Finalize strategy for achieving Level 3 certification or APC | 10/15/2015 |
| 4: Review PCMH 2014 Level 3 Standards and Requirements | 1/25/2016 |
| 5: Complete assessment of PCP practices to be become NCQA Level 3 certified and or APC | 12/16/2015 |
| 6: Complete the NCQA PCMH survey application and APC application requirements | 2/6/2017 |
| 7: PPS PCMH Certification Working Group to finalize PPS wide roadmap for achieving Meaningful Use certification | 12/31/2016 |
| 8: Review PCMH 2014 Level 3 Standards and Requirements | 8/31/2015 |
| 9: Conduct internal assessment of current EHR and other IT systems | 12/16/2015 |
| 10: Identify necessary data sets with individual demographic, health, and status information need to be collected within EHR | 3/31/2016 |
| 11: Finalize renegotiation contract with of existing IT vendor | 2/6/2017 |
| 12: Expand EHR capabilities to collect information, socioeconomic, demographic, and neighborhood characteristics | 3/22/2017 |
| 13: Confirm all participating providers meet Stage 2 Meaningful Use Requirements Certification and PPS has achieved NCQA 2014 Level 3 PCMH standards and/or APCM. | 5/7/2018 |
Project 3.a.i: Milestones and Work Steps Example
Project 3.a.i (Model 1. PCMH Service Site) PROJECT REQUIREMENT #1: Co–locate behavioral health services at primary care practice sites. All participating primary care practices must meet 2014 NCQA All practices meet NCQA 2014 Level 3 PCMH and/or APCM standards by the end of DY3.
| Target Completion Date | |
|---|---|
| 1: Finalize Contract/MOUs with PCP practices | 12/31/2016 |
| 2: Establish PCMH/APC Certification Working Group | 8/31/2015 |
| 3: Complete assessment of PCP practices to be become NCQA Level 3 certified and or APC | 12/16/2015 |
| 4: Finalize strategy for achieving Level 3 certification or APC | 1/25/2016 |
| 5: Establish policies and procedures outlining coordination and hand-offs between BH and PCP | 3/31/2016 |
| 6: Complete the NCQA PCMH survey application and APC application requirements | 2/6/2017 |
| 7: Institute clear workflows for assessment, referrals and follow up care to be provided | 10/15/2016 |
| 8: Train care team on workflows and care coordination processes | 3/22/2017 |
| 9: Project team completes review of care coordination outcomes and timeliness of services | 5/7/2018 |
| 10: PPS RCE team evaluates metrics (# of patients engaged, # connected to BH and receiving care) | 9/30/2018 |
Domain 4 Project Milestones
- In completing the DSRIP Project Plan Application for Domain 4 projects, each PPS defined project implementation milestones that they would work towards in implementing the project.
- Similar to the Domain 2 & 3 projects, the PPS will be expected to develop and define sub–steps that:
- Demonstrate progression towards and achievement of project requirements
- Provide the IA with clear understanding of the significant tasks which must be completed along the pathway of successful project requirement completion
- The PPS will, for the purposes of determining Achievement Values for the implementation of the Domain 4 projects and the payments associated with those Achievement Values, be expected to meet these self–defined milestones.
- Domain 4 projects will require the PPS to self–report in the PPS–Defined module. These work plan activities must align with the milestones committed to in the Project Plan Application.
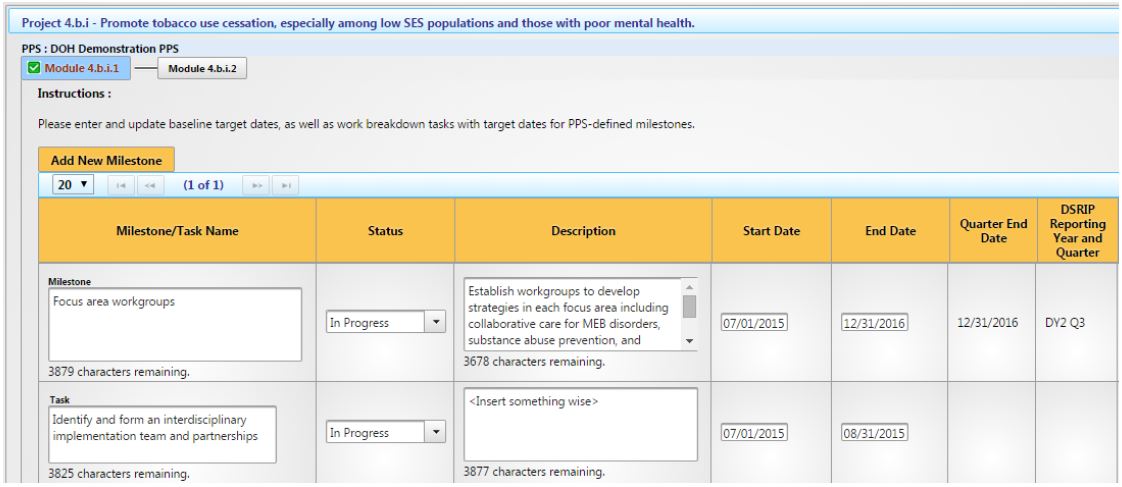
Project 4.a.iii: Milestones and Work Steps Example
4.a.iii Strengthen Mental Health and Substance Abuse Infrastructure across Systems
| Target Completion Date | |
|---|---|
| Milestone 1: Establish workgroups to develop strategies in each focus area including collaborative care for MEB disorders, substance abuse prevention, and training and education related to MEB health promotion, prevention and treatment. | 12/31/2016 |
| 1: Identify and form an interdisciplinary implementation team and partnerships. | 8/31/2015 |
| 2: Develop common agenda, goals and implementation plan. | 8/5/2015 |
| 3: Review existing programs and CBOs to identify gaps & strengths to build on via DSRIP | 10/15/2015 |
| 4: Engage partner agencies and expand efforts with DOH and OMH to implement ´Collaborative Care´ | 12/25/2016 |
| 5: Engage DOH / OMH/ OASAS in discussions to further enhance coordination of care across the system. | 12/16/2015 |
| Milestone 2: Develop mechanism for collection and aggregation of data as project components are implemented. | 2/6/2017 |
| 1: Identify opportunities meet data needs. | 8/31/2015 |
| 2. Identify existing population health management tools within the PPS. | 8/5/2015 |
| 3: Conduct analysis between existing and needed data needs to meet project requirements | 10/15/2015 |
| 4: Develop, as part of the overall l IT approach, strategies to leverage existing capabilities and create new capabilities to meet DSRIP project requirements and meet population needs for this project | 2/6/2017 |
| Target Completion Date | |
|---|---|
| Milestone 3: Provide cultural and linguistic training on MEB health promotion, prevention and treatment. | 12/31/2016 |
| 1: Create training schedule and materials to execute training. The focus of the training will be on strategies to improve effective patient engagement; and the use of data–oriented approaches to identify those likely to suffer from health disparities. | 8/31/2015 |
| 2: Develop training plans for clinicians, CBOs and other workforce segments based on best practice research that addresses the needs of ethnic and racial minority groups served by the PPS who suffer from health disparities. | 12/16/2015 |
| 3: Obtain Cultural Competency Committee sign–off on training plans. | 12/31/2016 |
| 4: Execute trainings for all organizations and individuals identified in Step 1 based on training plans. | 2/6/2016 |
| 5: Evaluate training sessions regarding specific engagement strategies and patient engagement approaches. | 3/22/2016 |
| 6: Review & revise educational materials and outreach initiatives targeting ethnic groups and high impact neighborhoods | 5/7/2016 |
| Milestone 4: Share data and information on MEB health promotion and MEB disorder prevention and treatment. | 12/31/2016 |
| 1: Conduct a complete analysis of PPS organizations to determine training needs on topics such as clinical quality, performance reporting, data for quality improvement, and others as needed | 8/31/2015 |
| 2: Develop training materials that address MEB health promotion and MEB disorder treatment across the PPS. | 7/16/2015 |
| 3: Roll–out training materials based on identified project participants | 10/31/2015 |
| 4: Evaluate re–training needs and frequency of future trainings | 12/31/2016 |
Quarterly Report/Project Implementation Plans:
MAPP Guidance
- In order to better view the peripheral functionality and buttons, it helps to decrease browser magnification.
- DY1 Q1 report aims to baseline all PPS activities over the life of the waiver. These projections are maintained in MAPP for the duration of DSRIP; however, PPS will provide updates to reflect actual activity in each Quarterly Report from DY1 Q2 and forward, with the ability to provide narrative for any substantial variations between baseline and actual data.
- Outside of the Roles and Responsibilities module associated with each Organizational Section, any additional context, including assigning responsibility for individual workplan activities, should be provided in the narrative textbox associated with each milestone.
- Save as Draft functionality is available for the Prescribed Milestone and Project Implementation Speed modules as of after the 07/08/2015 maintenance window. A PDF export of the quarterly report is now also available under the Implementation Plan link located on the Home Page.
- Workplan modules encompass the ability to add milestones and tasks. All PPS activities, including worksteps, sub–steps, sub–tasks, should be reported within the 2–feature hierarchy. Level of detail expected from PPS workplans is explicated in the Domain 1 Project Requirements Reporting Guidance webinar from April 10, 2015.
- Key milestones, and associated tasks, that extend beyond the timeframes of Organizational prescribed milestones should be reported within the PPS–Defined Milestone modules.
- Workplans can be changed in future reports; however, original milestone and task entries cannot be deleted. Edits will need to be accompanied by an explanation in the narrative section.
- When adding new tasks within the Project Prescribed Milestones modules, the reporting unit–level will default to ‘Project’.
- For any provider unit–level project requirements (defined in June 18, 2015 Domain 1 Project Requirements guidance document), cumulative ramp–up should align with respective provider type commitments displayed Project Implementation Speed modules.
- Consistent with the Project Plan Application structure and reasoning, there is no Patient Engagement Speed module for Project 2.a.i and no scale and/or speed modules for Domain 4 projects.
- In completing the DSRIP Project Plan Application for Domain 4 projects, each PPS defined project implementation milestones that they would work towards in implementing the project. For these projects, the PPS–Defined Milestones module should, inter alia, reflect these self–defined milestones.
Implementation Plan Support Documentation
DSRIP Webinars and Presentations
- Implementation Plan Project User Guide
https://commerce.health.state.ny.us/mapp/ntwk/projimpl/orgsec/projImplHome.jsf# - Domain 4 Project Reference Guide
http://www.health.ny.gov/health_care/medicaid/redesign/dsrip/docs/d4guidance_2015–06–08_final.pdf - July 2015 Quarterly Reporting in the Medicaid Analytics & Performance Portal (MAPP)
https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/docs/mapp_quarterly_rpt_slides.pdf
MAPP Technical Assistance
- Contact the CMA Help Desk (518–649–4335, MAPP–CustomerCareCenter@cma.com)
Follow Us