Managed Care Data Sharing Collaborative
MILLENNIUM COLLABORATIVE CARE ("MCC")
- Presentation is also available in Portable Document Format (PDF)
NYS ALL PPS WEBINAR – 12/8/2017
Vital Statistics: 260,000 Medicaid Recipients Attributed to Millennium
- 3.4% of New York State Medicaid Recipients are attributed to Millennium
- 26% of WNY residents are Medicaid recipients 52% of Medicaid recipients in WNY are attributed to Millennium
- 14% of the entire population of WNY is attributed to Millennium
The Millennium Mission
We are a Population Health Services Organization for our partners within the MCC network.
Beyond the services we provide, our true purpose and passion is improving health care quality, access & outcomes through a best–in–class physician–driven & analytics enabled transformation.
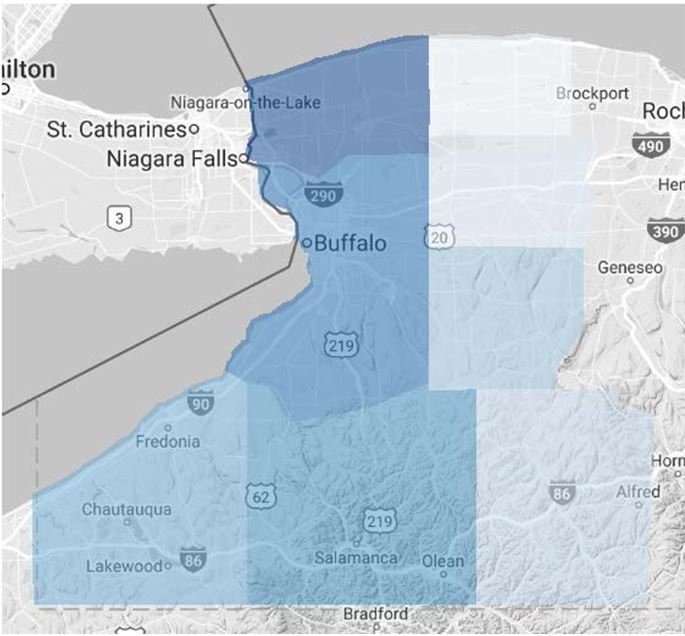
Our goal is to provide population health management programs and services to some 250,000 attributed Medicaid members across the eight counties of Western New York.
|top of page|OUR JOURNEY
MCC Provider Needs Assessment
- According to the NYS 2014 Managed Care Survey in WNY:
- 81.6% of Medicaid MCO Expenditures were governed by FFS arrangements
- 17.8% were governed by VBP Level 0 Arrangements
- Of 73 provider partners that were surveyed by MCC:
- Only 1 provider was receiving extensive clinical information from the MCOs
- The majority of our provider partners received:
- No data at all – 41%
- Basic data – 26%
- Limited or selective data –16%
- Few partners had a 360–degree comprehensive view of the patients they were attempting to manage.
MCC – Our Partners and VBP
- The introduction of Value Based Payment into this market has resulted in a flurry of recent discussions and activities around the formation of IPAs and ACOs:
- There is an increasing demand for the tools and analytics that will be needed by these organizations to support VBP contracts and ensure optimal population health management.
- Millennium is committed to supporting a regional population health management strategy in this region and has invested in the Cerner HealtheIntent population health management platform.
98% of our network partners have expressed a willingness to use a population health management tool provided by MCC.
|top of page|CHASING THE DATA
- Millennium has developed a multi–tiered strategy to collect and populate CERNER HealtheIntent with data. Our partners include:
- WNY RHIO – HealtheLink
- EMR and Clinical Data Feeds from Hospital Partners
- FQHCs
- Managed Care Organizations
MCO DATA SHARING AGREEMENTS
MCC and MCO Collaborative
- Identify "win–win" opportunities and partner on targeted performance improvement initiatives that benefit both organizations.
- Create data sharing agreements and exchanges that promote optimization of the management of the Medicaid population.
- Create an inventory of programs and incentives for both the providers and members. Identify opportunities to promote and/or collaborate in a manner that maximizes desired outcomes. Avoid duplicative programs.
- Support the introduction and adoption of value based payment arrangements within the community.
Data Sharing Contract – Structure
- Zero Cost Management Services Agreement:
- Contract is between MCC and IHA for population health management services.
- MCC has contracted with Cerner for the population management health platform.
- Data will be sent directly from IHA to Cerner.
- Initially the data will be limited to Medicaid patients attributed to MCC as defined by the NYS MCC Patient Roster.
Scope of Work
- Accept and stage data for reporting and analysis in Cerner´s HealtheIntent population health management platform using Independent Health enrollment, medical and pharmacy claims for attributed Medicaid members.
- Generate performance reports on mutually agreeable key performance indicators for a physician´s members, as attributed by Independent Health.
- Populate patient chronic disease and wellness registries with IHA data to assist physicians and practices with the identification of gaps in care, targeting members for outreach and performing pre–visit planning.
- Provide a care management tool to enable care and transition planning across care settings.
- Provide leading practice guidelines and support for Care Coordinators at Millennium´s contracted medical and behavioral health providers to achieve our mutual targeted performance objectives.
- In collaboration with Independent Health, provide analytic services to identify opportunities for improvement on targeted high value performance metrics.
- Educate and mobilize medical and behavioral health providers to develop and implement plans for quality improvement.
- Collaborate with community–based organizations to identify and address social determinants that are barriers to engagement in care.
Compliance and Risk Assessment
- The submission of a very detailed Vendor Risk Assessment that outlined MCC and Cerner policies, controls, security protocols, workflows and system requirements/specifications relating to data exchange was required.
- This assessment has been reviewed and approved by the IHA legal, risk and compliance teams pending receipt of additional MCC desktop security policies and controls.
- Once these documents are received and approved, IHA is poised to deliver a contract template to our legal team.
Business Continuity Controls
- Business Continuity Plans:
- How often do updates occur?
- How are emerging threats and vulnerabilities incorporated into the Plan?
- Recovery Plans:
- Primary and Secondary sites
- Disaster Recovery testing
- Invoking Business Continuity Plan
- Documentation of Previous Business Interruptions / Outages –
- Cause, remediation and recovery timeframes.
- Regulatory Agency Issues or obstacles impacting recovery efforts
- Strategies/Plans for the following:
- Loss of work space
- Personnel shortages or unavailability
- Degradation of service
- Data center outages o Application Outages o Cyber Attacks
- Operations at Recovery Site
- Server Capacity
Compliance Controls
- Compliance Officer
- Internal Department dedicated to corporate compliance and healthcare regulatory compliance
- Compliance risk assessments related to regulatory compliance
- Notification of changes in ownership or criminal convictions by managing employees
Offshore Oversight
- Details of all contractual/sub–contractual arrangements
- Assessment and Evaluation of alternatives
- Type and amount of PHI associated with the arrangement
- Regulatory Requirements incorporated into the agreements Policies and Procedures
- Training
- Auditing
Vendor Oversight
- Delegation and sub–contracting controls
- Oversight functions – auditing, compliance
- Deficiency Remediation
- Training Requirements and oversight
- Policies and Procedures –Record Retention
- Compliance Training – including Fraud, Waste and Abuse
- Type of Training
- Frequency of Training
- New Hires
- Specialized Training
- Exclusion and Sanctioned List Checks (OIG, LEIE, GSA, EPLS, OMIG, OFAC) including frequency
In the Interim
- The MCOs have provided MCC with aggregate information and current trends for:
- PCP Access
- Non–utilizers
- Avoidable admissions and readmissions
- Preventable ED visits
- Medication Adherence Measures
- The MCO is sending a list of patients who are non–compliant with targeted DSRIP P4P measures directly to the providers.
- MCC is deploying resources to review this data and work with the practice to develop work flows and a plan of action to manage these patients and improve performance.
- The MCOs are actively working on solutions to address billing and claims issues that MCC has identified as barriers to improving the performance metrics and meeting NYS DSRIP targets.
Follow Us