NEW YORK STATE MEDICAID REDESIGN TEAM (MRT) WAIVER
- Draft DSRIP Waiver Amendment Proposal is also available in Portable Document Format (PDF)
1115 Research and Demonstration Waiver #11-W-00114/2
Extension and Renewal Request
New York State Department of Health Office of Health Insurance Programs
One Commerce PlazaAlbany, NY 12207
November 27, 2019

Section I – Program Overview, Goals and Objectives
Program Overview and Phased Approach
The last five years was a groundbreaking and transformative time for New York´s Medicaid program. Through the current waiver, significant strides were made to transform Medicaid delivery systems to meet the myriad and evolving needs of Medicaid members today, while building infrastructure that supports providers´ ability to increase efficiencies in the delivery of care, engage in risk-contracting, and support population health.
The current 1115 waiver represented a crucial first step in New York State´s (the State´s) transition to value-based payment (VBP), which set a trajectory for the State´s continued advancements towards value-based care. This transition has resulted in moving Medicaid provider contracts into early risk-based arrangements and testing models of collaboration to support provider and managed care organization (MCO) ability to address social determinants of health (SDOH). Medicaid providers earned incentives for creating integrated, high- performing health care delivery systems that improve quality of care, support population heath, and reduce costs. Continuing this critical work while building a transition to even more integrated structures and reward pathways will be important to sustaining gains made. Further developing these clinical network partnerships by deepening existing relationships and workflows, adding new partners, and engaging MCOs will further strengthen local continuums of care and increase efficiencies across delivery systems.
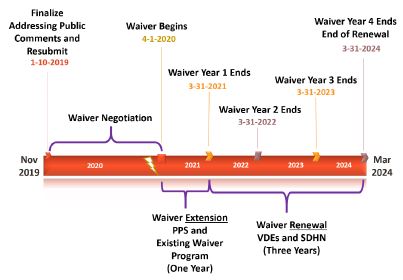
In this new waiver amendment proposal, the State seeks to transition the current waiver in two phases: (1) the Waiver Extension (Phase 1) from April 1, 2020 – March 31, 2021, during which the State will continue the existing waiver efforts, but in a streamlined fashion; and (2) following a robust stakeholder process that will take place during Phase 1, the Waiver Renewal (Phase 2) from April 1, 2021 through March 31, 2024, during which the State will build new entities to permanently sustain promising practices from the current waiver through more robust VBP contracting. This combined four-year period will allow the State to fully transition to sustainable models of VBP supporting the best system restructuring and clinical improvement models advanced by the waiver.
Historical Context
On April 14, 2014, the State and the Centers for Medicare and Medicaid Services (CMS) reached agreement on a groundbreaking 1115 Medicaid waiver that allowed the State to invest $8 billion of the $17.1 billion in federal savings generated by the Medicaid Redesign Team (MRT) reforms for comprehensive Medicaid delivery and payment reform. Since its approval by CMS, the State transformation has provided incentives for Medicaid providers to create and sustain an integrated, high-performing health care delivery system that can effectively and efficiently meet the needs of Medicaid members in their local communities by improving the quality of care, improving the health of populations, and reducing costs. This effort also represented the first step in the State´s transition to VBP, which set a trajectory for the State´s continued advance toward value-based care.
This transformation promoted community–level collaboration and sought to reduce avoidable hospital use by 25 percent over the five–year demonstration period, while financially stabilizing the State´s safety net providers. A total of 25 Performing Provider Systems (PPSs) were established statewide to implement innovative projects across three domains: system transformation, clinical improvement, and population health improvement (New York´s Prevention Agenda).1 All funds have been awarded based on provider achievement of performance goals and project milestones.
Demonstration Progress to Date and Newly Identified Needs
Through the innovative efforts of the 25 PPSs and their partners, the State has achieved significant reductions in avoidable hospital use through Measurement Year (MY) 4 ending June 2018. Potentially Preventable Admissions (PPAs) have been reduced by 21%, and Potentially Preventable Readmissions (PPRs) by 17% (Exhibit 1).
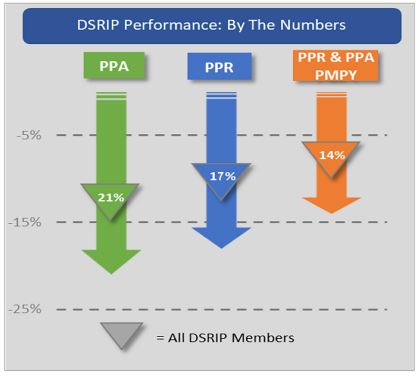
Exhibit 1
The combined reductions are estimated to have reduced per member per year preventable costs by approximately 14% over the last four measurement years, saving more than $500 million through MY 4 for these preventable events alone.
But those are just the averages. An even more impressive story emerges when looking specifically at those PPSs adopting the most promising practices. Eleven PPSs saw avoidable admission and readmission reductions of over 25 percent, with a five PPSs driving decreases of 38 and 39 percent on PPAs and PPRs, respectively, from baseline. Also, when looking from a patient lens, those members qualifying for health home (HH) care management saw average reductions of 25 percent or more in both measures of avoidable hospital use (Exhibit 2).
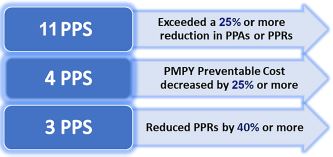
Exhibit 2
In addition to these reductions in avoidable hospital use, the Independent Evaluation has shown even more overall success including improved performance in the majority of behavioral health and population health measures in the interim evaluation period (through measurement year 3). Additionally, results for the asthma medication ratio measure improved, as did early indicators of system change, such as members connectedness to providers (usual source of care) and reduction in uninsured use of emergency department (ED). Of note, PPSs
As a result of the work thus far, integrated delivery networks have developed, strengthened, and matured over the waiver period to collectively improve performance in both quality and cost-savings. These new networks have advanced never-before-tested service models and now have had the shared experience of meaningful collaboration to exceed performance targets and earn the most challenging of waiver incentive payments. By doing so, these networks have been able to further participate in innovative VBP arrangements. In just a few years, New York has significantly moved its Medicaid program from almost exclusively fee-for-service to paying for value. Today, approximately seventy percent of the State´s Medicaid managed care expenditures are contracted under a VBP model, and approximately 45% are contracted in risk arrangements where providers share in financial risk for cost and quality outcomes. New York was first in the nation to require that certain VBP arrangements include Social Determinant of Health (SDOH) interventions and contractual agreements with one or more community-based organizations (CBO). Every VBP risk arrangement (45% of Medicaid managed care expenditure) have a defined SDOH intervention and include community-based human and social services organizations.
These first steps toward value-based care have moved rapidly and have established an initial structure through which New York State´s VBP model is defined; this strong foundation is necessary to bring VBP to full adoption. However, the VBP model must evolve to achieve the stated goals of delivery system and payment reform. VBP arrangements must incorporate more sophisticated provider networks that span the continuum of care and meet the unique needs of Medicaid members. Providers and MCOs must refine data exchange strategies to identify opportunities for improving cost and quality outcomes. Finally, MCOs and providers need time to structure VBP arrangements so that the most impactful evidence-based and promising performance-based practices can be sustained through shared savings.
The very promising population health work and forays into VBP are encouraging; however, more time is needed to directly support the best work and facilitate VBP maturation to continue the invaluable progress made to date. This additional time will allow the State to continue the promising practices from the current waiver and build on this outcomes-based performance, while more fully benefiting from collective shared savings and upstream reinvestment opportunities resulting from those efforts. Specifically, current VBP arrangements built exclusively around primary care provider (PCP) attribution and networks do not completely embrace the kind of comprehensive integrated primary care, behavioral health, long-term care, and other public health and social care capacities, including collaboration with local health departments (LHDs) and their community health coalitions, that have been at the heart of most of the initial waiver success. Accordingly, the required savings to power the most promising practices will be available on a broad scale only when VBP contracts mature to add more partners and embrace more sophisticated payment models that share accountability, performance, and payment risk across a broader continuum of providers and partners.
Two Phase Approach to Waiver Implementation:
As referenced above, the State proposes to transition from the current waiver in two phases aligned with the Waiver Extension (Phase 1) from April 1, 2020 – March 31, 2021 and Waiver Renewal (Phase 2) from April 1, 2021 through March 31, 2024.
Phase One – Extension:
In this phase, the State will continue the existing PPS efforts, but in a streamlined fashion, with performance rewards going out exclusively through pay-for-performance on a narrower set of higher priority performance measures. This Renewal Phase will be fully funded by funds "rolled over" as unspent in the prior waiver period. During this extension period, the current PPSs will remain in place, continuing their current projects and initiatives that have proven successful at achieving high-level goals of reducing avoidable hospitalizations, lowering costs, promoting SDOH interventions, and readying providers for value-based care. PPSs will focus on the most Promising Practices from the prior waiver and will move to further support efforts to increase the breadth and scope of VBP arrangements.
During the Waiver Extension period, the State will create two funding pools: the base performance pool and the high-performance pool. The State estimates that approximately $625 million will be unspent from the prior waiver period. Eighty (80) percent of available unspent dollars from the initial waiver will be deposited into the base performance pool and twenty (20) percent in the high-performance pool. PPSs will earn awards from the pool through gap-to-goal performance just as in the prior waiver period, but performance will be ranked so that the pool funds are fully liquidated and paid based on relative PPS performance for each measure in each pool.
To ensure the maximum impact is achieved, the State will, with very limited exception, only use a pay-for-performance (P4P) model and focused on a narrower set of high-impact and VBP- aligned measures from the existing measure set. These measures will remain fully connected to the existing approved PPS projects (i.e., no new measures). The only pay-for-reporting (P4R) measures that will remain are four measures where the State is transitioning from medical record chase and chart review to electronic reporting (e.g., Blood pressure control). Consistent with this goal to drive maximum impact, measures where the State has been "topping out" will be removed.
Each PPS seeking funds during the Waiver Extension period must submit a Phase Two implementation plan to the State demonstrating ongoing readiness to continue transformation efforts and associated partner payments. This plan will include how the PPSs will refocus efforts to the Promising Practices referenced below and begin local conversations readying stakeholders for Phase Two (renewal)).
Phase Two – Renewal
Following a robust review and vetting process with stakeholders to ensure that sure the State is on the correct path forward; the State will transition into the Waiver Renewal (Phase 2) of this proposal. This phase will include building new or reconstituting entities to permanently sustain promising practices (including SDOH) through more robust VBP contracting. In response to the public comments received to date, the State is advancing a retooled design for services integration, care management, and the more successful braiding of health, behavioral health, and social care into a consolidated service organization structure. This new structure includes a pivot from PPSs to Value Management Organizations (VMOs)2, which will include deeper integration of MCOs and CBOs. CBO services will be further organized and linked to health transformation activities through the development of regional Social Determinate of Health Networks (SDHNs).
Promising Practices: Documenting Evidence-Based Best Practices
Many best practices and lessons learned from the waiver effort are documented as "Promising Practices" in a report on strategies for meaningful change for New York Medicaid issued by the United Hospital Fund in July 2019.3 These select initiatives demonstrate the transformative regional and community collaborations among a diverse set of health system and social service providers that have impacted quality and clinical outcomes and earned PPSs the performance based incentive payments. These unprecedented efforts have been labor-intensive, requiring the formation of new relationships to better serve consumers and iterative testing to understand which innovations yield the best results at the local level. The State and its partners learned new workflows take time for maturation to yield optimal results. During the original waiver, each region learned much about the most effective partnerships to advance this important work. In some cases, the PPS as an entity has been the major driver of change. In others, subgroups working in carefully tailored medical markets have collaborated to address specific issues or subpopulations.
During the Waiver Extension (or Phase 1) of this request, the State will continue the existing PPSs´ efforts under a leaner structure designed to dovetail into the Waiver Renewal (or Phase 2) of this waiver request, where additional flexibility will be allowed to fund focused teams composed of providers, CBOs, MCO and LHDs, among others, to implement the high-priority Promising Practices. The collective Waiver Extension and Renewal efforts will allow the State to transition from demonstrating the success of system redesign and clinical improvement elements to building the most successful capacities into sustainable VBP contracts. Importantly, both phases of the amendment proposal will support the innovative transformative elements realized by the PPSs to be further developed and scaled with the MCOs as part of VMOs and VBP arrangements, while driving purposeful alignment with current federal healthcare initiatives and priorities.
Newly Identified Gaps and Needs
While great strides were made, more work is yet to be done. Key successes and identified challenges include:
- Meeting and Maintaining the shared goal of 25% reduction in avoidable hospitalizations. By extending the waiver program by one year, the State and its partners can collectively achieve the goal of reducing avoidable hospitalizations by 25%, and maintaining this reduction, generating even more savings to be shared by the State and Federal partnership.
- Building capacity for population health and value-based care with non-clinical providers such as LHDs, particularly to address SDOH. New relationships and collaboratives formed between SDOH providers and clinical providers implementing innovative approaches to integrate SDOH services as part of treating the whole person in impacting the non–medical factors to improve outcomes.4 New York providers spearheaded many innovations to address SDOH; however, these efforts need to be brought to scale. Through the course of the current waiver, the State learned that many SDOH providers are not integrated into clinical care approaches and protocols due to existing fragmentation of health and social services delivery systems. The current waiver programs were limited in its ability to build capacity for these providers to engage in more meaningful ways. This proposed amendment, especially during the Waiver Renewal phase, seeks to close those gaps so that downstream, non-clinical providers are effectively positioned to participate and engage in value-based care, and receive adequate reimbursement for services provided.
New York has been on the forefront when it required the use of SDOH interventions by investing State Medicaid dollars in housing, by promoting the inclusion of CBOs in PPSs, and requiring MCOs to include SDOH interventions in VBP contracts. Initial partnerships of CBOs and PPSs have been formed under the waiver, integrating SDOH services to impact non-medical factors, treating the whole person and improving their outcomes.
Alignment with Federal Goals
Healthcare transformation is most effective when State and Federal partners share aligned goals. The State has, and will, assess all elements of the amendment request for alignment with federal performance measurement approaches, programmatic approaches, promising practices from the CMS Center for Medicare & Medicaid Innovation (CMMI) and the Quality Payment Program, and efforts by the Medicaid Innovation Accelerator Program as well as data sharing and interoperability goals. These efforts must be robust enough to accommodate future programmatic and funding changes, with anticipated new guidance coming over the course of the upcoming year.5
An important shared goal of the State and CMS is the need to increase the depth of value-based care and contracting models. Core to Waiver Renewal period of the proposal is the development of entities that can support MCOs, providers, and CBOs to engage together collectively in risk-based contracts that drive value by improving health outcomes while generating shared savings that support ongoing population health and high-value promising practices.
In both the Waiver Extension and Renewal periods, the State will focus on higher-value promising practices from the current efforts that have demonstrated evidence of success and are clearly aligned with federal priorities. As outlined in Exhibit 16 of Appendix A the State outlined where the proposed focus areas align with identified federal priority areas that include: Substance Use Disorder (SUD) Care and the Opioid Crisis; Serious Mental Illness (SMI)/Serious Emotional Disturbance (SED); SDOH; Primary Care Improvement; and Alternative Payment Models (including value-based payments).
Within those priority areas and building on the work from the current waiver period, the following promising practice categories proposed for both phases of this amendment include:
- Expansion of Medication-Assisted Treatment into Primary Care and ED settings;
- Partnerships with the justice system and other cross-sector collaborations;
- Primary care and behavioral health integration;
- Care coordination, care management, and care transitions;
- Expansion of Mobile Crisis Teams (MCT) and crisis respite services;
- Focus on patients transitioning from Institutions for Mental Diseases (IMDs) to the community;
- Focus on SMI/SED populations;
- Addressing SDOH through Community Partnerships; and
- Transforming Primary Care and Supporting Alternative Payment Models.
Goals and Objectives of the Proposed Waiver Renewal
Apart from the need for the Waiver Extension as described above, the State proposes a Waiver Renewal (or Phase 2) to its 1115 Medicaid waiver for the purposes of establish a more robust framework to drive value-based care. Our goals for this Waiver Renewal phase of the proposal include:
- Improving the health outcomes and patient experience of the Medicaid population, including deeper integration across physical health, behavioral health (mental health and substance use disorder services), MCOs, public health and social services to collectively meet the myriad, evolving needs of the Medicaid members to live healthy lives in their communities;
- Improving the efficiency of the delivery systems, particularly as providers operationalize interventions addressing SDOH; and
- Incentivizing MCOs and providers as they continue to engage more highly integrated networks including CBOs in value-based care, supporting deeper and more sophisticated levels of risk contracting.
The State seeks to build on the lessons learned from its current waiver and develop an ongoing framework that will integrate providers across the care continuum with MCOs and CBOs, including LHDs, build new workflows that create efficiencies across programs, advance existing value-based arrangements, and support new payment models to ensure ongoing sustainability of Medicaid as a critical safety net program. Past efforts focused on building integrated delivery networks and population health infrastructure largely focused on clinical providers in the continuum of care.
The proposal for the Renewal Period would not just be a continuation of the current waiver program or the activities during the Waiver Extension period but will instead build upon prior efforts in a targeted way and align with federal goals to enhance the collective payment and delivery models. The State seeks to add MCOs, and non-clinical providers, particularly those crucial to address SDOH. It will fill newly identified gaps and deepen the delivery system´s ability to address SDOH interventions needed to keep Medicaid members healthy and stable in the community, while meeting the fiscal and service needs.
These objectives will be achieved through the establishment of VMOs and SDHNs working with MCOs, providers across the care continuum, public health, social services, and Qualified Entities (QEs)--the State´s regional health information organizations that connect to the Statewide Health Information Network-that are supporting data exchange across the State.
Collectively, these entities will work together to improve care delivery on individual and collective bases with the ultimate goal to improve cost and quality outcomes for New York´s Medicaid members under a sustainable VBP model that aligns with federal goals. Specific objectives include:
- Bringing to scale evidence-based Promising Practices that increase the value of care provided through the State´s Medicaid program;
- Supporting MCO-provider risk contracting by increasing the number of risk-bearing value-based contracts between and among MCOs, providers and CBOs, beyond the stated goals of the CMS approved Value Based Payment (VBP) Roadmap, "A Path toward Value Based Payment: New York State Roadmap for Medicaid Payment Reform;
- Supporting MCOs in developing new contracting models that address the needs of the whole person, including engagement with CBOs that impact patient health outcomes through addressing SDOH;
- Developing infrastructure and workflows between clinical, public health and social service providers to address SDOH in an integrated manner; and
- Focusing on key, high-priority areas not fully addressed specifically in the current wavier program, including long-term care, maternal mortality, children´s health, and opioid/substance use disorders.
Promising Beginnings and the Need for Continued Transformation
during the Waiver Renewal PeriodThe results of the early population health work and early forays into VBP in the current waiver and proposed Waiver Extension period are encouraging; however, more time will be needed to bring high value Promising Practices to scale and facilitate VBP maturation to continue the invaluable progress made to date. This additional time will allow the State to build on extremely promising outcomes–based performance while more fully benefiting from collective shared savings and upstream reinvestment opportunities resulting from those efforts.
Specifically, current VBP arrangements built exclusively around primary care provider (PCP) attribution and the networks do not completely embrace the kind of comprehensive integrated primary care, behavioral health, public health and other social care capacities that have been at the heart of most of the waiver success. As the State gains experience with provider risk contracting, the State acknowledges that the transfer of financial risk alone does not always support integrated, whole person approaches to care. Thus, the required savings to power the most Promising Practices will be available on a broad scale when VBP contracts mature to add more partners and embrace more sophisticated payment models that share accountability, performance, and payment risk across a broader continuum of providers collaborating on outcome improvement.
Some of the best examples of value–oriented collaborative work has been driven by progress actualized in Year 3 and Year 4 of the initial waiver, when project implementation matured to meet the needs of P4P based accountability. Transformative work has been focused on the significant undertaking of building partnerships and trust and clearly requires more time for maturation at scale. The continuum of community health and SDOH providers that has greatly contributed to moving the needle on population health must be recognized in VBP arrangements.
MCO engagement and partnership now need to be more meaningfully integrated to construct VBP agreements that recognize and sustain the new, non–traditional community partnerships that have demonstrated significant gains in performance and cost–savings referenced earlier.
VMOs are the mechanism to integrate MCOs and SDHNs into the Promising Practices, which, in turn, will drive more sophisticated VBP contracting with providers in the VMO network.
Demonstration Timeframe
The State seeks four (4) years in total to further support the cost savings and quality improvements being driven through the Promising Practices. As with the original Medicaid Redesign Team (MRT) waiver, New York State seeks an extension for the 1–year balance of the current 1115 waiver ending on March 31, 2021 and conceptual agreement, subject to further stakeholder feedback and input, to an additional three years from April 2021 to March 31, 2024. Accordingly, the full four–year extension and renewal period (1–year extension and 3 years of renewal) would span from April 1, 2020 through March 31, 2024.
Exhibit 3: Demonstration Timeframe
Section II – Phase 2 Program Description
The Waiver Renewal or Phase 2 of this proposal intends to build upon the successes and learnings from the current waiver that would be supported through the Waiver Extension (Phase 1). These successes and learnings were integral in developing clinical and population health infrastructure, supporting Medicaid members to achieve better health outcomes, and encouraging providers to engage in VBP contracting. As part of Phase 2, the State seeks to build on what worked and proliferate Promising Practices that improved health outcomes and decreased costs across the State. Further, continued transformation efforts as part of the proposed Waiver Renewal will address gaps in infrastructure beyond what has been built by, between, and among clinical providers and MCOs, in order to integrate SDOH providers and CBOs as a collective, co-managed approach to meeting the needs of the whole person. As indicated above, Phase 2 of this amendment proposal would allow the State to add two critical infrastructure pieces supporting these efforts to local delivery systems, namely VMOs and SDHNs.
The State and CMS´s shared goal of infusing VBP arrangements into the New York healthcare system beyond the confines of the initial waiver is further supported by the structural changes proposed. In doing so, the State is creating a pathway in this amendment proposal for a variety of entities in the health care delivery system—including MCOs, providers and CBOs—to move even further towards a unified, cohesive approach to value-based care models and arrangements. With this transformation, VMOs, and SDHNs will scale and expand what works while resolving emerging gaps and needs. They will also support MCOs, providers and CBOs as they seek to serve vulnerable populations identified as needing enhanced focus by the State.
Establishing VMOs to support providers and plans in the march towards value
A central component in the Waiver Renewal phase of the amendment proposal is the creation of VMOs. VMOs will further the goals and objectives of the Promising Practices and serve as a critical coordination point across integrated delivery networks, including as a convener, facilitator, point of shared learning and quality improvement champion. They will also provide technical support to their stakeholders (MCOs, clinical and SDOH providers, such as LHDs and CBOs) as they collectively build new VBP contracting models and implement clinical and social interventions to meet the needs of different patient populations.
One primary goal is the proliferation of more sophisticated VBP arrangements, creating mechanisms to scale and sustain promising practices to improve quality and drive efficiency. Leveraging previous population health and chronic disease clinical improvement projects, VMOs would be required to integrate Prevention Agenda goals. This integration should focus on extending the Promising Practices upstream towards primary and secondary prevention; including partners actively engaged in these activities to increase the potential for bending longer-term utilization and cost trends.
Based on an analysis of the roles and achievements of the PPSs under the current waiver, VMOs will function as the vehicle to finalize the State´s goal to transition to Care Management for All through funding an integrated program that builds on the Promising Practices and creates an inclusive and cross-disciplinary network for participating in and advancing population health initiatives, thereby enabling and rewarding the successful growth and evolution of VBP arrangements.6 Working with SDHNs, VMOs will be integral to supporting MCOs´ ability to incorporate funding for SDOH into provider contracts.
In performing these functions, VMOs are not intended to duplicate any existing care management efforts or infrastructure, but rather to coordinate, orchestrate and build upon existing–and sometimes overlapping–care management activities among its participants. Essential to this coordination and orchestration will be working closely with MCOs in their respective regions and across lines of business. VMOs will be designed to coordinate and create accountability for these care management activities and initiatives.
Moreover, VMOs should be structured to support (and not replace) existing VBP provider networks, including integrated delivery networks, accountable care organizations (ACOs), independent practice associations (IPAs) and Behavioral Health Care Collaboratives (BHCCs), as well as other provider network configurations (collectively, Provider Networks) that have already been formed to engage in MCO and VBP contracting. In this configuration, existing Provider Networks may leverage their existing activities to participate cohesively in VMOs and in VBP arrangements.
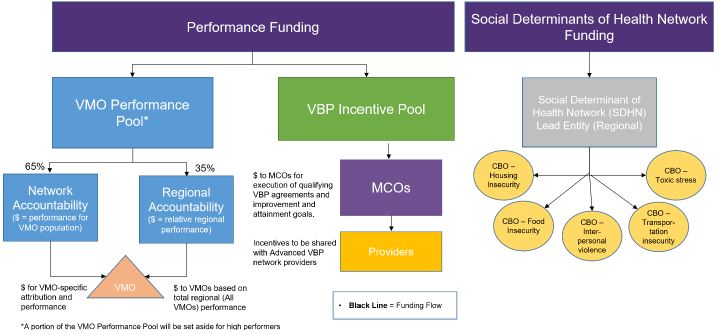
To that end, VMOs will not be a new type of Provider Network. Rather, in addition to engaging in direct activities for furthering the Promising Practices, VMOs will have a longer-term purpose as a support or services organization. Provider networks and MCOs pursuing sophisticated VBP arrangements will be able to use the infrastructure and collaboration built around value-driven population health and care management, which is designed to achieve positive health outcomes and lower costs over the course of the waiver program. To further these transformation objectives, the State will utilize a hybrid approach, by apportioning waiver funds into two interrelated and performance-based pools (the Funding Pools):
- VMO Performance Pool: Programmatic awards made available directly to VMOs based on member attribution and potential performance in driving the Promising Practices and other high-need projects, including but not limited to better orchestrating care management efforts, achieving pre-established quality measure goals (e.g., PPAs, PPRs), establishing bidirectional data capabilities and creating care linkages between and among the VMO participants; and
- VBP Incentive Pool: Incentive awards made available to MCOs, and by extension SDHNs and provider partners, through their VBP contracts. The funds would encourage evolution of their agreements into more sophisticated VBP contracting arrangements and would be conditioned upon (a) meaningful participation in the governance and programmatic initiatives of at least one VMO in their region(s), and (b) executing qualifying VBP agreement(s) between an MCO and an appropriately composed network of non-MCO partners in a VMO network.
Each funding pool is structured to create incentive-based award opportunities based on achieving performance and accountability milestones established for their respective funding pools and attributed member populations (Network Accountability). These pools are intended to support the development of VMOs and SDHNs, as well as both fund and support engagement and shared infrastructure to perform successfully under provider contracts post-demonstration and to generate savings under those contracts.
Integration of social determinants through new Social Determinants
of Health NetworksAs part of the Waiver Renewal phase, the State proposes to further advance this work through the development of SDHNs to 1) organize a wide range of non-clinical providers needed for SDOH interventions, 2) support these providers to engage in VBP contracting, and 3) deliver socially focused interventions linked to VBP.
Each SDHN will consist of a network of CBOs within each region of the State to provide evidence-based interventions that address housing instability, transportation, food insecurity, interpersonal safety, and toxic stress. The State will designate regions and select a lead applicant within each region, which may be a CBO itself or a network entity (e.g., an IPA) composed of CBOs. The lead entity will create a network of CBOs that will collectively use evidence–based interventions to coordinate and address housing instability, food insecurity, transportation, interpersonal safety, and toxic stress.
The role of the SDHN is to develop and scale comprehensive SDOH interventions in alignment with the population health agenda of the VMO. To this end, LHDs will be an important partner to the network. Similar to the VMO, the SDHN will function as a convener of CBOs, coordinating CBO activities and providing essential infrastructure for success under the VBP paradigm.
Although VBP arrangements include interventions that address social and environmental barriers to better health, they are often not far reaching in their scope relative to the full social burden of the populations being served. Further, VBP arrangements must develop payment structures that effectively and appropriately reward the delivery of SDOH interventions, while having the agility to flex intensity of services depending on the needs of the Medicaid member(s). For example, a chronically homeless patient with opioid addiction would need different interventions than a senior with long term care needs and housing instability due to rising rental rates. Accurately targeting SDOH interventions, scaling them effectively and measuring SDOH outcomes remain challenges that are capable of being addressed by this waiver proposal.
The construct of VMOs and the incentives to drive regional collaboration among MCOs, providers, and SDHNs will help organize CBOs, create partnerships, and build infrastructure to support and enable timely referrals and access to social services in closed loop structures. The SDHN will play a key role in the governance of the VMO, representing the interest of the convened social care network. Similarly, SDHNs will be critical to support provider and CBO ability to refer and coordinate patient engagement and receipt of non-Medicaid funded programming that supports self-sufficiency, creating a regional discussion around braiding of funding to ensure efficient use of State and Federal dollars. Please refer to Exhibit 4 below for a visual depiction of the funding pools proposed.
Exhibit 4: Proposed Funding Pools (not inclusive of IAAF or Workforce Development Funds)
Bringing High Priority Promising Practices to Scale Statewide
Critical to the success of the waiver proposal, both during the Waiver Extension and Waiver Renewal phases, will be the preservation and proliferation of the most Promising Practices Statewide. In this waiver proposal, the State seeks to create meaningful structural change beyond the initial waiver that will allow the Promising Practices to mature, as well as allow the transformation of VBP by utilizing SDHNs and VMOs to address the whole Medicaid individual. These Promising Practices will support chronic disease management and member self- management for both children and adults, particularly in the areas of asthma, cardiovascular disease, diabetes, and Human Immunodeficiency Virus (HIV) infection. For those with diseases in more advanced stages, Palliative Care initiatives will focus on improving quality of life. Palliative Care recognizes the symptoms and stress of the disease and its treatment, entailing a broad range of issues that can include pain, depression, anxiety, feeling "at peace," and loss of appetite, as well as addressing advance directives. At the advanced end of the spectrum, Hospice Care moves away from "cure" to comprehensive comfort care for the individual and support for the family. Hospice care can be delivered in the home, assisted living, nursing home, or inpatient setting. See Long-Term Care section for more information on Palliative Care and Hospice Care investments.
While these practices will be key to both the Waiver Extension and Renewal phases, beginning in the Waiver Renewal phase, each VMO will be required to select Promising Practices that are most appropriate for the population served in their region or for their subpopulation based on their community needs assessment. However, in addition to matching the Promising Practices to the community needs assessment, each VMO will be required to implement five high-priority Promising Practices focus areas. These high-priority focus areas include:
1) Transforming and Integrating Behavioral Health – Specifically through Peer Outreach and Expansion of Crisis Capacity;
Transforming and continuing to integrate BH into primary care will be an ongoing focus for the next waiver period. In the current waiver all 25 PPSs undertook BH integration projects, employing up to three models of integration – 1) Integration of BH into Primary Care settings, 2) Integration of Primary Care into BH settings, and 3) the IMPACT Model of Collaborative Care. With approval of the Waiver Renewal these efforts will continue by strengthening and sustaining current efforts and expanding integration to new practices site, while continuing to address the challenges presented by collocation in certain settings, such as hospital outpatient departments and Federally Qualified Health Centers (FQHCs).
For SUD, care transitions and follow-up treatment may be more effective with support from peers who have already successfully navigated the system, from detoxification through rehabilitation and onto recovery. Peer recovery coaches connect with individuals, ensure attendance at the first outpatient appointment, connect individuals to recovery supports in the community, help them with navigation of the healthcare and social service systems, and ensure any missed appointments get rescheduled. Peer coaches have the lived experience that resonates with persons suffering from addiction, helping to build their confidence and trust, and can be the first bridge back into a system of care.
Individuals experiencing a BH crisis may often not need treatment in the ED or hospital if they can access successful de-escalation resources in an ambulatory setting. Co-located with ambulatory services, BH urgent care or crisis centers can act as a bridge to BH treatment, which is often difficult to access for both children and adults. Such programs help close the gap by providing mental health assessments, treatment referrals, treatment initiation (if necessary), and care coordination with medical and behavioral health providers, schools, and/or other community resources.
2) Care Coordination, Care Management and Care Transitions – Specifically through hot spotting, development of transitional care teams, and leveraging telehealth
Medicaid members with complex medical, behavioral, and social needs often use hospital services at significantly higher rates than other members. In many cases, use of these services can be avoided through better navigation of the health system and existing community resources. The community navigator often performs a role similar to that of a community health worker or care manager, helping individuals schedule appointments, coordinate transportation, or accompanying individuals to their appointments.
Recognizing that a medical or BH event requiring hospitalization can provide a critical moment for supporting individuals in the healing/recovery process, thereby preventing potential readmissions, "Transition of Care" programs support individuals transitioning from an inpatient medical or psychiatric setting back into the community. Under these programs, individuals in hospital-based medical or psychiatric units are introduced to a clinician and peer before they are discharged. This prepares them to receive peer support services and clinical assessments post-discharge. Collaboration between these clinical and community- based service providers helps individuals who have been discharged attend outpatient follow-up appointments and obtain assistance navigating community resources, such as crisis respite or transitional housing.
Another promising model is through transitional care nurses (TCNs) and managers organized into transitional care teams (TCTs), which provide safe and effective transitions of care for patients at particular risk for readmission. At-risk patients are identified through a modified LACE tool (which assesses length of hospitalization stay ("L"), acuity of admission ("A"), comorbidities ("C") , and ED utilization ("E")), a social determinants of health screening tool, and clinician judgment.7 These patients are referred to TCNs, who use assessments to create 30-day care-transition plans. In turn, the transitional care teams work with patients in the hospital and during a 30-day post-discharge period to address medication concerns and administer condition-specific teaching. TCTs also serve as a key link between patients and community-based clinical and SDOH providers.
Extending care management across settings and supporting disease self-management reveal some natural opportunities for telemedicine, where health care services are delivered to patients and their caregivers via information and communication technology. Recognizing that physically traveling to health care providers may be difficult for individuals in both rural and urban settings, telemedicine programs for triaging, treating, and monitoring non-urgent illnesses and injuries in patients´ homes can reduce unnecessary ED and urgent care visits and improve continuity of care between patients, physicians, nurses, and direct care staff. As examples, palliative care telemonitoring programs and BH telemedicine programs enhance access to primary care, support integration of palliative care into primary care via patient-centered medical homes and improve clinical care for those with BH conditions.
3) Addressing Social Needs, Community Partnerships and Cross-Sector Collaborations – Specifically, through Utilizing Community Health Workers (CHWs) and Linking to SDHN High-Priority Social Care
It is now commonly accepted that unmet social needs are a major determinant of health outcomes and health care spending. Successful care management often requires new workforce investments, such as contracting with partners to incorporate new staff within clinical workflows and building capacity among new and existing staff. Leveraging the VMOs´ newly developed community resource infrastructure from the current waiver, continued funding will support deepening CBO partnerships and cross-sector collaborations aimed at improving outcomes for specific populations. These alliances often rely on these new types of workers to tackle Medicaid members´ complex care management and navigation needs to connect them to social resources. Moreover, these resources span across sectors of the clinical and public health care systems, the educational system, and the criminal justice system, as examples, to improve outcomes for specific populations. For example, schools in underserved communities may have insufficient capacity to meet their students´ disproportionately greater BH needs, which may require new and different workforce models to address this gap.
As a result, investments in the health care workforce are important for increasing the number of professionals qualified to screen Medicaid members for unmet social needs and connect them to social services. Community health workers (CHWs) can support high-risk beneficiaries with unmet social needs who seek care in the ED or are admitted to the hospital. These workers can be the key to connectivity to outpatient medical, behavioral, social, and educational services. For example, CHWs can follow up with a home visit within 72 days of an ED or hospital discharge or ensure that the BH needs of a child identified by the school get addressed in the community, and then follow up regularly until the individual is fully engaged in care. During this time, CHWs provide persons with care management and warm handoffs to health care and SDOH providers. Serving as a critical bridge across different sectors and programs, CHWs can be trained to provide self-management education to patients and their caregivers and reinforce care messages delivered in the clinical setting to support adherence to medications and care delivery recommendations. They also help beneficiaries schedule primary care visits, secure transportation to appointments, apply for public benefits such as housing and food assistance, and maintain Medicaid enrollment when eligible. As needed, CHWs also connect patients with longer- term care supports, such as the HH program. The unique ability of CHWs to be extenders of clinical practice into the field, serving as eyes and ears of the providers, while meeting the unique needs of patients where they are is a critical missing bridge between clinical and community settings.
Additionally, CHWs may also connect with people who underutilize health care services because they lack the knowledge and skills to navigate the system. Promising Practices have included partner organizations using an outreach model in which CHWs enter the community to find and engage people who are not in primary care, and other partners use an "in-reach" model designed to engage members when they seek services. Aligned with the goals of improving access to primary care while also increasing patient activation, engagement, and self-management skills, CHWs help low- and non-utilizing Medicaid members and uninsured, Medicaid-eligible individuals connect to primary care and social services.
4) Addressing the Opioid Crisis – Specifically Medication-Assisted Treatment (MAT) expansion to primary and emergency department (ED) care and SUD peer bridging
Significant gains have been made to advance care for those with a diagnosis of Opioid Use Disorder (OUD) specifically and SUD generally. From Measurement Year 0 to Measurement Year 4 in the initial waiver, potentially preventable ED visits (PPVs) for persons with a BH diagnosis (includes SUD and mental health conditions) have decreased by nearly 2%, despite over a 35% increase in eligible members over the same period.
The next phase will build on the best practices implemented in the current demonstration such as:
- broad screening for OUD/SUD in primary care physician (PCP) practices (e.g. Screening, Brief Intervention, and Referral to Treatment, (SBIRT));
- MAT initiated in ED and PCP practices;
- MAT further focused on the justice–involved population,
- Hospital to community linkages, and
- deployment of peers in care transitions, navigation, and recovery.
VMOs will partner with their regional Centers for Treatment Innovations (COTIs), NY State´s Office of Addiction Services and Supports (OASAS) treatment providers, and Drug User Health Hubs (DUHH) that are focused on engaging people in their communities by offering harm reduction and mobile clinical services, as well linking people to other appropriate levels of care. COTIs target un/underserved areas and expand access to tele–practice, SUD services, and linkage to MAT, as well as peer outreach and engagement within the local community.
Besides continuing to expand MAT capacity in primary care offices, ED physicians are increasingly eager and able to prescribe MAT, giving the first dose in the ED and ensuring warm handoff to the outpatient office/clinic prescriber. These models will be expanded as a best practice and scaled to be supported in VBP arrangements. ED-initiated MAT supports meeting Medicaid members where they are at as part of a "No Wrong Door" policy.
Engagement with Project ECHO (Extension of Community Healthcare Outcomes) can empower rural, office-based providers across New York to address OUD with MAT integrated into office-based settings. Project ECHO provides on-site training and electronic consultation resources for staff through TeleECHO clinics. The model supports licensed, qualified clinicians to become prescribers and receive their Drug Addiction Treatment Act of 2000 (DATA) waivers to prescribe buprenorphine. These activities are linked to broader efforts to improve initiation of, and ongoing engagement in, alcohol and other drug dependence treatment, and to reduce potentially avoidable ED visits, hospitalizations, and readmissions (including those associated with OUD and its comorbidities).
An additional Promising Practice to replicate and scale in the next phase is the use of peer recovery coaches to support beneficiaries´ needs when transitioning out of treatment facilities into early recovery, ensuring attendance at the first outpatient appointment, and making a connection with recovery supports in the community. Additionally, peer recovery coaches can provide assistance with the navigation of health and social service systems and offer help rescheduling missed appointments. These efforts are consistent with performance goals related to sustaining engagement in alcohol and drug treatment and connecting adults to primary and preventive care.
As part of the expanded emphasis on children in this waiver amendment, special projects will be undertaken to engage teens addicted to opiates, alcohol, and other substances, including a focus on vaping. Further, special focus will be given to opiate-addicted pregnant women to engage them in care and treatment during and after the pregnancy, and to ensure appropriate treatment for their infants who are at risk for neonatal abstinence syndrome.
5) Addressing High Utilizers of Care through Rapid-Cycle Continuous Improvement processes.
Through NYS Medicaid´s Accelerated eXchange (MAX) Series, a highly touted success story has been the use of rapid-cycle continuous improvement (RCCI) activities to address high utilizers. Regardless of the chronic condition, the drivers of utilization are typically behavioral in nature, consisting of mental health, SUD, and unmet social needs. This Promising Practice will be required of VMOs to address high utilizers of care, both through new programs to address high ED and inpatient utilizers, but also through train-the-trainer activities to sustain these efforts.
As an example, after recognizing that many high-utilizing patients were receiving care from multiple health systems, partners in one region developed new processes for sharing clinical information on high utilizers and collating the information into a single hospital´s care management infrastructure, thereby bridging gaps in coordination across these providers. Through the MAX series project, the overall aim is to improve care management and follow- up for patients´ unmet BH, medical, palliative care, and social needs, along with any other underlying drivers of utilization. These efforts have been shown to significantly reduce ED and inpatient readmissions, lead to greater patient and staff satisfaction, and be amenable to replication and further scaling, including in other settings like long term care.
Building out these capacities will be a focused Statewide goal, and all VMOs will be required to incorporate these five high-priority Promising Practices. In their application to the State, each VMO will be required to include a specific project plan for replicating and scaling these high- priority focus areas. This project plan must detail how the VMO performance network will be utilized to build these activities across the region and how the MCOs, providers, and SDHNs (and their network of CBOs and partners) in the region will be leveraged to participate in these focus areas and assure they can be sustained through VBP arrangements by the third year of the demonstration.
While these high-priority focus areas are directly connected to performance on measures of preventable hospitalizations, chronic disease management, and BH, it will be important to assure that these capacities are built by attaching performance dollars to their specific development. To achieve this aim, the State will develop a payment structure in the VMO Performance Pool that specifically reserves funds, rewarding the degree to which these critical capacities have been developed.
To ensure transparency and accountability, VMOs, in collaboration with their stakeholders, will be required to develop and submit an approved implementation plan that:
- Documents the current state of need through a community needs assessment, including gaps in care, unmet needs, workforce gaps, missing infrastructure needs and provider shortages by type;
- Clearly identifies the Promising Practice(s) the VMO and its stakeholders will implement collectively (including the five high-priority Promising Practices) including linking the Promising Practice to the findings in the community needs assessment and how their selection addresses the gaps and needs identified;
- Clearly articulates how the VMO and its stakeholders will implement each chosen Promising Practice, including roles and responsibilities of key players by type; and
- Clearly identifies metrics and milestones by demonstration year, including the targeted types and number of services delivered and outcomes generated.
Deepening Value Based Payment Arrangements
As part of the Waiver Renewal period, the State will continue VBP implementation by refining existing VBP arrangements and establishing new and more progressive risk-based arrangements through stronger network integration, data sharing and adoption of sustainable evidence-based and promising performance interventions into value-based arrangements. The transition to VBP has been swift, resulting in very uniform total cost of care arrangements supported by narrowly defined provider networks. However, VBP implementation will benefit from more rounded and sophisticated networks, as new evidence shows that health and health outcomes are impacted by SDOH in a way that requires non-traditional, non-clinical provider intervention for successful stabilization of patients in the community.
The structure of VBP arrangements, including network composition, must evolve to fully realize the goals of value-based care. New York State´s Medicaid Managed Care VBP model is now at a pivotal point as MCOs and providers, including CBOs and their partners, focus their efforts beyond the transition to VBP and toward strengthening, improving, and refining their VBP partnerships and arrangements to improve efficiency, quality, and population health outcomes.
The next evolution of this transformation requires a focus on deepening VBP arrangements to drive maximum impact in the populations they serve. Deepening VBP requires MCOs, VMOs and Provider Networks to scale evidence-based and extremely promising outcomes-based performance interventions in an integrated fashion, to more fully benefit from collective savings and upstream reinvestment opportunities resulting from those efforts.
The State will maintain current levels of VBP and will create additional opportunities for MCOs and providers to adopt VBP arrangements where both parties are mutually accountable for improved cost and quality outcomes. This approach will continue to move Medicaid´s VBP model forward in alignment with other CMS programs, such as the Medicare Shared Savings Program and Direct Contracting. The State will continue to engage key stakeholders, including the VBP Workgroup and VBP Clinical Advisory Groups (CAGs), to evolve and shape the next iteration of NYS´ VBP model as defined in the VBP Roadmap through the following efforts:8
- Maintaining a core set of requirements that will continue to define VBP, such as the role of cost and quality outcomes in target budget setting and performance measurement, defined population-based and episodic arrangements, and, minimum risk-sharing and savings thresholds as defined in the VBP Roadmap (VBP Levels); and
- Refining additional elements of the model such as provider network integration, data sharing, SDOH, children´s health and long-term care to achieve the intended goals of VBP.
Refining and Strengthening VBP Arrangements
Many VBP arrangements have been built around PCPs despite the comprehensive needs of the attributed population, which warrant broader Provider Networks. Many Medicaid members in VBP arrangements have complex medical needs where community based BH services and/or SUD services are critical to delivering impactful and appropriate care.
The proposed construct of MCOs, providers and VMOs working in concert will support comprehensive integrated primary care, BH, and other public health and social care capacities within VBP arrangements that are necessary to meet the needs of Medicaid members. Although progress has been made, achieving more sophisticated and integrated networks remains an important goal. VBP arrangements built around fully integrated networks that leverage the support of VMOs and SDHNs and include evidence-based and promising outcomes-based interventions, will be better positioned to create a sustaining framework for the system´s optimal healthcare delivery strategies, including evidence-based and promising outcomes-based practices.
There remains significant opportunity to transition MCOs and providers into more progressive risk bearing arrangements, where greater accountability is shared for cost and quality outcomes, and where savings can be maximized. The overarching VBP and VMO performance framework incentivizes MCOs and providers to enter into more meaningful risk bearing arrangements. Maximizing this opportunity will improve quality and efficiency outcomes.
VBP arrangements must evolve to appropriately align provider and CBO networks to the populations they serve and expand rewards and savings (and possibly risk) beyond primary care, including to BH or other specialty providers. Existing arrangements often do not include sufficient methods of rewarding providers or CBO partners with savings for their positive contributions to the outcomes of populations they serve. Allowing additional time and stronger collaboration among health system partners will help generate the models that effectively reward providers beyond primary care.
Data sharing within VBP arrangements remains a major hurdle in structuring effective VBP arrangements and managing performance. For effective VBP contracting and performance, data sharing among MCOs, providers and CBOs must be timely, accurate, and complete. However, these standards have yet to be defined. The creation of VMOs as population-health drivers and partners will strengthen collaboration and improve data analytics capabilities. These strengths will enable a better understanding of population health needs, gaps in care, and opportunities for quality improvement among the attributed population within a provider´s and MCO´s VBP arrangement(s).
Refining and Strengthening Data Sharing Capabilities
The current waiver provided a critical role in triaging and stabilizing the technological and data components of the State´s Medicaid delivery system; this next phase will focus on readying the system for self-management. While the initial waiver brought together behavioral, social, physical, and specialty providers, this clinical transformation towards person-centered care also depended on a technological transformation towards person-centered data. A key component of the workflows in each of the promising practices is technology and data availability, functioning as a trigger for identifying needed intervention, communicating critical handoff instructions, coordinating and tracking team-based activities, evaluating clinical efficacy, and, in some cases, all of the above. The initial waiver placed an unprecedented volume of curated and actionable population health data at providers´ fingertips, and the next phase of this transformation will continue this important work. In order to cement the State´s transition to VBP, this data must be further democratized, entities will need to identify their unique value propositions, and additional data will need to be collected, shared and utilized.
Some components of the State´s Medicaid delivery system significantly evolved their data integration and interoperability efforts during the initial waiver period. The State Office of Health Insurance Programs (OHIP) developed significant upstream capacity in data curation, storage, and distribution, creating a retail environment for access to comprehensive Medicaid claims data. Utilizing its Medicaid Data Warehouse (MDW), the State developed several key performance management support capacities in its Medicaid Analytics and Performance Portal (MAPP). Through MAPP, the State launched a provider network capacity, linked to automated PPS monthly performance attribution. MAPP provided rolling performance snapshots to each PPS (and their downstream partners), displaying progress towards closing annual gaps with a monthly "score" against time-sequenced interim milestones. PPSs received monthly, member-level claims extracts, auto redacted for member opt-out and SUD histories. MAPP also includes other key population health workflow support, including performance support dashboards, rudimentary predictive analytics, and aggregated performance benchmarking.
Building from the information provided through MAPP, PPSs developed state of the art clinical and claims handling capacities to share actionable information with performance partners. Some PPSs developed in-house data integration and analysis platforms, and some also leveraged the State´s network of Qualified Entities (QEs) to help with bidirectional data exchange and supportive analytics. The best in class systems are linking claims, clinical and social data into regionally focused population health support tools, enabling better care for special populations or service needs like OUD and Justice-involved populations.
While the initial waiver enabled significant advances in technology-enabled population health management infrastructure at the State and PPS level, further work is needed to build an interoperable enterprise that places all aspects of patient health data at all points of care. Although QEs played in important role in some regions at supporting the initial waiver´s work through data provisioning, quality measurement, and analytic support, QE involvement represents another practice which showed promise during the initial waiver: the State would like to expand, formalize, and centralize the role of QEs in data distribution during the next waiver period. Additionally, the next waiver period will be marked by increased MCO involvement, as the State seeks to embed these critical care management partners and their advanced in-house capacities in the developing population health management ecosystem.
Whereas the initial waiver´s effort required building capacity, the next waiver period will be defined by increased interoperability, integration, role definition, and workflow management. Confusion around security, privacy policies, permitted data access, data provisioning scope, quality measurement and reporting still exists, and the success of VBP depends on an environment with clearly defined rules. The State looks forward to fostering an environment where each partner can focus on their unique contribution to the technological transformation of care delivery and is planning to define roles accordingly for this next phase.
A concretely defined Statewide data access structure in the next waiver period will utilize the VMOs to more purposefully create regional understanding and utilization of standardized data pathways. In this new structure, the State will forge a more direct relationship with the QEs, as the link to the Statewide HIE, to provision claims data downstream. The State will provide claims data to the QE and the QE will in turn provision this data downstream to VMOs with, when possible, pre-linked, relevant, clinical data. While much more work remains to be done to define specific tasks, QE involvement will create a more purposeful connection between clinical data provisioning and claims data provisioning. This will allow the State to focus on Statewide quality and efficiency measurement and comparative benchmarking for all accountable partners: MCOs, VMOs, HHs, IPAs/ACOs, PCPs and more.
Many lessons have been learned and much feedback has been received on data exchange. Some highlights for focus during the next period include:
- Attribution will be simpler and will align better with MCO enrollment, contracting, and quality programs. More complex forms of attribution break when complicated claims changes are implemented.
- Clearly defined data standards are important for interoperable data exchange. Confusion arises when there is a lack of specific, concrete, and uniform guidance.
- Data security and privacy roles will be clearly defined in advance. While security standards naturally change over time, moving goalposts make it difficult to advance initiatives.
- Performance management for dual-eligible members (duals) requires the connection of Medicare/Medicaid claims information. Duals data is complicated but connecting these data sets will be critical.
- MCOs and QEs will be the source for real-time, standardized pathways for directing care interventions among providers, VMOs, and CBOs. The State has data for benchmarking purposes, but it is not always available timely.
- Social data must be standardized, integrated, and shared to provider truly person-centered care. Tasking QEs, MCOs, VMOs and SDHNs with the job of standardizing and integrating social data will be essential to advance VBP.
- Telehealth requires full optimization of regional IT capacity. The VMOs can provide an essential coordinating function to bridge remaining caps in this critical capacity.
- Data must be expanded beyond hospitals and large physical health providers. Long term care, BH, and other providers must be brought into the data sharing ecosystem for connectivity with other providers by utilizing existing technological pathways.
Each of the promising practices identified earlier depends on actionable patient data; their potential to transform patient care requires that data be interoperable, accessible, and uniform. The next phase of this waiver transformation will seek to build on what´s working in the State´s healthcare technology landscape, improving standardization and role clarity while democratizing access. Each participating entity type will have a clearly defined role, enabling all technological partners to operate at the "top of their license" in the distribution of actionable data. What constitutes patient data will be expanded to include social factors, enabling a truly person-centered model of care. Person-centered care requires person-centered data, and while the initial waiver period produced significant gains in connecting technological workflows, much work is still needed to optimize these promising pathways.
Leveraging an All-Payer Approach to Drive Value
The State´s transformation efforts will carefully consider opportunities to support the construction of regional all-payer payment models that align incentives and interests of individual providers and stakeholders across the region. All payer demonstrations may be supported as integrated components of the State´s healthcare transformation efforts when sufficient payer participation is achieved, and goals are aligned. The proposed VMO Performance Fund and VBP Incentive Fund may support all-payer demonstrations based on regional readiness and aim to address the unique needs of high-risk populations in rural areas and/or underserved higher-risk urban areas.
To date, the State has collaborated with a provider-led entity comprised of primary care, behavioral health providers, hospitals, and other providers across the care continuum in the Adirondack North Country, and CMMI to identify an effective all payer value-oriented payment model that incorporates global budgeting for a provider and multi-payer partnership. The State´s transition toward VBP, and the framework proposed in this waiver, will remain flexible and may readily align attribution and other programmatic elements, including quality measurement and risk thresholds, to support a regional, all-payer payment model.
The next phase of the State´s transition to value-based care stands ready to support innovative and regionally based all payer approaches where value is at the core of healthcare delivery. Aligning payer incentives and establishing innovative payment models will support the State in achieving a sustainable and thriving delivery system that drives higher quality and transitions care to more appropriate settings.
Additional Areas of Focus
Beyond the Promising Practices, the State also identified areas of focus based on high or emerging needs impacting the Medicaid program, particularly in relation to high utilizing and/or vulnerable populations. Therefore, as part of the Waiver Renewal phase of this amendment proposal, the State seeks to enhance provider focus on specific vulnerable subpopulations, sectors, and issues such as children, long-term care, and maternal mortality, as well as continued focus on critical areas of high and emerging need that continue to affect the health of New Yorkers, like opioid and substance use disorders. Specifically, VMOs and their stakeholders will have an opportunity to incorporate interventions that address the following areas of focus:
Children´s Health
Approximately 47% of the State´s children are covered by Medicaid, putting Medicaid in a critical position to advance pediatric and family health. The proposed amendment would extend successful practices to include children in the areas of 1) chronic care management, 2) BH integration, and 3) pediatric-focused patient-centered medical homes, with attention to Adverse Childhood Experiences (ACEs), social determinants, and specific efforts to reach children and families impacted by racial disparities and who face institutional barriers accessing health care services. Social determinants that impact food security, housing stability, and readiness for kindergarten, as examples, are critically important to be recognized and addressed, not only for the child, but also for the caregiver and the family unit in which the child lives. Fostering family resiliency and strengthening protective factors support the Pediatric Vision for Population Health in NY, as recommended by stakeholders.9
A Statewide coalition of child health experts and advocates was convened by the State as part of its First 1000 Days on Medicaid Initiative and was charged with developing a list of ten priority proposals to maximize outcomes and deliver results for the children the State serves. This list includes several recommendations that are well aligned with this Medicaid Waiver application. One of the most significant proposals was to convene a Preventive Pediatric Care Clinical Advisory Group (CAG) to develop a comprehensive report for a vision of pediatric population health in NY, identifying the best strategies to improve care delivery, with the goal of reaching children and families not engaged with a medical home and improving the health of infants, children and adolescents enrolled in the Medicaid program.
- Targeted care transitions and care management. Care transitions and care management for targeted groups have been very successful and would be expanded to serve this population, in collaboration with the Health Homes Serving Children. Further integration of CHWs into provider teams to assist with chronic care management for asthma has also been highly successful and can be replicated and scaled, both for asthma and other conditions critical to children´s health.
- Focus on children with BH needs. For this population, transitional care teams of clinicians and peers bridging psychiatric inpatient to community settings would be deployed. Use of telemedicine for care management of residential populations for ED triage and expansion of crisis stabilization programs would improve management of overall care and minimize avoidable admissions. Children with special health care needs, HIV/AIDS, and end-of- life/palliative care populations are other examples of special populations where collaborative improvement projects could open the door to more robust VBP approaches.
- Infant/Early Childhood Mental Health and Dyadic Therapy. Additional proposals are to develop a braided funding strategy for Infant/Early Childhood Mental Health Consultations and to implement Dyadic Therapy for pediatric populations, addressing maternal and infant health together. These proposals provide the building blocks for the next phase of addressing children´s physical and social/emotional health under Medicaid. The report by the Preventive Pediatric Care CAG and the pilot work that is just beginning in some selected regions in New York provide the vision for Medicaid to address three themes for children´s health in the next phase of care delivery reform: 1) develop a life-course approach by implementing two-generational care, 2) develop a more comprehensive approach to BH Integration in primary care practices for children, and 3) and focus on care of infants, children, and adolescents impacted by the Opioid Crisis.
The two-generational approach:A key first step of the VMOs will be to implement a focused, two-generational approach to address BH needs and the impact of the Opioid Crisis in pediatric populations. The State has already begun to implement post-partum depression screening and referral for treatment as necessary in pediatric practices. Dyadic therapy will also provide a mechanism to enhance the provision and coverage of care for mothers addicted to opioids (as well as other substances) and their children, regardless of whether the child is found to have Neonatal Abstinence Syndrome.
- creates equitable opportunities to reduce racial disparities that focus and address the needs of both children and adults, with the goal of improving the health and well-being of children, families, and ultimately, communities, and
- uses both a holistic lens as well as specific interventions to address the individual needs of children and adults in families.
The Dyadic Therapy approach (as already endorsed and released by CMS) provides a key mechanism for the State´s goal to develop and expand BH integration for pediatric populations, addressing ACEs and social determinants of health. Based on recommendations from the Pediatric Preventive CAG, VMOs will implement the HealthySteps model in pediatric primary care settings across New York to impact children in the first 1000 days of life. "HealthySteps is an evidence-based, interdisciplinary pediatric primary care program that promotes positive parenting and healthy development for babies and toddlers, with an emphasis on families living in low-income communities."10
- IMPACT for children´s populations. The implementation of the Improving Mood–Promoting Access to Collaborative Treatment (IMPACT, or Collaborative Care) Model, which began for adults in New York State in 2015, will be further applied to pediatric populations. The IMPACT model, which originated from the University of Washington in Seattle, integrates depression treatment into primary care and improves physical and social functioning, while cutting the overall cost of providing care. In this model, the behavioral health providers do not necessarily physically integrate into the primary care site. Evidence shows that this minimizes loss to follow up that often occurs with external referrals to specialty care. Collaborative Care also improves efficiency and provider satisfaction in primary care practices. There is a built-in capacity to treat BH, and a dedicated resource to keep track of patient outcomes, which often improve for both behavioral and physical health conditions. The implementation of this model, along with expanding use of Telemedicine/Telepsychiatry, will enhance access to mental health services for affected children and their parents as well as those youth with complex medical conditions and those served through NY´s HH model.
- VBP arrangements supporting children´s health. MCOs and providers need time to implement the children´s VBP arrangement with carefully structured networks that can address the unique needs of children. The comprehensive model of Pediatric Population Health is built on the premise of integrated primary care and BH and accountability for social and environmental factors. This integration is ideally combined with a two generational approach that acknowledges that cost and quality outcomes may be realized over a longer period and across multiple public sector domains. Structuring a specific value-based approach for children is complex and requires more time for stakeholders to structure the arrangement and develop the network that can deliver the care.
The collective efforts of MCOs, providers, VMOs, and SDHNs will support children´s VBP models that are careful to avoid relying entirely on standard efficiency measures, often characterized as cost or expenditure-based measures. Rather, children with complex medical needs and children with "standard" health needs will benefit from access and in many cases, increased care in pediatric and other appropriate specialty care settings. Providers and MCOs must be encouraged to transition care to these settings and empowered with investment to enable impactful care delivery. This approach accounts for efficiency by incorporating other performance indicators that may serve as a proxy for efficiency or unnecessary health care utilization such as Potentially Preventable Admissions (PPAs), Potentially Preventable ED Visits (PPVs) and Potentially Preventable Readmissions (PPRs).
This value-based approach is a deliberate effort to bend the cost curve and to create opportunity to organize a care delivery framework across multiple public sector domains (health, social, education, justice, etc.). As a result, there exists opportunity to develop virtual benchmarks focused on trends rather than historical costs, and which account for multiple public benefit programs to fully understand and realize the benefit of effective and impactful pediatric and family-based care.Long-Term Care
Going forward, the need to more fully incorporate the long-term care (LTC) population into the waiver reforms is critical, marked by the projected growth in this population and their service needs. According to the U.S. Census Bureau, by 2035, senior citizens will outnumber youth for the first time in U.S. history. This is true in New York - by 2025, 18 percent of New York´s population is projected to be age 65 or older, up from 14 percent in 2010. Between 2015 and 2040, the number of adults age 65 and over in New York State is projected to increase by 50 percent, and the number of adults over 85 will double. Both the number and percentage of older New Yorkers is expected to rise further over the next 20 years, driving a likely increase in the number of New Yorkers with cognitive and functional limitations who need LTC services.
Approximately 36 percent of New York´s Medicaid global cap spending for SFY 2019-20 is projected to be in the LTC sector. Medicaid LTC spending has increased from $14.4 billion (gross) in CY 2014 to $19.9 billion (gross) in CY 2018, a 38 percent increase over those five years. In 2018, the dual eligible population (members enrolled in Medicaid and Medicare) accounted for 83 percent of Medicaid long term care spending.
Another key demographic impacting the ability to deliver a continuum of care for the LTC population is the workforce available to deliver community-based services. By 2040, the number of adults between 18 and 64 for every adult over age 85 will drop from 28 to 14. There is a current LTPAC workforce crisis throughout much of the State, and that crisis is projected to deepen over the next twenty years.
In an environment of increasing need, rising costs and workforce shortages, reforms can be achieved by building upon existing promising practices that address LTC workforce issues. VMOs chosen through the waiver will be required to place a considerable focus on practices that bridge acute and post-acute care and expand the best practices to include a component for LTC, both institutional and community-based. The LTC areas of focus include:
- Workforce recruitment and retention remains a top priority. Major demographic shifts in New York have created a workforce crisis. In addition, training for existing workforce is a priority to ensure care coordination and management. Leveraging best practices from the first phase, this waiver will expand upon the following:
- Expanding the use of and/or embedding CHWs, resident assistants and other workforce in locations including senior housing developments. Programs will learn from and expand upon best practices in cross-sector coordination through care management and addressing social needs. They will increase the ability to assess for needed SDOH interventions through funding provided initially by the VMOs but allow successful programs to be included in and paid for through managed LTC MCO value-based arrangements.
- Expanding the use of INTERACT® and other training initiatives to improve quality for the management of acute changes in nursing home resident conditions. In just one illustration of the potential value, a PPS worked with a skilled nursing facility (SNF) to reduce its residents´ ED use and hospital readmissions by developing SNF protocols for common clinical decisions around evaluation, management, and transportation and by implementing more systematic palliative care referrals. As a result of these activities, the SNF´s hospital readmission rate decreased from 31% (in January–March 2018) to 23% (in April–November 2018).
Quality improvement training programs will be funded by the VMOs for a wide range of skilled and non-skilled workers, aiming to reduce avoidable hospitalizations and reduce discharge errors.- Continuing the successful Workforce Investment Programs (WIP). The initial waiver included funding for the WIP as a $245 million investment over three years for the recruitment, retention and training of LTC direct care workforce. Additional funding will be allocated to continue those programs which, through a Department evaluation, are shown to have the greatest outcomes in recruiting, retaining and training LTC workforce. LTC Workforce funding would come from the dedicated workforce pool.
- Developing new Workforce Continuity incentive program in which the VMO would support financial incentive plans for the LTC providers that implement practices to retain workforce. Evidence shows that workforce retention as well as continuity with residents improves quality. The providers would receive longevity payments when they show they have reduced staff turnover.
- Incentives for Providing Integrated Care for Duals. Any strategy for improving the delivery of services to the nearly 800,000 New Yorkers fully eligible for both Medicare and Medicaid must address the current system of bifurcated delivery and financing of health care for these individuals. New York´s dual eligible population are a high need, high cost population and comprise 15 percent of the Medicaid population, accounting for 37 percent of Medicaid spending for CY 2018. CMS and New York are actively working in partnership on the shared goal of providing integrated care for members in both Medicare and Medicaid (dual eligible) and better aligning Medicare and Medicaid service delivery and financing. There is growing evidence supporting the value and benefits of incorporating integrated models in Medicaid programs. Benefits of integrated care include:
Despite these well recognized benefits, fully integrated care for dual eligible individuals in New York, like in most other states, is but a small percentage (4 percent) of those eligible for these programs.
- Improved member experience, quality of life and health outcomes through integrated care management; deeper coordination of care across all services regardless of payer; and improved member experience related to simplifying the process of navigating care across the Medicare primary and acute services and Medicaid long term services and supports (LTSS).
- Program efficiencies achieved by aligning clinical and financial incentives between Medicare and Medicaid, and the provision of integrated, person-centered care planning. Integrated care models provide a significant opportunity to provide a continuum of care that can help rebalance the use of LTSS as a dual eligible member ages and requires more intensive services.
- Opportunities to foster and promote relationships with CMS to identify and initiate shared savings partnerships to reward the State, MCOs, and providers for Medicare savings attributed to Medicaid spending.
We applaud CMS for taking on the effort to promote integration and the flexibility it has already demonstrated. We are already working with CMS to use this flexibility to further refine integrated products, branded in New York as Medicaid Advantage (MA) and Medicaid Advantage Plus (MAP) for those in need of LTC services, using the Medicare D- SNPs as the foundational structure to integrate care. Using this well-established structure, augmented by lessons learned from prior demonstrations including Fully Integrated Duals Advantage (FIDA), makes the most sense and generally has broad support by New York stakeholders. Accordingly, over the course of the next two years, New York will implement a series of steps to transition persons newly dually eligible and those already dually eligible into integrated programs.
However, years of experience across the nation shows that establishing programs and processes alone will not achieve the goal of increasing enrollment in integrated products. Through the new waiver, New York will develop, with stakeholder input, additional investments that will accelerate the adoption of integrated care for duals over a two-year period and as a result transform the system of care for hundreds of thousands of Medicaid consumers. These investments will seek to address barriers that have long stood in the way of integration, incentivize the use of integrated models, incorporate preventive programs in integrated care models that seek to slow the progression toward intensive LTSS guarding against the need for long-term institutional care, and strategically work to align services to reduce overall costs to the benefit of both Medicare and Medicaid.
Among these transformative investments are the following:Waiver funding will also be made available to assist in consolidating the current array of managed long-term care options into integrated MLTC programs tailored to the needs of consumers. Other waiver investments will seek to complement the transition of duals to integrated products including other initiatives such as arrangements between the state Medicaid program and CMS for those individuals who are not enrolled in a Medicare Advantage plan.
- Consumer education strategies that will include, but not be limited to, general education about the benefits of integrated care and direct to consumer messaging to provide tailored information about the value of "one-stop" integrated Medicare and Medicaid coverage to the consumer and their caregivers;
- Education campaigns focused on health care providers that serve dually eligible consumers across the continuum of care, including primary care, LTC, and CBOs as part of the SDHNs established by the waiver; and
- Consumer and provider incentive programs that reward health outcomes and incentivize enrollment in integrated products.
- Reduce Hospital and Nursing Home Admissions and Improve Discharge Planning. Reducing hospital and nursing home admissions is at the forefront of reducing LTC costs. High quality discharge planning reduces readmissions, and can be achieved by:
- Implementation of evidenced based Falls Prevention programs to avoid hospitalizations and nursing home stays and significantly reduce falls over the next four years. Each VMO will be required to invest in a plan to reduce falls by the end of the waiver.
- Leverage VMOs and VBP arrangements to help transition nursing facility residents to the community and provide high quality transition supports and hospital discharge planning for duals (and other Medicaid members). Successful transition models include those that leverage partnerships between CBOs and acute care hospitals, especially those with higher readmission rates.
- Palliative Care/Hospice Care. Increasing access to palliative care programs and hospice for persons with serious illnesses and those at end-of-life can help ensure care and end-of-life planning needs are understood, addressed, and met prior to decisions to seek further aggressive care. Two Promising Practices have emerged that warrant broader replication and scale:
Much education on the role of palliative care and the distinction of palliative care and hospice care still needs to be done among health care practitioners, as well as with Medicaid beneficiaries. These efforts will support palliative care programs already in place in many larger hospitals where care plan decisions can be made, and appropriate post-discharge care planning can be done.
- Palliative Care introduced in primary care settings through the Patient-Centered Medical Home model and;
- Palliative Care administered through nursing homes.
Each VMO will be charged with sponsoring and funding community collaborations around end of life care and advanced planning. Each community in New York is unique and locally tailored evidence-based solutions are necessary. In addition, general statewide measures to be used will be determined by the State.- Improving the LTC/Post-acute care IT Infrastructure. The LTC/post-acute care (LTCPAC) sector was not eligible for federal investments under the HITECH act (i.e., "meaningful use"). As a result, it lags the progress made by other sectors in data collection, analytics and health information exchange, which can hinder the ability to engage in more sophisticated value-based arrangements.
Encouraging the use of Electronic Medical Records (EMR) to engage in QE through incentive payments under the HITECH act has proven effective in improving transitions of care and avoiding unnecessary emergency department visits and hospitalizations. While many of the State´s LTCPAC providers are likely using some form of an EMR, they may not be compatible for information sharing or connected to a network that would transfer data necessary for quality improvement. Incentivizing LTCPAC providers to adopt an EMR and begin to meaningfully engage in HIE will help facilities overcome start-up costs and encourage more meaningful exchange of resident data to ensure better coordination of care, more effective transfers between care settings, and potentially reduce ED visits and unnecessary hospital stays through improved care coordination.
VMOs would be charged with encouraging the LTC providers in their area to invest in IT infrastructure that meets standards developed by the State and generally based on the principles of HITECH including parameters for patient volume, payer source, definitions of meaningful use and system capabilities. Eligible providers could include certified home health care agencies, SNFs, hospices and assisted living programs.Maternal Mortality
In 2016, New York State ranked 30th in the nation for its maternal mortality rate with clear racial disparities. In the State:
- Between 2012-2014, the top five causes of pregnancy-related deaths were embolism (24%), hemorrhage (16%), infection (16%), cardiomyopathy (12%) and hypertensive disorders (7%). Sixty-five percent of the pregnancy-related deaths occurred within a week of the end of pregnancy. Sixty-six percent of the pregnancy-related deaths involved a cesarean section.
- Between 2012-2014, the top five causes of pregnancy-associated but not related deaths were substance use (30%), motor vehicle accidents (22%), suicide (17%), homicide (15%) and cancer (14%).11
- The maternal mortality rate for black women was 51.6 deaths per 100,000 live births, compared to 15.9 deaths per 100,000 live births for white women in 2014-2016. Black women are approximately three times more likely to die than white women.12
In April 2018, Governor Andrew M. Cuomo announced a comprehensive initiative to target maternal mortality and reduce racial disparities in health outcomes. The multi-pronged initiative included efforts to review and better address maternal death and morbidity with a focus on racial disparities, expanding community outreach and taking new actions to increase access to prenatal and perinatal care.
With the State Medicaid program covering 50 percent of the births in the State, Medicaid must be part of the efforts to improve maternal outcomes. As part of the Waiver Renewal period in the proposed amendment, VMOs must develop initiatives to improve maternal outcomes that could include adoption of a maternity care VBP arrangement. These initiatives should:
- Improve access to and attendance at prenatal and postpartum visits, with a focus on prenatal education and social support;
- Address the leading causes of maternal death; and
- Reduce the racial disparities in maternal outcomes.
For these efforts, the VMOs could leverage existing public health projects and/or integrate Promising Practices from the initial waiver (e.g. Centering Pregnancy). The VMOs should also refer to the March 2019 report from the NYS Taskforce on Maternal Mortality and Disparate Racial Outcomes for ideas. This report details ten recommendations to reduce maternal deaths and improve outcomes for women and families of color in NYS.13
Options for VMOs to incorporate into their initiatives include:
- working with CBOs, such as maternal/perinatal infant community health collaboratives, on expanding and enhancing CHW services to address key barriers that impact maternal outcomes;
- implementing the Centering Pregnancy group-based model of prenatal care, which incorporates prenatal education and social support;
- providing universal access to birth preparedness classes, with the intent to improve preparation for labor and delivery as well as improve the connection to providers and health care;
- incorporating the BH needs of women in prenatal and postpartum settings, with a goal to increase screening and treatment for perinatal mood and SUD;
- supporting and incentivizing providers to participate in the State-led Perinatal Quality Collaboratives (PQCs), whose efforts are aimed at reducing pregnancy complications, improving maternal and neonatal outcomes, and reducing racial/ethnic and geographic disparities; and
- promoting diversity in the VMOs´ maternal health provider workforce.
By working to improve maternal health both in the prenatal and postpartum periods, VMOs will help achieve the State´s goal to decrease maternal mortality and reduce racial disparities in health outcomes. VMOs´ efforts will not only benefit mothers across the State, they will also improve the health of their infants as well. This work also supports the State pediatric vision of population health and aligns with the overall goals of this wavier application.
Interim Access Assurance Fund (IAAF) 2.0: Supporting
Critical Safety Net Providers as they EvolveIAAF 2.0 is a critical component of health care reform in New York. The success of the initial waiver in driving down avoidable hospitalizations including readmissions and avoidable ED visits have curtailed revenue for some of the State´s hospitals serving the most vulnerable Medicaid and uninsured patients. This comes at a time when the necessary risk and value–based payment structures are not mature enough to have provided a path for shared savings to at least partially supplant this revenue loss. Many facilities are focusing new resource development on urgent care, ambulatory, and other forms of non–institutional care, but revenue loss on the inpatient side without additional transition funding could serve to permanently destabilize some critical access and essential safety net providers.
In the proposed waiver period for IAAF 2.0, $500M will be made available to provide supplemental payments that exceed upper payment limits, DSH limitations, or State plan payments, to ensure that current trusted and viable Medicaid safety net providers, according to criteria established by the State consistent with agreed–upon Special Terms and Conditions, can fully participate in the transformation without unproductive disruption. The IAAF is authorized as a separate funding structure to support transformation of these facilities to adjust to the new health care environment while maintaining access for Medicaid members.
IAAF 2.0 payments will again be structured to ensure that sufficient numbers and types of providers are available to Medicaid beneficiaries in the geographic area to provide access to care for Medicaid and uninsured individuals while the State continues its transformation path. The IAAF payments shall be limited to providers that serve significant numbers of Medicaid individuals and that the State determines have financial hardship in the form of financial losses or low margins.
In determining the qualifications of a safety net provider for this program and the level of funding to be made available, the State will take into consideration both the number of Medicaid beneficiaries being served and whether the funding is necessary (based on current financial and other information on community need and services) to provide access to Medicaid and uninsured individuals. The State will also seek to ensure that IAAF payments supplement but do not replace other funding sources.
Workforce Flexibility and Investment During Transitions
to New Payment Models and VBPVBP arrangements require providers and payers to continually innovate models of care for quality and efficiency. A trained and engaged workforce is critical to the success of these efforts. In this waiver amendment, VBP efforts will intensify the need for more workforce training that all team members will need in the delivery of care workflows to succeed in VBP implementation.
Many of the initial waiver initiatives that have proven results rely on non-traditional, non- clinical workforce to achieve project goals by helping members better navigate the clinical and social service systems to best meet their unique needs. Regional PPSs and partner collaboratives focused on local gaps in the delivery system and implemented workforce strategies such as community college CHW training courses, training stipends, scholarships, recruitment/retention of needed clinical and non-clinical staff, and building community workforce pipelines to build local employment and capacity. The local collaborations were nimble in mobilizing available community agencies and institutions for workforce training, recruitment, and placement in relatively short timeframes to impact performance at provider program sites and address critical workforce shortages.
These efforts also strengthened economic development and sustainability in many communities by creating new employment opportunities and career ladders for people without college degrees for roles as CHWs, peer advocates and navigators. PPSs reported significant demand for the training and hiring of "transformation titles" over the course of the initial waiver that encompassed care coordination and care management as primary functions both in clinical and non-clinical positions. Additional educational opportunities for career advancement were also initiated, such as courses for certified nursing assistants for LPN certification. These were supported by stipends and other assistance to remove barriers. Ongoing trainings have been and will be critical to re-orient and engage all members of the care delivery staff in the design and implementation of patient-centered integrated care, value-based models and workflow changes to care for patients differently and effectively. Examples of key trainings are in areas of motivational interviewing, cultural competency/health literacy, care coordination, applicable Evidence-based Protocols and Rapid Cycle Continuous Improvement. These efforts should continue through the VMOs.
The VMOs should continue workforce investments in the "transformation titles" and their expansion to the additional high priority areas of children, including such roles as youth and family peer advocates. These positions have facilitated greater access to providers, improved patient self-management abilities through support, and helped increase the capacity of the clinical teams by addressing many of the non-medical issues in timely and culturally competent ways. Continuous support and training are required for this valuable workforce segment to ensure retention and maintain skillsets.
The VMOs will require ongoing flexibility to use earned dollars to support non-clinical workforce as they work with the MCOs, providers and CBOs to design VBP approaches that support these value-adding team members for the long-term. Required workforce-related planning and reporting in the extension period would focus on the data that all partners, including community-based partners, would need to assess intervention costs and savings for purposes of future VBP. The VMOs should continue to assess and invest in local workforce needs to fuel innovative approaches and improve outcomes. A portion of the VBP incentive payment could be based on integration of non-traditional workforce into higher-level VBP arrangements.
VMOs will be required to develop and submit a comprehensive workforce workplan tied to the promising practices and priority areas for VBP arrangements to identify the skillsets, and available labor resources and training programs. The workplan should identify the promising practice and priority areas, what gaps exist and strategies to address the gaps as well as other strategies to enhance the skillsets and engagement of the workforce to successfully implement the value-based models of care.
Section III – Demonstration Evaluation and Hypotheses
Phase 1 Waiver Extension Demonstration Evaluation Plan and Hypotheses
The extension will follow the evaluation plan in the original waiver for an additional year, continuing to test the components identified in the current evaluation plan. It will also adhere to the hypotheses established in the existing evaluation plan.
The Original Evaluation Design includes research questions and hypotheses as core components. This includes a statement of the specific research questions and testable hypotheses that address the goals of the demonstration, including:
- safety net system transformation at both the system and state level;
- accountability for reducing avoidable hospital use and improvements in other health and public health measures at both the system and state level; and
- efforts to ensure sustainability of transformation of/in the managed care environment at the state level.
By extending our waiver by one year the evaluation design for this extension will focus on research questions pertaining specifically to the accountability for reducing avoidable hospital use and improvements in other health and public health measures at both the system and state level. Extending the waiver will allow NYS to collectively achieve our goal of reducing avoidable hospitalizations by 25% and continue to leverage improvements in care from Year 3 and Year 4 incentives when project implementation matures to meet the needs of pay-for-performance (P4P) based accountability. The research questions, hypotheses, data source, and evaluation design are outlined below (Exhibit 5).
Exhibit 5: Waiver Extension Demonstration Hypotheses
Research Question Hypothesis Anticipated Measure(s) Data Sources Evaluation Approach Did health care quality improve because of clinical improvements in the treatment of selected diseases and conditions? Health care quality will increase in the following areas:
- behavioral health,
- cardiovascular health,
- diabetes care,
- asthma,
- HIV/AIDS,
- perinatal care, and
- palliative care.
- Adherence to Antipsychotic Medications for People with Schizophrenia
- Follow-up after hospitalization for Mental IllnessControlling High Blood Pressure
- Comprehensive Diabetes Care-Hemoglobin A1c (HbA1c) Poor Control (>9.0%)
- Asthma Medication Ratio
- Medication Management for People with Asthma
- Viral Load Suppression
- Prenatal and Postpartum Care
- Palliative Care
Medicaid Claims and Encounters
Electronic Clinical DataDescriptive statistics
Interrupted Time Series AnalysisDid utilization of behavioral health care services increase as a result of the VMO program? Behavioral health care service utilization will increase.
- Follow-up after hospitalization for Mental Illness
- Initiation and Engagement of Alcohol and Other Drug Dependence Treatment)
Medicaid Claims and Encounters Descriptive statistics
Interrupted Time Series AnalysisWas avoidable hospital utilization reduced as a result of the VMO program? Avoidable hospital utilization will decrease.
- Potentially Avoidable Readmissions
- Potentially Avoidable Emergency Room Visits
Medicaid Claims and Encounters Descriptive statistics
Interrupted Time Series AnalysisPhase 2 Waiver Renewal Demonstration Evaluation Plan
The State intends to contract with an independent evaluator to develop and execute a plan for evaluating the demonstration proposal, specifically the hypotheses indicated below. In consultation with the independent evaluator, the State will design an evaluation plan that:
- Identifies validated performance measures that assess the impact of the demonstration, in general and on beneficiaries;
- Identifies meaningful comparison group, as relevant to specific interventions; and
- Includes an evaluation budget.
It is the intent of the State to follow all CMS evaluation design guidance in working with the State´s independent evaluator to draft and execute the evaluation plan.
Furthermore, the State will conduct ongoing monitoring of this demonstration. The State intends to provide information regarding such monitoring activities in the required quarterly and annual monitoring reports.
Phase 2 Waiver Renewal Demonstration Hypotheses
The State intends to test the hypotheses identified in Exhibit 6 during the Phase 2 demonstration period. Please note that these hypotheses will utilize the same evaluation approach – The independent evaluator will design quantitative and qualitative measures to include quasi-experimental comparisons.
Exhibit 6 Phase 2 Demonstration Hypotheses
Hypothesis Anticipated Measure(s) Data Sources Evaluation Approach Increase the number and type (episode, subpopulation) of VBP arrangements in NY and strengthen collaboration of providers, MCOs, and social service providers/CBOs by establishing regional networks known as Value Management Organizations (VMOs)
- Number of new or enhanced VBP contracts among VMO-affiliated MCOs and providers
- VMO support agreements as part of VBP arrangements
Managed Care Contract Database Descriptive statistics Through VBP arrangements with VMOs and MCOs, SDHNs will improve collaboration and participation of social service providers in VBP arrangements and increase the availability of social care interventions.
- Number of new interventions/workflows implemented
- Increase in number of referrals to community-based providers
SDHN referral tracking system Independent evaluator will design quantitative and qualitative measures to include quasi-experimental comparisons Addressing both clinical improvements and non-clinical factors of care will reduce avoidable healthcare utilization; improve health outcomes; and improve quality of life for vulnerable populations, such as children, long-term care members, and members with opioid use disorder.
- Performance measures (See Table 3 and 4)
Medicaid Claims and Encounters
Electronic Clinical DataInterrupted time series
Section IV – Demonstration Eligibility, Benefits and Cost-Sharing
This proposed demonstration does not change, affect or modify the State´s current Medicaid and/or CHIP programs outside for any of the above components. Existing eligibility standards, benefits, cost-sharing and delivery systems established in the New York State plan are anticipated to stay the same during both extension and renewal.
Section V – Delivery System
This renewal, during Phase II, drives evolution of existing Medicaid delivery systems to incorporate:
- Value Management Organizations (VMOs) that will serve as a performance and population health driver across the continuum of care, linking managed care with clinical and SDOH providers that serve the same Medicaid member
- Social Determinant of Health Networks (SDHNs) that will organize SDOH providers and CBOs into networks needed to provide stabilizing support and services to Medicaid members in the community, reducing overall health care cost
VMOs and SDHNs are two critical entities that support delivery of value-based care under an anticipated risk sharing environment established by the end of the proposed demonstration period to progress and increase the number of Medicaid providers in risk contracts. The role of VMOs and SDHNs are described further below and as part of Section II.
Value Management Organizations (VMOs)
Role: The State envisions that the VMO will be constituted as a legal entity (e.g., not-for-profit corporation, limited liability company, etc.), which may be either newly formed or modified from an existing PPS structure under the original waiver to include a network that, at a minimum, is composed of providers, MCOs, and CBOs as part of the governance, management and operational structure of the VMO. Additionally, the QEs would also be integrated into the
VMOs and their collaborative partnerships, either formally through their governance and/or through the provision of services to assist in sustaining and enhancing the VMO participants´ bidirectional data exchange capabilities. VMOs must be legally organized in a way that permits the VMO to contract with, and receive funds from, the State, such that VMOs can then distribute these funds as part of downstream agreements with participants in connection with achievement of, and payment for, programmatic objectives and measures built around better health outcomes.
Governance: VMOs will reflect their governance structure in organizational documents, which will include the establishment of a governing body and sub-committees with voting members that are representative of their participants and will coordinate VMO programmatic objectives. The roles of each participant must be reflective of the VMO´s purposes to both replicate and scale the Promising Practices and achieve VBP readiness and VMO governance must include representatives from each provider type (including but not limited to health systems, physicians, BH, LTC, and children), MCOs, local departments of health and public health, and SDHN/CBOs that are capable of reviewing efforts and investments necessary to improve regional or sub-population performance (e.g., primary care, BH, LTC, etc.). Additionally, the governance body of the VMO must include Medicaid members in a voting capacity.
Exhibit 7: VMO Performance Pool Funds Distribution and Legal Structure
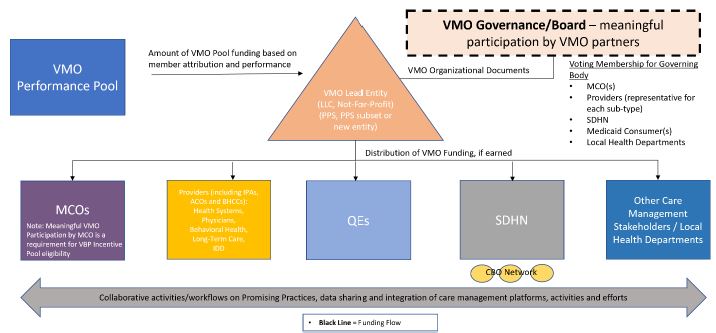
Attribution for Valuation: To ensure equity and accountability, the State proposes using an attribution methodology to allocate available waiver funds under this pool based on valuation and performance. Attribution to each VMO would be based on historical utilization using a care management hierarchy, but would be prospectively fixed for a given measurement period.
Funding: The first portion of the waiver funds will be awarded directly to VMOs selected by the State based on the following criteria:
- Medicaid member attribution;
- History of performance improvement by their participants in the VMO;
- The strength of provider, MCO and CBOs alliances;
- The inclusive nature of the governance structure that includes a range of providers (e.g., primary care, BH, acute care, LTC, etc.), MCOs, and CBOs in executive steerage; and
- Importantly, the potential to sustain the selected Promising Practices under VBP arrangements.
The size of the award available to each VMO will vary by the number of attributed Medicaid member lives to the VMO and the performance of the VMO in achieving programmatic goals for their attributed members, similar to the original waiver.
Social Determinant of Health Networks (SDHNs)
Role: SDHN lead entities will work to integrate social care into the population health work of the VMO. The SDHN lead entities will be a party to VBP negotiations as the system matures into a VBP environment. The lead entity of the SDHN will develop, contract with, and manage the network of participating CBOs that will deliver social determinant of health (SDOH) services. SDHNs will also monitor and track SDOH services and report on metrics for rapid cycle improvement so the State can make any necessary mid-course adjustments. While this does not preclude the opportunity for MCOs or providers to directly contract with individual CBOs, it will provide a more resourced, organized, vetted, and regionally accountable pathway.
The SDHNs can choose to participate in risk-bearing VBP arrangements with MCOs and VBP contractors. SDHNs may also perform social risk support for members referred from a MCO, provider, or the VMO.
Governance: SDHNs must demonstrate that they have enough capacity to serve their region and must incorporate all five service domains into their network: housing instability; transportation; food insecurity; interpersonal safety; and toxic stress. SDHNs will work with their community partners including but not limited to: MCOs, VMOs, PPSs, Continuum of Care (COC) and BHCCs, HHs, IPAs, ACOs, and health care providers including PCPs, clinics and health systems. The governance of SDHNs must include full voting representation from the five service domains, and should also include representatives from local government representing social service programs, local departments of health and public health and representatives from the local VMO(s) in capacities sufficient to ensure coordination between the two entities.
Engagement with MCOs and VMOs: Referrals of Medicaid members may come from MCOs, VMOs or providers. SDHNs are anticipated to work with VMOs to develop infrastructure and workflows that reduce barriers and allow providers serving the same patient to better co- manage and coordinate services and interventions, thereby reducing patient barriers to services and increasing efficiency across providers. VMOs will engage SDHNs in local learning collaboratives and work jointly on quality improvement projects targeting priority populations identified previously.
Funding: MCOs have an ability to fund SDOH services outside of the medical loss portion of their premium and will work with the SDHNs to identify services that will improve health outcomes and decrease medical expenses. SDHNs have an option of taking on upside and downside risk in VBP arrangements. The State will engage with the VMO, MCO and SDHN providers on the establishment of phased funding goals that begin to measure the percent of Medicaid funds that are spent on SDOH services, which may factor into future targets on the percent of Medical Loss Ratio (MLR) as a percent of total premium that can be carried as either health care quality improvement activity or direct clinical intervention spending.
Funding will provide for both capacity building of the SDHNs and payment of services to the MCOs. Funding for capacity building would flow from the State and payment for services will be funded from MCOs or VMOs, depending on the SDHN activity, to the SDHNs for the following efforts:
- Coordination with the VMO and its partners;
- Integration of health and human services for VBP;
- Formal organization of CBOs to perform SDOH interventions;
- Coordination of a regional referral network with multiple CBOs, VMO, QEs, MCOs and health systems;
- Creation of a single point of contracting for VBP SDH arrangements including review and oversight of existing Medicaid SDOH contracts;
- Assessment of Medicaid Members for the key State–selected SDH issues and appropriate referrals based on need; and
- Representation of CBOs in the VMO.
Impact: The SDHN will provide an organized system of assessment to proactively screen attributed population for social risk factors that negatively impact health outcomes. Referrals will be made to members of the network and appropriate services will be delivered. IT infrastructure overlay will provide a closed-loop referral process and reporting mechanism. Outcomes of referrals will be shared with referring source (VMO, MCO) to ensure comprehensive and coordinated care. By employing evidence-based SDOH interventions the system will recognize the following: decreased unnecessary inpatient and ED admissions; increased patient engagement; and decreased avoidable institutionalization. The SDHN will also coordinate with existing State funded infrastructures and resources including arrangements with CBOs that have established trusted relationships with over 70% of individuals who enroll or renew in Medicaid through the State´s health insurance marketplace.
Funding Methodology for Value Based Payment
While this proposal does not change the payments made through MCOs for the purpose of providing and paying for services, the State proposes a portion of incentive funds be made through MCOs. This incentive payment opportunity is important to support the incorporation of funding key population health and SDOH infrastructure into plan networks and to build plan contracting capacity to fund key value-driving infrastructure that provides broad benefits across their provider network. To achieve this goal, the State proposes development of a VBP Incentive Pool and Network Accountability Fund as described below:
VBP Incentive Pool
A portion of the waiver funds will be awarded directly to VMO-participating MCOs to be leveraged within VBP arrangements and shared with providers which enter into or significantly enhance qualifying VBP arrangements with VMO-affiliated participants.
The State will designate a maximum amount of funding for each MCO based on member attribution, but the actual amount earned by each MCO in the fund will depend upon its contracting for "eligible" VBP agreements (or amendments) with VMO-affiliated participants, based on the criteria specified below (each, an Eligible VBP Agreement). Part of the VBP Incentive Pool will be paid each year to qualifying MCOs, and it is anticipated that much of the funding would be front-loaded, to the extent possible, to incentivize contracting during earlier performance years and given the multi-year nature of VBP agreements. This fund is envisioned to be "use-it-or-lose-it," with dollars not earned by a particular MCO repurposed for future performance years, reallocated to reward the highest performers, or surrendered entirely.
MCOs will earn funds set aside in the VBP Incentive Pool based on each new or amended Eligible VBP Agreement, but amounts earned will be prioritized to reflect the underlying sophistication of the Eligible VBP Agreement, based on features and timing of the specific Eligible VBP Agreement, as delineated below. MCOs could also earn funds from the VBP Incentive Pool based on aggregated measures, such as attainment of a target rate of VBP contracts or percentage-based improvements in the rate of an MCO´s VBP contracting efforts. Distribution of these funds are depicted in Exhibit 8: VMO Incentive Pool Funds Distribution below.
Exhibit 8: VMO Incentive Pool Funds Distribution
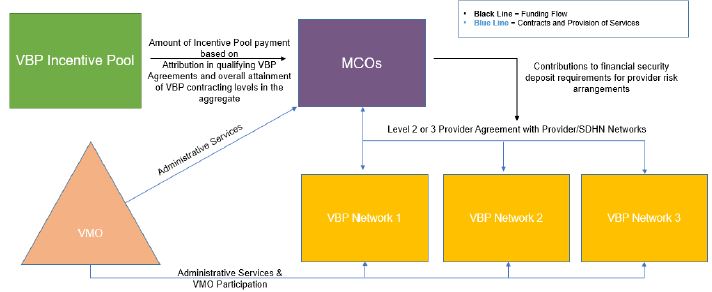
Eligible VBP Agreements
The eligibility to access VBP incentive award dollars will be performance-based in that their receipt is conditioned on the MCOs and the providers/Provider Networks achieving certain qualifying criteria:
- Meaningful Participation in VMOs. To be eligible for receipt of a VBP Incentive Award, MCOs must participate meaningfully in one or more VMOs serving any region in which the MCOs have material enrollment. Meaningful participation will entail having an active role in the governance and executive steerage of the VMO, sharing data among the VMO participants, and active involvement in VMO initiatives that further the Promising Practices and other population health initiatives.
- Qualifying VBP Arrangement. Consistent with the Department of Health´s Provider Contract Guidelines for Article 44 MCOs, IPAs, and ACOs , the jointly negotiated provider agreement (or an amendment to an existing provider agreement) that contains a qualifying VBP arrangement will be submitted by the MCO to the State.14 A qualifying VBP arrangement must have the following components:
- Risk Arrangement. The payment terms involve VBP Level 2 or greater risk, based on the most recent version of the CMS approved New York State Roadmap for Medicaid Payment Reform (VBP Roadmap), that implements, refines, or relates to one or more Promising Practices or initiatives of the VMO.
- Network Composition. The provider or Provider Network included within the VBP arrangement with the MCO (the Value Network) is appropriately inclusive of VMO-affiliated providers and is composed to adequately address the needs of the members in the VBP arrangement, as informed by prior VMO initiatives. The State will work with the VBP Workgroup, including VMOs to establish the adequacy criteria and composition for each VBP provider network based on the nature of the VBP arrangement.
- Data-Sharing Requirements. The VBP arrangement will satisfy a minimum level of data exchange requirements so that both the MCO and the Provider Network is capable of monitoring performance based on health outcomes and cost.
- Quality Reporting. The VBP arrangement will use quality measures and require quality measure reporting consistent with waiver goals and VMO priorities for the target population.
- Financial Risk Management. The MCO and the Value Network will address how the VBP arrangement will satisfy financial security deposit requirements under applicable rules, including 10 NYCRR Part 98 and New York State Department of Financial Services Regulation 164. Proposed strategies may include using a portion of the VBP Incentive Award to fund the financial security deposit requirements directly or through other risk-mitigation mechanisms approved by the Department of Health and/or Department of Financial Services, as applicable.
- VMO Support Services Agreement. Before the end of the waiver, the MCO and/or the provider/Provider Network will enter into an administrative or management services agreement with the VMO to support aspects of the VBP arrangement that build on the capacity, competencies and infrastructure of the VMO, which may include referral linkages, data exchange, and data reporting.
Evaluation of Eligible VBP Agreements
The VBP Incentive Pool will be divided among the regions and MCOs in the regions. MCOs can then earn a VBP Incentive Award upon approval of an Eligible VBP Agreement; however, the size of the VBP Incentive Award for a particular Eligible VBP Agreement will vary depending on how well the VBP arrangement aligns with the goals of demonstration, the Promising Practices, its ability to achieve cost and quality outcomes, and the number of eligible awards earned in a region.
Accordingly, criteria used to score and size a VBP arrangement, which will inform the size of the VBP Incentive Pool award, may include:
- Attribution Size - Size of the VBP arrangement, as measured by the attribution of Medicaid members to the VBP agreement;
- Level of Risk - Higher risk arrangements (e.g., Level 3) will be scored more highly;
- Network Composition - inclusiveness of the VBP provider network being proposed to participate in the VBP arrangement, and the overlap in composition with the non-MCO participants in the VMO;
- Safety Net Providers - The inclusion of historical and/or financially distressed safety net providers;
- Timing - The speed at which MCOs and Provider Networks can leverage the work of the VMO to receive approval for a VBP arrangement, as compared to other networks; and
Adoption of Cost and Outcome Measures - Adoption of quality and cost outcome measures, and potentially more progressive measures, that build on the goals and objectives of the demonstration and the State, including those recommended by the VBP Workgroup and VBP CAGs.VMO Performance Pool
The VMO Performance Pool is designed primarily to fund investments in population health and infrastructure required to further the Promising Practices and related population health initiatives. The VMO Performance Pool will be distributed directly to
VMOs based on their adoption of proven strategies for population health management and continued population health improvement through quality measurement.
The VMO Performance Pool will be divided into two accountability funds: (1) the Network Accountability fund; and (2) the Regional Accountability fund. The purpose of these funds is to ensure that each VMO is appropriately incentivized to promote population health efforts that support outcomes for both their attributed member populations and the collective regional Medicaid population, regardless of attribution. The pools and funds are re-depicted below from Exhibit 4: VMO Performance Pool Funds Distribution and Legal Structure below.
Exhibit 4 (re-depicted): Proposed Funding Pools (not inclusive of IAAF or Workforce Development Funds)
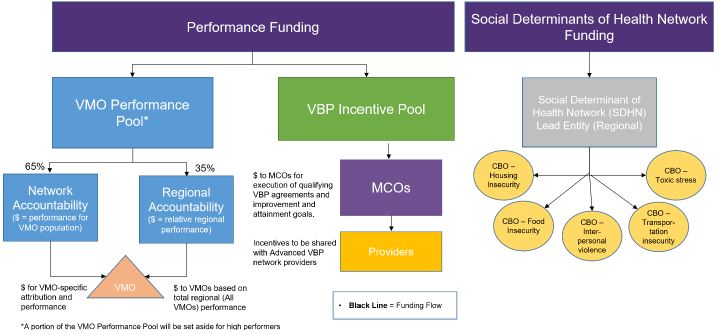
Network Accountability Fund
The Network Accountability Fund (approximately 65% of the total VMO Performance Pool) will reward individual VMOs for adoption of proven population health strategies, built on the Promising Practices, and will measure results within their attributed member population. A maximum amount of funding per VMO will be determined based on member attribution and associated valuation, but the amount each VMO actually earns from the VMO Performance Pool will be based on adoption of the Promising Practices and results measured among their attributed members.
Awards from this Network Accountability fund will be made each performance year, but will be "use-it-or-lose-it," such that any available funds not earned by a particular VMO in a particular performance year would be repurposed for future performance years, reallocated to the regional accountability fund, reallocated to reward the highest performers, or surrendered entirely.
Measurement of award amount will be structured such that VMOs are rewarded in at least two categories: (a) implementation of Promising Practices ideally shared among a broad group of VMO participants, such as those related to population health management infrastructure, data analytics capabilities, data sharing, shared services, etc.; and (b) calculated performance measure results that would reward measure improvement as well as attainment.
The Regional Accountability Fund
The Regional Accountability Fund (approximately 35% of the total VMO Performance Pool) will reward all VMOs with meaningful attribution in a region (minimum member count or percentage) based upon measure results within that region, regardless of attribution to a specific VMO. Specific targets for attainment and improvement are expected to be different for different regions. Unlike the Network Accountability fund, this fund will have a designated amount set aside per year, which would be fully liquidated along a bell curve, with the higher- performing regions receiving more. It is expected that regions might need to be unequally weighted to avoid drawing all efforts to regions with higher populations.
Performance Measurement
Overview Waiver Extension (Phase One) MY 6: 2020-2021
Each PPS has employed multiple projects both to transform health care delivery as well as to address the broad needs of the population that the performing provider system serves. These projects were grouped into different strategies, such as behavioral health, within each Domain (System Transformation Projects (Domain 2), Clinical Improvement Projects (Domain 3), and Population-wide Projects (Domain 4). To move from the current project-based performance measurement system to a Total Care for the General Population VBP arrangement in Phase 1, the waiver extension will involve removing certain domains and aligning performance measures with the NYS VBP Roadmap. The focus will be on Pay for Performance (P4P) measures. Domain 1 measures will be removed as projects have been fully implemented, and while system transformation goals have largely been met, some measures of system transformation will be maintained, specifically Potentially Preventable Emergency Department Visits (PPVs) and Potentially Preventable Readmissions (PPRs). Domain 3 clinical improvement project measures will be maintained, and Domain 4 Population-wide pay-for- reporting (P4R) measures will be removed (Exhibit 9).
Exhibit 9 – Waiver Extension (Phase 1) Performing Provider Systems´ Measure Reporting Responsibilities
Domain Current Waiver MY 0-5 Extension Waiver (Phase 1) Domain 1 Overall Project Progress Removed Domain 2 System Transformation Removed except for PPV and PPR Measures Domain 3 Clinical Improvement Maintained Domain 4 Population-wide Removed Performance in Measurement Year – or the Waiver Extension period – will be evaluated using the approved gap-to-goal methodology. As noted previously, 80% of performance dollars will be used for regular performance and 20% for high performance, with both based on scaled, tiered performance paid on a Per Member Per Month (PMPM) basis, established after the close of performance. The waiver extension measurement year will focus on P4P measures in the previous waiver demonstration that have not topped out their performance. The only P4R measures that will be included will be those previously non-claims-based P4P measures whose data will now come from the health information exchanges and other electronic data sources rather than from medical record chases/reviews.
The set of metrics that the PPSs will be responsible for will remain the same for wavier extension measurement year for the projects within the strategy. However, current waiver MY5 P4R measures and those measures not aligned with the Total Care for General Population VBP measure set will be removed. Measures that are collected using the C&G CAHPS Survey will also be removed, as performance on these measures has topped out. Measures which require information from medical records will be collected using electronic clinical data available from the QEs and PPSs electronic health records. These new data sources will involve resetting the PPS measure result baseline, hence four measures using electronic clinical data will move to P4R in the wavier extension measurement year to accommodate the new reporting mechanism. No new measures will be added. Exhibit 10 shows all the performance measures that will be evaluated in the waiver extension.
Exhibit 10. Waiver Extension Performance Measures
Measure Name Steward and Specification Version NQF # Projects Associated with Measure Data Source Payment: Demonstration Year 5 Payment: Demonstration Year 6 DY 6 Potentially Preventable Emergency Room Visits (PPV) ± 3M NA 2.a.i – 2.a.v,
2.b.i – 2.b.ix,
2.c.i – 2.c.iiClaims P4P P4P Potentially Preventable Readmissions (PPR) ± 3M NA 2.a.i – 2.a.v,
2.b.i – 2.b.ix,
2.c.i – 2.c.iiClaims P4P P4P Antidepressant Medication Management – Effective Acute Phase Treatment HEDIS® 2020 0105 3.a.i – 3.a.iv Claims P4P P4P Antidepressant Medication Management – Effective Continuation Phase Treatment HEDIS® 2020 0105 3.a.i – 3.a.iv Claims P4P P4P Diabetes Screening for People with Schizophrenia or Bipolar Disease who are Using Antipsychotic Medication HEDIS® 2020 1932 3.a.i – 3.a.iv Claims P4P P4P Follow-up after hospitalization for Mental Illness – within 7 days HEDIS® 2020 0576 3.a.i – 3.a.iv Claims P4P P4P Follow-up after hospitalization for Mental Illness – within 30 days HEDIS® 2020 0576 3.a.i – 3.a.iv Claims P4P P4P Screening for Clinical Depression and follow-up NYS-specific NA 3.a.i – 3.a.iv Electronic Clinical Data P4P P4R Adherence to Antipsychotic Medications for People with Schizophrenia HEDIS® 2020 1879 3.a.i – 3.a.iv Claims P4P P4P Initiation of Alcohol and Other Drug Dependence Treatment (1 visit within 14 days) HEDIS® 2020 0004 3.a.i – 3.a.iv Claims P4P P4P Engagement of Alcohol and Other Drug Dependence Treatment (Initiation and 2 visits within 48 days) HEDIS® 2020 0004 3.a.i – 3.a.iv Claims P4P P4P Antipsychotic Use for Persons with Dementia ± Pharmacy Quality Alliance MDS 3.0 NA 3.a.v MDS P4P P4P Percent of Long Stay Residents who have Depressive Symptoms ± MDS 3.0 Measure #0690 NA 3.a.v MDS P4P P4P Controlling High Blood Pressure HEDIS® 2020 0018 3.b.i – 3.b.ii, 3.h.i Electronic Clinical Data P4P P4R Comprehensive Diabetes screening – All Three Tests (HbA1c, dilated eye exam, and medical attention for nephropathy) HEDIS® 2020 0055, 0062, 0057 3.c.i – 3.c.ii, 3.h.i Electronic Clinical Data P4P P4R Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Poor Control (>9.0%) ± HEDIS® 2020 0059 3.c.i – 3.c.ii, 3.h.i Electronic Clinical Data P4R P4P Pediatric Quality Indicator # 14 (Asthma Admission Rate) +/- AHRQ 2018 0728 3.d.i – 3.d.iii Claims P4P P4P Asthma Medication Ratio (5 – 64 Years) HEDIS® 2020 1800 3.d.i – 3.d.iii Claims P4P P4P Medication Management for People with Asthma (5 – 64 Years) – 50% of Treatment Days Covered HEDIS® 2020 1799 3.d.i – 3.d.iii Claims P4P P4P Medication Management for People with Asthma (5 – 64 Years) – 75% of Treatment Days Covered HEDIS® 2020 1799 3.d.i – 3.d.iii Claims P4P P4P Cervical Cancer Screening HEDIS® 2020 0032 3.e.i Claims P4R P4P Chlamydia Screening (16 – 24 Years) HEDIS® 2020 0033 3.e.i Claims P4P P4P Viral Load Suppression NYS-specific NA 3.e.i Electronic Clinical Data P4P P4R Prenatal and Postpartum Care— Timeliness of Prenatal Care HEDIS® 2020 1517 3.f.i Electronic Clinical Data P4R P4P Prenatal and Postpartum Care— Postpartum Visits HEDIS® 2020 1517 3.f.i Electronic Clinical Data P4R P4P Well Care Visits in the first 15 months (5 or more Visits) HEDIS® 2020 1392 3.f.i Claims P4R P4P Childhood Immunization Status (Combination 3 – 4313314) HEDIS® 2020 0038 3.f.i Electronic Clinical Data P4R P4P Percentage of patients indicating need who were offered or provided an intervention for pain symptoms experienced during the past week NA NA 3.g.i – 3.g.ii Non-claims P4R P4P Percentage of patients indicating need who were offered or provided an intervention for physical symptoms (other than pain) experienced during the past week NA NA 3.g.i – 3.g.ii Non-claims P4R P4P Percentage of patients indicating need who were offered or provided an intervention for not feeling at peace during the past week NA NA 3.g.i – 3.g.ii Non-claims P4R P4P Percentage of patients indicating need who were offered or provided an intervention for depressive feelings experienced during the past week NA NA 3.g.i – 3.g.ii Non-claims P4R P4P Percentage of patients who were offered or provided an intervention when there was no advance directive in place NA NA 3.g.i – 3.g.ii Non-claims P4R P4P Overview Waiver Renewal (Phase 2) MY 1-3: 2021-2024
Throughout the Phase Two renewal demonstration years, VMOs will be evaluated using specific quality measures that align with the State Medicaid program´s Total Care for the General
Population VBP measure set. This section describes the measure domains and the methodology for establishing goals and annual improvement increments that will be used to determine performance attainment in each demonstration year. The demonstration will focus primarily on P4P measures, except in the few instances where measure development work is still needed, such as with Developmental Screening in the First Three Years of Life and measures of social determinants.
Measures will focus on six (6) domains:
- Primary Care,
- Children´s,
- Behavioral Health,
- Substance Use Disorder (SUD),
- HIV/AIDS, and
- Maternal Health (Exhibit 11).
These measures align well with screening and prevention as well as chronic disease management aspects of primary care. P4P measures specific to children, pregnant women, and HIV/AIDs populations are also included, since these population are a focus in the State Medicaid program. Outcome measures are emphasized across these domains where they exist. For example, for those with HIV infection or AIDS, viral load suppression is the premier outcome measure.
Two additional domains will focus on: 1) Palliative and Hospice Care, and 2) Long-term Care measures that look at potentially avoidable hospitalizations and nursing facility level of care scores (Exhibit 12). The Nursing Facility Level of Care (NFLOC) score is only for Managed LTC members, not for the nursing home population. It evaluates how well the plan does in maintaining stability (or improving) the members Activities of Daily Living function, cognition, continence, and behavioral issues.15
Population-based utilization measures from 3M´s suite of Potentially Preventable Events will include Potentially Avoidable Admissions (PPAs), Potentially Avoidable Emergency Room Visits (PPVs), and Potentially Avoidable Readmissions (PPRs) (Exhibit 11). An efficiency measure for total cost of care will examine the actual costs versus the expected costs of care. Measures of social determinants to include Kindergarten Readiness, Food Insecurity, and Housing Stability will be explored for pay-for-reporting (P4R) purposes (Exhibit 12). There is no single standard across states for these measures of social determinants and as such, work will involve developing an approach to collecting the standardized data needed to populate quality measures, as well as the measurement development process. These measures of social determinants align with CMMI´s Integrated Care for Kids Notice of Funding Opportunity.
Clinician & Group Survey (CG-CAHPS) will not be used in this phase as these measures topped out in the State Medicaid population in the current waiver. Patient-reported outcome measures will be explored as an alternative.
Methodology for Establishing Performance Goals, Annual Improvement Targets, and High Performance
Measurement Period
The measurement year for the wavier extension period will be reset to align with managed care plan reporting requirements. The measurement year will run January to December 31 as opposed July to June as was done in the prior demonstration.
Performance Goals
Performance goals are intended to reflect the best performance expected in New York State and the performance goals are the same, consistently applied to all VMOs each year. The performance goal for each measure will not be changed throughout the demonstration. Due to the inclusion of new performance measures and new data sources for existing measures, the performance goals for each measure will be set using the first measurement year VMO results. The performance goals will be established by using VMO results from measurement year 1 and adjusting the best performing baseline result by 20% lower or higher depending on whether a lower or higher result is desirable. If the measure specifications are changed to the degree that prior results are not comparable, CMS and the State have established a process for resetting performance goals. LTC measures are sourced used NYS SPARCS data and the Uniform Assessment System (UAS) for MLTC members. Sources of data are still be explored for Palliative and Hospice Care, Kindergarten readiness, food insecurity and housing instability.
Annual Improvement Targets (AITs)
Annual improvement targets (AITs) for measures in the Renewal Phase Two for a VMO will be established using the methodology of reducing the gap to the goal by some percentage to earn the achievement value. As more data and analyses are reviewed from the initial waiver, multiple factors appear to affect PPS performance, including number of lives, complexity, and geographic coverage.
Rewarding improvement within the gap to goal as well as attainment is important. This was absent from the initial waiver, where some PPSs missed the 10 percent goal by slim margins (sometimes multiple years in a row) despite making significant annual or even 4-year improvements. Neglecting to reward such instances of improvement resulted in PPSs with significant multi-year improvements not earning any incentives. Improvement can be rewarded with partial AVs are other mechanisms. Exploration of the best mechanisms to award improvement will be included in stakeholder sessions relative to the waiver extension.
The most current VMO measurement year (MY) result will be used to determine the gap between the VMO result and the measure´s performance goal, and then a portion of that gap will be added to the most current VMO result to set the annual improvement target for the current MY (i.e., baseline for Measurement Year 1). Each subsequent year will continue to be set with an improvement target using the most recent year´s result. This will account for smaller gains/losses in subsequent years as performance improves toward the goal or measurement ceiling. If a VMO result for a MY meets or exceeds the performance goal, then the annual improvement target and the high-performance target (where applicable) for the next MY will equal the performance goal.
Measure Calculation Process
The New York State Department of Health (NYS DOH) uses several sources of data to report performance measures. Medicaid claims and encounters are the basis for calculation of claims- based measures. Programs used to calculate measure results have been developed using the measure steward specifications. Validation procedures for these programs included: review by external staff experienced in Healthcare Effectiveness Data and Information Set (HEDIS®) source code review, replication of Medicaid managed care submitted data produced from certified HEDIS® software results, and comparison of all Medicaid results from previous years. Medicaid transaction data for the measurement year (January to December) will be considered finalized with the inclusion of the current year June billing information in the transaction systems, allowing a six-month run out of claims data.
For the non-claims-based measures that require clinical data (e.g. Controlling High Blood Pressure) electronic clinical data from the Qualified Entities, NY´s Health Information Exchanges, will be a new data source for measure results. LTC measures are sourced used NYS SPARCS data and the Uniform Assessment System (UAS) for MLTC members. Sources of data are still be explored for Palliative and Hospice Care, Kindergarten readiness, food insecurity and housing instability.
Quality Measures
Exhibit 11 below includes measures that are fully aligned with Medicaid´s VBP Total Care for the General Population measure set, with the addition of avoidable utilization and efficiency measures. Exhibit 12 lists measures to evaluate performance in palliative and hospice care, LTC, and social determinants of health. Please note that these measures will be updated annually as the VBP model is refined and recommendations from VBP CAGs and workgroups are incorporated.
It is anticipated that all measures would be required of the VMOs with the exception of the SDOH measures. SDOH measures will be further explored. Measures for both VMO and SDOH will be vetted through a stakeholder process to finalize the measures. All measures will be required of the VMOs, with the exception of the SDOH measures, from which at least one must be selected.
Exhibit 11: Waiver Renewal VMO Domains
Measure Name ID# Class Data Source Primary Care Domain Antidepressant Medication Management – Effective Acute Phase Treatment & Effective Continuation Phase Treatment NQF0105 P4P Claims Asthma Medication Ratio NQF 1800 P4P Claims Breast Cancer Screening NQF 2372 P4R Claims Cervical Cancer Screening NQF 0032 P4P Claims Chlamydia Screening in Women NQF 0033 P4P Claims Colorectal Cancer Screening NQF 0034 P4R Electronic Clinical Data Comprehensive Diabetes Care: Eye Exams NQF 0055 P4P Electronic Clinical Data Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Poor Control (>9.0%) NQF 0059 P4P Electronic Clinical Data Comprehensive Diabetes Care: Medical Attention for Nephropathy NQF 0062 P4P Electronic Clinical Data Controlling High Blood Pressure NQF 0018 P4P Electronic Clinical Data Diabetes Screening for People w/ Schizophrenia or Bipolar Disorder Using Antipsychotic Medications NQF 1932 P4P Claims Initiation and Engagement of Alcohol & Other Drug Abuse or Dependence Treatment (IET) NQF 0004 P4P Claims Medication Management for People with Asthma NQF 1799 P4P Claims Screening for Clinical Depression and Follow- up NQF 0418 P4P Electronic Clinical Data Children´s Domain Asthma Admission Rate - PDI #14 NQF 0728 P4P Claims Childhood Immunization Status – Combination 3 NQF 0038 P4P Non-Claims Developmental Screening in the First Three Years of Life - P4R Claims Immunizations for Adolescents – Combination 2 NQF 1407 P4P Non-Claims Well–Child Visits in the First 15 Months of Life NQF 1392 P4P Claims Well–Child Visits in the Third, Fourth, Fifth, and Sixth Year of Life NQF 1516 P4P Claims Mental Health Domain Adherence to Antipsychotic Medications for Individuals with Schizophrenia NQF 1879 P4P Claims Depression Remission or Response for Adolescents and Adults - P4P Electronic Clinical Data Follow–Up After Emergency Department Visit for Mental Illness NQF 2605 P4P Claims Follow–Up After Hospitalization for Mental Illness NQF 0576 P4P Claims Potentially Preventable Mental Health Related Readmission Rate 30 Days - P4P Claims Substance Use Disorder Domain Follow-Up After High-Intensity Care for Substance Use Disorder (FUI) - P4P Claims Follow–Up After Emergency Department Visit for Alcohol and Other Drug Dependence NQF 2605 P4P Claims Initiation of Pharmacotherapy upon New Episode of Opioid Dependence - P4P Claims Pharmacotherapy for Opioid Use Disorder (POD) NQF 3175 P4P Claims HIV/AIDS Domain HIV Viral Load Suppression NQF 2082 P4P Electronic Clinical Data Maternal Health Domain Prenatal and Postpartum Care NQF 1517 P4P Electronic Clinical Data Exhibit 12: Waiver Renewal VMO Domains
Measure Name Class Data Source Palliative Care Domain Percentage of patients who were offered or provided an intervention for depressive feelings experienced during the past week P4P Non-Claims IPOS* Percentage of patients who were offered or provided an intervention for not feeling at peace during the past week P4P Non-Claims IPOS* Percentage of patients who were offered or provided an intervention for pain symptoms experienced during the past week P4P Non-Claims IPOS* Percentage of patients who were offered or provided an intervention for physical symptoms (other than pain) experienced during the past week P4P Non-Claims IPOS* Long Term Care Domain Potentially Avoidable Hospitalizations (PAH) for a primary diagnosis of heart failure, respiratory infection, electrolyte imbalance, sepsis, anemia, or urinary tract infection (Community-Based Residents) P4P SPARCS^ Potentially Avoidable Hospitalizations (PAH) for a primary diagnosis of heart failure, respiratory infection, electrolyte imbalance, sepsis, anemia, or urinary tract infection (Nursing Home Residents) P4P SPARCS^ Percentage of members who remained stable or demonstrated improvement in Nursing Facility Level of Care (NFLOC) score P4P UAS + Social Determinants of Health Domain Kindergarten Readiness TBD $ TBD Food Insecurity TBD TBD Housing Stability TBD TBD #NQF – National Quality Forum
*IPOS – Integrated Palliative Care Outcome Scale
^ SPARCS – Statewide Planning and Research Cooperative System
+UAS – Uniform Assessment System for New York for MLTC members
$TBD – To be determined
Section VI – Enrollment in Demonstration
This proposed demonstration does not change affect or modify of the State´s current Medicaid and/or CHIP programs outside for any of the above components. Projected enrollment will not be impacted by this proposal and will be the same with or without waiver. Please refer to attached budget neutrality spreadsheet in Appendix C for projected enrollment associated with budget neutrality.
Section VII – Demonstration Financing and Budget Neutrality
The State is seeking approval of an 1115 waiver amendment to continue delivery system and payment transformation efforts for an additional one-year extension period of the current waiver, and a three-year renewal. This proposal includes a funding extension request as outlined in the following Exhibit 13:
Exhibit 13 - Waiver Programmatic Breakout by Waiver Year (Total Computable $ millions)
Funded Program Year 1 Year 2 Year 3 Year 4 Total Demonstration Year 22 23 24 25 - Waiver Performance $1,210 $4,838 $1,896 $1,896 $9,840 Waiver Administration $40 $40 $40 $40 $160 Workforce Development $0 $1,000 $500 $500 $2,000 Social Determinants of Health $0 $1,200 $900 $900 $3,000 Interim Access Assurance Fund $0 $1,000 $0 $0 $1,000 Total $1,250 $8,078 $3,336 $3,336 $16,000 As required for all 1115 waiver amendment applications, the State has prepared the necessary Budget Neutrality documentation in this section and in Appendix C. Through this exercise, the State has identified the following two considerations for discussion with CMS as part of the review process:
Unearned Funding from the Waiver Program to Fund Year 1 of Waiver Performance Program
The State is seeking CMS approval to leverage previously approved, but undistributed federal funding authority from the current waiver to fund the first year of Waiver Performance expenditures ($1.25B seen in chart above). Current projections for the total undistributed funds from the initial waiver show $1.25B in undistributed funds. Leveraging these undistributed funds would fully cover the funding for the first year of the Waiver Performance Program. As this is a projection, if the undistributed funding were to change the State would seek authority to spend the full amount undistributed.
Spending for Years 2 – 5 of the Current Waiver Counted Against Historical Savings
The current waiver was approved as a reinvestment of the savings generated through initiatives implemented by the Medicaid Redesign Team (MRT). With the implementation of the new Budget Neutrality guidance, formalized in the August 2018 State Medicaid Director (SMD) letter, it would appear the use of savings from what had previously been approved has changed. Now, the expenditures for the current waiver are counted against the savings generated during the current demonstration period and not against the previous savings generated by the State. Under the new Budget Neutrality guidance, states will be limited to carrying forward only those savings generated under the most recent five years´ demonstration period.
The State is requesting CMS consideration for the application of the historical savings generated from the previous demonstration periods to the spending for years two through five of the current waiver. This request would more appropriately align the spending for the currently approved program as a reinvestment of historical savings as was agreed to under of the initial amendment. This request would also ensure that New York is not disproportionately impacted by the application of new Budget Neutrality guidance that was not introduced until four years after the approval of the initial waiver application.
The current Budget Neutrality calculations, excluding this proposed amendment, project the following savings for the current demonstration period of April 1, 2016 – March 31, 2021 (DY18 – DY22):
Exhibit 14: 1115 Budget Neutrality Project Savings by Waiver Year (Total Computable $ millions)
Demonstration Year 18 19 20 21 22 Total Savings (DY18-DY22) Projected Savings $1,459 $892 $1,733 $2,933 $5,576 $12,594 However, if the expenditures associated with the initial waiver were to be counted against the historical savings generated in the prior demonstration period as noted in the narrative above, the savings for the current demonstration period would be projected as follows:
Exhibit 15: 1115 Budget Neutrality Project Savings by Waiver Year Initial Waiver Expenditures Excluded (Total Computable $ millions)
Demonstration Year 18 19 20 21 22 Total Savings (DY18 – DY22) Projected Savings $1,459 $892 $1,733 $2,933 $5,576 $12,594 + Initial Waiver Expenditures* $2,703 $3,027 $2,540 $1,944 $0 $10,214 Revised Savings $4,162 $3,919 $4,273 $4,877 $5,576 $22,808 This Waiver Extension period of this amendment is anticipated to result in approximately $625M in federal funding that was approved but unspent from the current waiver through the end of the Waiver Extension period and an additional $7.375B through DY 25 for the Waiver Extension period. Accordingly, the State anticipates the annual average demonstration cost of $58.8B will be increased by the dollars indicated in Exhibit 12 Waiver Programmatic Breakout by Waiver Year displayed in the application and reduce the overall Budget Neutrality savings by $16B in the next demonstration period as a result of the adoption of this amendment
Section VIII – Proposed Waivers and Expenditure Authorities
The State requests the following waivers and expenditure authorities to operate the demonstration, as outlined below in Exhibit 17: Proposed Waiver Authorities and following subsection discussing Proposed Expenditure Authorities.
Exhibit 17: Proposed Waivers and Authorities
Waiver Authority Reason and Use of Waiver 1115(a) – Extension of the Existing Demonstration Project To the extent necessary to enable the State to extend the existing waiver for an additional year and to extend, a modified amendment, focused on Value Based Care. 1902(a)(13)(A) and 1902(a)(13)(A) – Payments to Providers Under the State Plan To the extent necessary to enable the State to reduce supplemental payments to institutional providers otherwise authorized under the approved State plan so that priority is given to funding delivery system reform incentive payments and Value Based Care.
Section IX – Compliance with Public Notice and Tribal Notification
Public Notice Process
The state certifies that the first public notice and tribal notification for the formal waiver amendment were published in the New York State Register on October 2nd, 2019, with written comments to be received by electronic or written mail by November 4th, 2019.
Two in-person public hearings were held in two separate locations during the fall of 2019, seen below with exact upstate and downstate locations. The public hearings were broadcasted live via webcast (accessible via the New York MRT website) and were scheduled to gather feedback and assure public input on the waiver extension request. All interested speakers were given an opportunity to express their views which were documented and incorporated into the final waiver extension application. No pre-registration was necessary for the public hearings. All comments were limited to 5 minutes per presenter to ensure that all public comments were heard. Public comment transcripts, slides, and supporting materials are publicly available on the New York MRT website.16
The State further certifies that the public was notified of the intent to submit a waiver amendment to CMS, as evidenced by the announcement posted on the New York MRT website.17 Additionally, the State certifies that a notice of the waiver amendment was posted in the New York State Register.
The downstate public comment day was held on October 25, 2019 from 11:00am – 2:00pm at Baruch College, 55 Lexington Ave. (Corner of 24th St. & Lexington Ave.), Room 14–220 (14th Floor), New York, NY 10010. The upstate public comment was held on October 30, 2019 from 11:00am – 2:00pm at The Oncenter Carrier Theater, 421 Montgomery Street, Syracuse, NY 13202.
Both comment sessions included a current overview of current 1115 waiver initiatives as well as a brief summary of New York´s Medicaid Redesign Team (MRT) concept paper. After the presentation by NYS DOH staff, commenters were afforded the opportunity to present oral comments, questions, or recommendations to the panel of NYS DOH staff, limited to five minutes per commenter. All comments that were presented during these sessions were made available in their written format on the New York MRT website.
The State certifies that it used an electronic mailing list to notify the public of the State´s intent to seek a waiver amendment to CMS. The State created a Medicaid Redesign Team Listserv (MRT Listserv) in order to notify interested parties that new information was posted on the MRT website. The notices alerted subscribers to new information available on the MRT website which included: meeting announcements, access to webcasts, meeting materials, updated timelines, press releases and any other information of interest. This listserv was available to the public for email sign-up and was also used as a mechanism to receive public comments. Individuals who wished to submit written comments during the aforementioned periods were able to do so by writing an email to1115waivers@health.ny.gov. by including "1115 Public Forum Comment" in the subject line.
Public Comment
Overview. The State received over 200 comments, both written and verbally, from individuals, advocacy groups, community providers and other stakeholders. These are available online at the State website.18 The State appreciates all of the comments and feedback shared by its stakeholders regarding this waiver amendment proposal. These comments informed the content and approach of this amendment application. In fact, the state changed its approach in considering several comments that expressed concerns with the readiness for program implementation of VMOs, SDHNs and MCO engagement, and suggested the state change the timeline and structure of the original draft plan to a two-phase, extension and then renewal approach. Public comments suggested allowing a one-year transition (the current Phase One Extension Waiver Request) to the new program to allow more time to prepare for the implementation of what is now Phase Two, the 3-year Waiver Renewal. The current proposal reflects the importance of stakeholder public comment and the State´s responsiveness to these suggestions.
Generally, commenters expressed overall support for the changes proposed in the waiver amendment. Questions and comments about the governance, leadership, regionalization, and inclusion of CBOs and MCOs, as well as of the VMO and SDHN structures were found to be among the most common questions received in both written comment and in-person sessions.
Many comments were concerned with workforce investments in long-term care workers, BH providers, and how funds would be utilized to help defray the costs of training expenses for a variety of different healthcare providers. Questions about the additional "high-needs priority" areas were raised concerning how the State intended to link their Prevention Agenda to populations that were explicitly mentioned in this waiver amendment such as Children, Maternal mortality and Medicaid members with OUD.
A summary of the comments submitted and the State´s responses to those comments are provided below. Some comments were not germane and outside of the scope of this amendment proposal; these are not addressed in the comments below.
Public Comment Themes and State Response
Development, Role, and Governance of Value Management Organizations (VMOs)
The construction of VMOs were heavily influenced by comments and questions received from a variety of stakeholders during the public comment period. Questions about MCO engagement, VBP readiness, and SDHN alignment were clarified (Please refer to Section II) as to structure the VMOs in accordance with feedback received during the public comment period. The geography that is covered by VMOs as well as what entities would be able to serve in the lead role of the VMO was also considered in developing the proposed structures. Comments from various sectors requested more meaningful representation of community-based primary care, BH, and LTC providers in VMO governance to assure investments into these areas. The state has addressed concerns in diversity in VMO governance and as part of network adequacy in VBP incentive funding pools. Consumer representation has been incorporated into the VMO structure. As seen in Section II, these comments informed the State´s general thinking and strategy as to how VMOs would be part of the transition.
Development of Attribution Methodology
Providers and PPSs commented in this area. With the exception of some notable outliers, the early yet encouraging work in VBP has focused almost exclusively around primary care and requires the State to consider multiple accountability points in this new amendment request. When developing new guidance on attribution methodology, the State was heavily influenced by public comment regarding the participation of other disciplines who may be more accountable for the outcomes of particular populations, such as behavioral health providers, and for attribution to be based on patients´ patterns of care utilization. Other comments requested that VMO attribution align with MCO attribution. Other comments suggested prospective attribution set annually instead of the rolling retrospective methodology. Suggestions also were made to include all Medicaid members in VMO attribution and for there to be regional/geographic responsibility to engage all providers and payors to promote population health goals.
As described in Section II, the State took public comment into consideration to inform strategy on the VMO Performance and VBP Incentive Pools. These funding streams underscore the public comments on current attribution methodology and aim to clarify the State´s intention to create incentives for VMOs and MCOs to achieve performance and accountability milestones based on the goals and objectives established for their respective funding pools and attributed member populations.
Program Development and Performance Measurement
Program and performance measurement were informed by public comment from a variety of provider/service trade associations and advocacy organizations. Feedback was received on program aspects such as the need for more attention on duals and the Long Term and Post- Acute Care sector. Comments also addressed types of services to serve high risk children. There were questions regarding the program selection process and the parameters of performance measurement. There were requests for performance and program measurement to be simplified and transparent. In consideration of these comments, the state developed program and Total Cost of Care VBP performance measures as seen in Section V, that cover six key areas:
- Primary Care,
- Children´s,
- Mental Health,
- Substance Use Disorder (SUD),
- HIV/AIDS, and
- Maternal Health, while two additional areas specifically focused on
- Palliative and Hospice Care and
- Long-term Care measures that look at potentially avoidable hospitalizations and nursing facility level of care scores.
The State´s strategy to create consistent and transparent performance and program measures was also informed by the ongoing stakeholder process of the VBP and Preventive Pediatric Care CAGs as well as the public comments received.
Role of CBOs in VMOs and SDHNs
CBOs, social care organizations, and advocates commented on the role of CBOs. The role of CBOs in VMO and SDHN, and the role of the SDHN were heavily influenced by public comments and questions about VMO governance, SDHN role within the VMOs, relationship of VMO and SDHN, CBO leadership of SDHN, the data exchange capabilities, incorporating specific requirements for MCOs on CBO contract inclusion, and inclusion of Area Agencies on Aging as SDOH service providers. Many of the comments will help craft the envisioned SDHN procurement process as part of Phase Two Waiver Renewal and will create accountability of MCOs in developing VBP arrangements that are inclusive of CBOs. Furthermore, public comment informed the State in developing the reimbursement strategy for SDOH as part of VMOs through creating a statewide standard.
MCO Participation
In consideration of ensuring MCO participation, the State considered feedback from the public on measures such as data sharing and transparency, risk-sharing and encouraging MCOs to shift risk to VMOs while compensating for value. The State has expressly designed the Waiver Renewal to incentivize and integrate MCO participation to collaborate in this waiver´s plan and in Section II outlines a plan to engage MCOs and their participation in facilitating the maturation of VBP arrangements with a variety of health care system stakeholders.
Role of Behavioral Health Providers in VMOs
Recognizing the contributions of BH health providers and how their participation in VMOs will be a vital part of moving beyond progress made in the current waiver was highlighted in the public comments addressed to the State. Questions concerning the attribution mechanisms and developing BH-specific rewards that go beyond just Total Cost of Care greatly informed the State´s strategy. In Section II the State emphasizes the need for VBP arrangements to evolve and include specialty providers such as BH providers to strengthen these arrangements by expanding rewards and shared savings.
Data Use and Access
A variety of providers, PPSs, IPAs, QEs, social care, and CBO stakeholders commented on Data Use and Access promoting widespread data access across multiple sectors to encourage exchange accountability and overcome limitations of state-provided data to develop data integration is key to the State´s strategy in the amendment request. Questions concerning the prominence and role of HIEs within VMOs heavily influenced the State´s strategy in including these aspects of data use and access within new and existing structures.
Workforce Development Needs
During the public comment period many stakeholders expressed the need for continued investment in workforce and had questions and suggestions for how it would be implemented across a variety of different providers and modalities. In acknowledging these questions, the State has developed strategies to continue workforce flexibility and investment (as seen in Section II), improve upon the promising practices realized, develop funds to defray training expenses, expand the peer and community health worker base, and develop opportunities for non-traditional health care workers.
Use of Regulatory Authorities
The regulatory authorities that are being utilized in this amendment request are similar to that of the current waiver. During the public comment period, questions about the use of regulatory waivers and general support for extending what has already been approved were shared by some individuals. The State´s strategy is to continue utilizing the existing regulatory authorities for this amendment request as informed by general support provided during the public comment period.
Long-Term Care Needs
The State´s LTC strategy was heavily influenced by public comments received. Questions about the consideration of LTC facilities inclusion for the IAAF, continued workforce investments and workforce support and to make a distinction between LTC from Post-Acute care. As seen in Section I and II, the State considers LTC and Post-Acute care a top priority and has incorporated both into distinct parts of the State´s strategy to facilitate the promising practices while enabling LTC MCOs and providers to participate meaningfully in VBP arrangements.
Children´s Health Needs
As with LTC, the State acknowledged the need for additional focus on specific sub-populations like Children to be included in the amendment request. The public comments and questions reflected this need and thus greatly influenced the State´s strategy in the development of upstream connections with the Prevention Agenda for children and families, and a comprehensive two-generational approach, as seen in Section II. The State´s strategy is reflective of comments received on the investment in peer coaches, the continued utilization of the pediatric CAG´s work, and cross-sector collaboration.
Opioid Crisis Needs
Continued focus on the Opioid Crisis in New York State was a need expressed by many commenters during the public comment period. The State´s strategy on continued efforts to address OUD by integrating and expanding MAT to justice-involved populations and primary care, ED settings, as well as OUD/SUD peer bridging support from ED inpatient to community- based treatment is seen in Section I and Appendix A.
Tribal Notification
New York State is home to nine federally recognized Tribal Nations.19
- Tonawanda
- Tuscarora
- Seneca
- Onondaga
- St. Regis Mohawk
- Oneida
- Cayuga
- Shinnecock
- Unkechaug (Poospatuck)
In accordance with 42 CFR 431.408(b), on September 17th, 2019 (60 days prior to submission of the waiver extension application to CMS) the Department of Health advised the above- mentioned tribes by letter of the intent to request a four-year extension via amendment, (refer to Appendix D, Tribal Letter). During this 60-day period, no comments were received from any of the aforementioned tribes.
Section X – Demonstration Administration
Name and Title:
Donna Frescatore
Medicaid Director
Office of Health Insurance Programs
New York State Department of HealthTelephone Number:
(518) 474-3018
Email Address:
Appendix A – Promising Practices Alignment
Exhibit 16 - New York State Waiver Amendment/Extension Request
CMS Priorities Promising Practice alignment/Program Extension Areas SUD and the Opioid Crisis Transforming and Integrating Behavioral Health
- Expanding Access and Provider Capacity at Critical Levels of Care, including for Medication-Assisted Treatment
Integration and expansion of Medication-Assisted Treatment in primary care and ED settings
- Integration and expansion of MAT into primary care and emergency rooms.
- SUD peer bridging support from ED and inpatient settings to community-based treatment.
- MAT focus on justice-involved population
- Implementing Comprehensive Treatment Strategies to Address OUD
Partnerships with the justice system and other cross-sector collaborations
- Work with criminal justice sector for post-arrest and pre- arraignment diversion and treatment.
SMI/SED Demonstration Transforming and Integrating Behavioral Health
- Primary Care/Behavioral Health Integration
Primary care and behavioral health integration
- Hot-spotting and data sharing among PCP, BH and inpatient providers for improved follow-up of care.
- Expansion of primary care at BH sites and BH at primary care sites, and screenings for SUD, depression and chronic disease management.
- Care Transitions to Reduce Avoidable ED Visits and Readmissions
Care coordination, care management, and care transitions
- Coordinate BH treatment from jails to post-release in the community.
- Hot-spotting high-risk behavioral health patients for intensive care management.
- Transitional care teams for patients at risk of readmission.
- Transitional care teams of clinicians and peers bridging psychiatric inpatient to community settings.
- Leverage telemedicine for care management of individuals with I/DD or other special populations for ED triage.
- Integration of peers for outreach, support and navigation for care of special populations - HIV, BH and SUD.
- Integration of peers for chronic disease management - asthma and diabetes.
- Integration of community and social service providers into care teams for comprehensive care coordination.
- Crisis Stabilization
Expansion of Mobile Crisis Teams (MCT) and crisis respite services
- MCT expansion and crisis respite capacity.
- Children´s BH urgent care center (8.2)
- Peer outreach to track and support patients in crisis programs, such as mobile crisis, crisis respite, post-discharge treatment.
- Institute of Mental Disease - Transition short-term stay patients from IMD to community
Extend successful practices above in cross-sector collaboration, care transitions, and care management to patients transitioning from IMDs to the community.
- Transitional care teams of clinicians and peers bridging psychiatric inpatient to community settings.
- Peer outreach to track and support patients in crisis programs, such as mobile crisis, crisis respite, post-discharge treatment.
- Increase crisis stabilization programs and extend to children.
- Serious Emotional Disturbance (SED)
Extend successful practices above in cross-sector collaboration, care transitions and care management to apply to SED children.
- Increase crisis stabilization programs and extend to children.
- Children´s BH urgent care center.
- Leverage telemedicine for care management of residential populations for ED triage.
- Transitional care teams of clinicians and peers bridging psychiatric inpatient to community settings.
Social Determinants of Health Social Needs, Community Partnerships
- CMMI Accountable Health Communities model
- Transportation, nutrition, housing, in-home visits
Addressing Social Determinants of Health through Community Partnerships
- Social needs screening by CHWs at bedside, provider site and in the home.
- Food as Health in the hospital and at home, addressing food insecurity, nutrition and other social factors.
- Community navigation and care management.
- Integrated electronic clinical and SDH screening referral systems linking clinical providers to community partners for services and feedback loop.
Primary Care Initiatives Primary Care and Alternative Payment Models CPC+ and Primary Care First VBP 20 Transforming Primary Care and Supporting Alternative Payment Models (APMs)
- The initial waiver and SIM have provided practice transformation support and significantly increased the level of advanced primary care recognition in NYS and in turn, the capacity of these practicesto further engage in population health and VBP arrangements. - The State seeks to incorporate Medicaid into APM to align and streamline performance and financial incentives. This would promote providers to focus on high-value performance measures and increase overall VBP adoption across payers.
ADDITIONAL PRIORITIES Children InCK Model through CMMI Investing in Community Health Workers (CHW) for Chronic Disease Management
- The initial waiver providers developed Asthma Action Plans for children with asthma and referred families to CHW programs for home-based services, to include referrals for pest management and mold remediation services when asthma triggers were identified
Crisis Stabilization: Preventing Unnecessary Behavioral Health Hospitalizations
- Behavioral health urgent care center for children 5-17 years old
Fostering Cross-Sector Collaborations to Target Behavioral Health in Schools
- A program focusing on prevention and early identification of behavioral health problems among students, using coaches to train teachers and staff and deliver crisis support and behavioral health referrals to students and families
Long-term Care Disabled Members and Older Adults Medicare Post-Acute Care Transformation Act of 2014 (the IMPACT Act) 21 Building Quality Improvement Capacity Across the Care Continuum
- Implementing the INTERACT (Interventions to Reduce Acute Care) program across a network of 27 skilled nursing facilities (SNFs) to reduce transfers tohospitals
- Building in more systematic palliative care referralsin SNFs
Tracking High Utilizers Across Multiple Settings to Bridge Gaps in Coordination
- Technical assistance through the Medicaid Accelerated eXchange (MAX) series for Rapid-Cycle Continuous Improvement to address high utilizers with unmet palliative care needs
Appendix B – Promising Practices Examples
The PPS examples below elaborate on some of the promising practices outlined in the preceding Exhibit 16 and more detailed representations can be found in the UHF Report, "DSRIP Promising Practices: Strategies for Meaningful Change in New York Medicaid". The strategies described suggest opportunities for larger outcome improvement if given the time and resources for effective scaling and replication. There are many examples of similar PPS efforts and these are not intended to represent the full breadth and depth of promising practices that the initial waiver has fostered across the State.
1. Addressing the Opioid Crisis Through the Integration and Expansion of Medication-Assisted Treatment in Primary Care and Emergency Department Settings
1.1 Leatherstocking PPS championed the recruitment, training, and certifying of additional primary care practitioners to provide medication-assisted treatment, thereby improving access to treatment for opioid use disorder.
1.2 Central NY Care Collaborative PPS and SUNY Upstate emergency department providers initiated opioid use disorder treatment for patients, providing transition support through interim services and peer outreach until the patients are able to receive ongoing treatment.
2. Addressing the Opioid Crisis and Behavioral Health Needs through Partnerships with Education, Law Enforcement/Justice System and Other Cross-Sector Collaborations
2.1 Adirondack Health Institute PPS focused on diversion programs where treatment for SUD and behavioral health issues are alternatives to arrest and incarceration. Law enforcement officials were trained in crisis intervention strategies and resources. Care managers meet with people with behavioral health issues in the jail to develop plans for connecting these individuals with post-release community services. Pre- and post-arraignment diversion programs focus on supporting treatment and recovery for behavioral health needs, such as opioid use disorder.
2.2 100 Schools Project is a collaboration to strengthen the capacity of schools in underserved communities to meet their students´ disproportionately greater behavioral health needs. Four PPSs-Bronx Health Access, Bronx Partners for Healthy Communities, Community Care of Brooklyn, and OneCity Health-and the Jewish Board of Family and Children´s Services partnered with four behavioral health providers, New York City (NYC) government units, and underserved NYC public schools. The program focuses on prevention and early identification of behavioral health problems among students, using coaches to train teachers and staff and deliver crisis support and make behavioral health referrals to students and families. In turn, the program also aims to improve students´ educational outcomes, such as reductions in truancy and suspensions. In 2018, about half (49%) of all behavioral health crises where police responded to 911 calls at participating schools were mitigated without an arrest and without the student needing to leave school, compared to a quarter (26%) of such crises across all city schools.
3. Hot-Spotting High-Risk Behavioral Health Members and Mobilizing Care Teams for Engagement
3.1 Mt. Sinai and Staten Island PPS, in partnership with Health Home and community care management providers, targeted high-risk BH members using utilization and clinical data from the state, as well as hospital and Qualified Entity sources. The PPSs worked with patients´ providers to enroll them in six-month intensive care management programs linking appropriate outpatient care and community social supports.
4. Expanding Primary Care within Behavioral Health Sites and Behavioral Health within Primary Care Sites
4.1 Montefiore Hudson Valley PPS and Suffolk Care Collaborative PPS bridged gaps in care management by integrating physical and behavioral health care through the operation of van-based mobile health centers that deliver primary care services and screenings to patients at multiple behavioral health provider sites.
4.2 Refuah Community Health Collaborative PPS integrated behavioral health services into primary care settings through multiple strategies, including: data sharing, workforce expansion, development of shared behavioral health protocols, new workflows and delivery models in primary care settings, and investments in co-location.
5. Care Coordination, Care Management, and Care Transitions for At-Risk Patients
5.1 The Community Care of Brooklyn PPS created Transitional Care Teams (TCTs) of nurses and care managers to work with patients at risk for 30-day readmission, by addressing medication concerns and providing condition-specific education. Post-intervention reductions in TCT patients with ED visits ranged from 1.5% to 6.9%, and reductions in TCT patients with hospital admissions ranged from 11.5% to 18.7%,
5.2 Community Partners of Western New York PPS fostered community-based telemedicine programs that support effective care transitions and provide ongoing in-home ED triage and monitoring for special subpopulations such as individuals with intellectual and developmental disabilities and chronic disease patients with palliative care needs.
5.3 Staten Island PPS developed a comprehensive care coordination program supporting individuals identified as "at risk" of future Health Home eligibility by building partnerships between the PPS, two Health Homes, a community health center, and a CBO to train care coordinators in providing health coaching and community support to the at-risk individuals.
6. Integration of Peer Support (SUD, HIV, BH) and CHWs for Specific Populations for Improved Outcomes
6.1 Montefiore Hudson Valley Collaborative PPS partnered with an inpatient detoxification and rehabilitation facility to hire two certified peer recovery coaches to meet a variety of needs for individuals transitioning out of the facility into early recovery. During calendar year 2018, peer recovery coaches ensured that 100% of the 122 transitioning patients attended their first outpatient appointment. Of those, 80% of recovering patients attended their first appointment within seven days of discharge, and nearly 96% kept their second appointment. Patients completed more routine discharges, experienced better transitions to, and long-term engagement with, outpatient treatment, and had lower rates of readmissions.
6.2 WMCHealth PPS partnered with community BH clinicians and peers to create an inpatient psychiatric transitions program including a meeting with patients in the hospital prior to discharge, an in-home assessment 48 hours post-discharge, and follow-up support with navigating medical appointments and community-based resources.
6.3 New York-Presbyterian PPS, building on its three existing Designated AIDS Centers, the hospital EDs, and ambulatory care network, further transformed its already robust HIV/AIDS care and prevention services with the involvement of six CBOs, Community Health Workers, and peers who were vital to the outreach efforts necessary to make a population- level impact.
7. CHWs/Peer Mentors for Chronic Disease Management of Asthma and Diabetes
7.1 OneCity Health, the largest PPS, trained 29 CHWs across 8 CBOs to be deployed in the home visitation program for asthma. Clinicians develop Asthma Action Plans (AAPs) for children with asthma and CHWs visit the families´ homes, supporting the AAPs and arranging remediation when asthma triggers are identified. Within a six-month period, OneCity reports the pediatric asthma admission rates (PDI-14) decreased by 25%.
7.2 WMCHealth PPS implemented evidence-based self-management programs for diabetes in partnership with CBOs and peer mentors. The PPS partnered with CBOs to implement the Stanford University Self-Management Resource Center model, while also initiating a one- on-one peer mentoring pilot for Medicaid patients with uncontrolled diabetes.
8. Expansion of Mobile Crisis Teams and Crisis Respite Services for Behavioral Health
8.1 Three upstate PPS (Central NY Care Collaborative, Care Compass Network and Better Health for Northeast NY) have expanded the number and capacity of Mobile Crisis Teams in 18 counties, increasing timely access and reducing emergency use for BH needs. Crisis respite capacity has also been built to provide more appropriate settings for BHtreatment.
8.2 Nassau Queens PPS partnered with Northwell Health to support opening a Children´s BH urgent care center for children age 5-17, co-located with pediatric ambulatory services. With mental health service access limited, the center serves to bridge gaps in treatment, helping to coordinate care with schools, pediatricians, and other healthcare professionals.
9. Addressing Social Determinants of Health through Community Partnerships
9.1 Nassau Queens PPS partner Northwell Health implemented a "Food as Health" program to connect food insecure patients who have a nutrition-related diagnosis with a structured network of resources in the community including the delivery of medically tailored meals as appropriate. Results have shown the services may have contributed to lower A1C scores, increased primary care visits, increased SNAP enrollment, and decreased food insecurity, ED use, and readmissions.
9.2 Finger Lakes PPS partnered with CBOs, BH providers, care management agencies, and FQHCs to utilize trained community navigators to build on its patient activation efforts and connect over 17,000 individuals to medical services and social resources. The PPS reports that these efforts have helped decrease potentially preventable ED visits and increase access to primary care.
10. Transforming Primary Care
10.1 PPS and State Innovation Model (SIM) efforts provided practice transformation support and significantly increased the level of advanced primary care recognition in NYS, enhancing the capacity of these practices to manage complex patients and participate in integrated delivery systems, paving the way towards engaging in population health and VBP arrangements. New York has over 9000 clinicians who are PCMH-recognized.
10.2 SOMOS PPS is among the state´s leaders in supporting small practice providers where 646 of their affiliated clinicians achieved PCMH recognition. SOMOS invested in training and deployment of CHWs to support the practices in care management, outreach and education efforts with their patients.
Appendix C – Budget Neutrality
Please refer to the following excel file for exhibits 17 and 18 listed below:
Waiver Performance 1115 Budget Neutrality UPDATED.xlsx
- Budget Neutrality Exhibit 18
- Historical Expenditure Exhibit 19
Appendix D – Tribal Consultation
September 17, 2019
Clinton Halftown
Nation Representative
Cayuga Nations
PO Box 803
Seneca Falls, NY 13148Dear Mr. Halftown:
The New York State Department of Health (NYSDOH) is providing notice of the State´s intent to request approval from the Centers for Medicare and Medicaid Services (CMS) for a four (4) year waiver amendment to further support the quality improvements and cost savings through the Delivery System Reform Incentive Payment (DSRIP) program. As with the original Medicaid Redesign Team (MRT) waiver, New York State seeks a continuation of DSRIP for the 1-year balance of the 1115 waiver ending on March 31, 2021 and conceptual agreement to an additional 3 years from April 2021 to March 31, 2024. Thus, the full four-year extension/renewal period (1-year extension and 3 years of renewal) would span from April 1, 2020 through March 31 , 2024.
The New York DSRIP program has already reduced Potentially Preventable Admissions through June 2018 of 21%, well on its way to the goal of 25% by the end of the demonstration. The waiver amendment seeks additional time and funding support for the community collaborations to be sustained and fully mature to successfully transition the DSRIP Promising Practices into Value Based Payment (VBP) arrangements. The State will focus on higher-value practices that are clearly aligned with federal priorities. These federal priority areas include: Substance Use Disorder (SUD) treatment and the Opioid Crisis; Serious Mental Illness and Severe Emotional Disturbance (SMI/SED); Social Determinants of Health; Primary Care Improvement and Value-Driving Payment Models.
In addition, the DSRIP promising practices would expand to certain high-need and highcost populations, such as higher-risk children and members needing long-term care. A continuation of workforce investments is essential to be responsive in meeting future needs, especially in the long-term care sector, as well as aid to financially distressed hospitals to help accelerate the transformation of acute and ambulatory health care.
The anticipated impact this demonstration would have on Tribal members includes:
- Improving patient-centered care by further sustaining the integration across physical health, behavioral health, addiction treatment, and social services in communities;
- Improving access through sustained workforce investments and aid to financially distressed hospitals; and
- Improving care for higher-risk children and Medicaid members in need of longterm care.
A draft of the amendment proposal is available for review here.
Written comments will be accepted by email at 1115waivers@health.ny.gov or by mail at the address below. All comments must be postmarked or emailed by November 4th, 2019.
NYS Department of Health
Office of Health Insurance Programs
Waiver Management Unit
99 Washington Avenue
12th Floor, Suite 1208
Albany, NY 12210We look forward to our continued collaboration.
Sincerely,
Gregory S. Allen, Director
Division of Program Development & Management
Office of Health Insurance Programscc: Sean Hightower
Vennetta Harrison
Phil Alotta, NYSDOH
Michele Hamel, NYSDOH
September 17, 2019
Joseph Heath
Nation Representative
Cayuga Nations
512 Jamesville Avenue
Syracuse, NY 132108Dear Mr. Heath:
The New York State Department of Health (NYSDOH) is providing notice of the State´s intent to request approval from the Centers for Medicare and Medicaid Services (CMS) for a four (4) year waiver amendment to further support the quality improvements and cost savings through the Delivery System Reform Incentive Payment (DSRIP) program. As with the original Medicaid Redesign Team (MRT) waiver, New York State seeks a continuation of DSRIP for the 1-year balance of the 1115 waiver ending on March 31, 2021 and conceptual agreement to an additional 3 years from April 2021 to March 31, 2024. Thus, the full four-year extension/renewal period (1-year extension and 3 years of renewal) would span from April 1, 2020 through March 31 , 2024.
The New York DSRIP program has already reduced Potentially Preventable Admissions through June 2018 of 21%, well on its way to the goal of 25% by the end of the demonstration. The waiver amendment seeks additional time and funding support for the community collaborations to be sustained and fully mature to successfully transition the DSRIP Promising Practices into Value Based Payment (VBP) arrangements. The State will focus on higher-value practices that are clearly aligned with federal priorities. These federal priority areas include: Substance Use Disorder (SUD) treatment and the Opioid Crisis; Serious Mental Illness and Severe Emotional Disturbance (SMI/SED); Social Determinants of Health; Primary Care Improvement and Value-Driving Payment Models.
In addition, the DSRIP promising practices would expand to certain high-need and highcost populations, such as higher-risk children and members needing long-term care. A continuation of workforce investments is essential to be responsive in meeting future needs, especially in the long-term care sector, as well as aid to financially distressed hospitals to help accelerate the transformation of acute and ambulatory health care.
The anticipated impact this demonstration would have on Tribal members includes:
- Improving patient-centered care by further sustaining the integration across physical health, behavioral health, addiction treatment, and social services in communities;
- Improving access through sustained workforce investments and aid to financially distressed hospitals; and
- Improving care for higher-risk children and Medicaid members in need of longterm care.
A draft of the amendment proposal is available for review here.
Written comments will be accepted by email at 1115waivers@health.ny.gov or by mail at the address below. All comments must be postmarked or emailed by November 4th, 2019.
NYS Department of Health
Office of Health Insurance Programs
Waiver Management Unit
99 Washington Avenue
12th Floor, Suite 1208
Albany, NY 12210We look forward to our continued collaboration.
Sincerely,
Gregory S. Allen, Director
Division of Program Development & Management
Office of Health Insurance Programscc: Sean Hightower
Vennetta Harrison
Phil Alotta, NYSDOH
Michele Hamel, NYSDOH
September 17, 2019
Ray Halbritter
Nation Representative
Oneida Indian Nation
5218 Patrick Road
Verona, NY 13478Dear Mr. Halbritter:
The New York State Department of Health (NYSDOH) is providing notice of the State´s intent to request approval from the Centers for Medicare and Medicaid Services (CMS) for a four (4) year waiver amendment to further support the quality improvements and cost savings through the Delivery System Reform Incentive Payment (DSRIP) program. As with the original Medicaid Redesign Team (MRT) waiver, New York State seeks a continuation of DSRIP for the 1-year balance of the 1115 waiver ending on March 31, 2021 and conceptual agreement to an additional 3 years from April 2021 to March 31, 2024. Thus, the full four-year extension/renewal period (1-year extension and 3 years of renewal) would span from April 1, 2020 through March 31 , 2024.
The New York DSRIP program has already reduced Potentially Preventable Admissions through June 2018 of 21%, well on its way to the goal of 25% by the end of the demonstration. The waiver amendment seeks additional time and funding support for the community collaborations to be sustained and fully mature to successfully transition the DSRIP Promising Practices into Value Based Payment (VBP) arrangements. The State will focus on higher-value practices that are clearly aligned with federal priorities. These federal priority areas include: Substance Use Disorder (SUD) treatment and the Opioid Crisis; Serious Mental Illness and Severe Emotional Disturbance (SMI/SED); Social Determinants of Health; Primary Care Improvement and Value-Driving Payment Models.
In addition, the DSRIP promising practices would expand to certain high-need and highcost populations, such as higher-risk children and members needing long-term care. A continuation of workforce investments is essential to be responsive in meeting future needs, especially in the long-term care sector, as well as aid to financially distressed hospitals to help accelerate the transformation of acute and ambulatory health care.
The anticipated impact this demonstration would have on Tribal members includes:
- Improving patient-centered care by further sustaining the integration across physical health, behavioral health, addiction treatment, and social services in communities;
- Improving access through sustained workforce investments and aid to financially distressed hospitals; and
- Improving care for higher-risk children and Medicaid members in need of longterm care.
A draft of the amendment proposal is available for review here.
Written comments will be accepted by email at 1115waivers@health.ny.gov or by mail at the address below. All comments must be postmarked or emailed by November 4th, 2019.
NYS Department of Health
Office of Health Insurance Programs
Waiver Management Unit
99 Washington Avenue
12th Floor, Suite 1208
Albany, NY 12210We look forward to our continued collaboration.
Sincerely,
Gregory S. Allen, Director
Division of Program Development & Management
Office of Health Insurance Programscc: Sean Hightower
Vennetta Harrison
Phil Alotta, NYSDOH
Michele Hamel, NYSDOH
September 17, 2019
Irving Powless, Jr., Chief
Onondaga Nation
PO Box 319-B
Nedrow, NY 13210Dear Chief Powless:
The New York State Department of Health (NYSDOH) is providing notice of the State´s intent to request approval from the Centers for Medicare and Medicaid Services (CMS) for a four (4) year waiver amendment to further support the quality improvements and cost savings through the Delivery System Reform Incentive Payment (DSRIP) program. As with the original Medicaid Redesign Team (MRT) waiver, New York State seeks a continuation of DSRIP for the 1-year balance of the 1115 waiver ending on March 31, 2021 and conceptual agreement to an additional 3 years from April 2021 to March 31, 2024. Thus, the full four-year extension/renewal period (1-year extension and 3 years of renewal) would span from April 1, 2020 through March 31 , 2024.
The New York DSRIP program has already reduced Potentially Preventable Admissions through June 2018 of 21%, well on its way to the goal of 25% by the end of the demonstration. The waiver amendment seeks additional time and funding support for the community collaborations to be sustained and fully mature to successfully transition the DSRIP Promising Practices into Value Based Payment (VBP) arrangements. The State will focus on higher-value practices that are clearly aligned with federal priorities. These federal priority areas include: Substance Use Disorder (SUD) treatment and the Opioid Crisis; Serious Mental Illness and Severe Emotional Disturbance (SMI/SED); Social Determinants of Health; Primary Care Improvement and Value-Driving Payment Models.
In addition, the DSRIP promising practices would expand to certain high-need and highcost populations, such as higher-risk children and members needing long-term care. A continuation of workforce investments is essential to be responsive in meeting future needs, especially in the long-term care sector, as well as aid to financially distressed hospitals to help accelerate the transformation of acute and ambulatory health care.
The anticipated impact this demonstration would have on Tribal members includes:
- Improving patient-centered care by further sustaining the integration across physical health, behavioral health, addiction treatment, and social services in communities;
- Improving access through sustained workforce investments and aid to financially distressed hospitals; and
- Improving care for higher-risk children and Medicaid members in need of longterm care.
A draft of the amendment proposal is available for review here.
Written comments will be accepted by email at 1115waivers@health.ny.gov or by mail at the address below. All comments must be postmarked or emailed by November 4th, 2019.
NYS Department of Health
Office of Health Insurance Programs
Waiver Management Unit
99 Washington Avenue
12th Floor, Suite 1208
Albany, NY 12210We look forward to our continued collaboration.
Sincerely,
Gregory S. Allen, Director
Division of Program Development & Management
Office of Health Insurance Programscc: Sean Hightower
Vennetta Harrison
Phil Alotta, NYSDOH
Michele Hamel, NYSDOH
September 17, 2019
Maurice A. John, Sr.
President
Seneca Nation of Indians
PO Box 231
Salamanca, NY 14779Dear Mr. John
The New York State Department of Health (NYSDOH) is providing notice of the State´s intent to request approval from the Centers for Medicare and Medicaid Services (CMS) for a four (4) year waiver amendment to further support the quality improvements and cost savings through the Delivery System Reform Incentive Payment (DSRIP) program. As with the original Medicaid Redesign Team (MRT) waiver, New York State seeks a continuation of DSRIP for the 1-year balance of the 1115 waiver ending on March 31, 2021 and conceptual agreement to an additional 3 years from April 2021 to March 31, 2024. Thus, the full four-year extension/renewal period (1-year extension and 3 years of renewal) would span from April 1, 2020 through March 31 , 2024.
The New York DSRIP program has already reduced Potentially Preventable Admissions through June 2018 of 21%, well on its way to the goal of 25% by the end of the demonstration. The waiver amendment seeks additional time and funding support for the community collaborations to be sustained and fully mature to successfully transition the DSRIP Promising Practices into Value Based Payment (VBP) arrangements. The State will focus on higher-value practices that are clearly aligned with federal priorities. These federal priority areas include: Substance Use Disorder (SUD) treatment and the Opioid Crisis; Serious Mental Illness and Severe Emotional Disturbance (SMI/SED); Social Determinants of Health; Primary Care Improvement and Value-Driving Payment Models.
In addition, the DSRIP promising practices would expand to certain high-need and highcost populations, such as higher-risk children and members needing long-term care. A continuation of workforce investments is essential to be responsive in meeting future needs, especially in the long-term care sector, as well as aid to financially distressed hospitals to help accelerate the transformation of acute and ambulatory health care.
The anticipated impact this demonstration would have on Tribal members includes:
- Improving patient-centered care by further sustaining the integration across physical health, behavioral health, addiction treatment, and social services in communities;
- Improving access through sustained workforce investments and aid to financially distressed hospitals; and
- Improving care for higher-risk children and Medicaid members in need of longterm care.
A draft of the amendment proposal is available for review here.
Written comments will be accepted by email at 1115waivers@health.ny.gov or by mail at the address below. All comments must be postmarked or emailed by November 4th, 2019.
NYS Department of Health
Office of Health Insurance Programs
Waiver Management Unit
99 Washington Avenue
12th Floor, Suite 1208
Albany, NY 12210We look forward to our continued collaboration.
Sincerely,
Gregory S. Allen, Director
Division of Program Development & Management
Office of Health Insurance Programscc: Sean Hightower
Vennetta Harrison
Phil Alotta, NYSDOH
Michele Hamel, NYSDOH
September 17, 2019
Charles K. Smith
Council of Trustees Chairman
Shinnecock Indian Nation
PO Box 5006
Southampton, NY 11969Dear Mr. Smith
The New York State Department of Health (NYSDOH) is providing notice of the State´s intent to request approval from the Centers for Medicare and Medicaid Services (CMS) for a four (4) year waiver amendment to further support the quality improvements and cost savings through the Delivery System Reform Incentive Payment (DSRIP) program. As with the original Medicaid Redesign Team (MRT) waiver, New York State seeks a continuation of DSRIP for the 1-year balance of the 1115 waiver ending on March 31, 2021 and conceptual agreement to an additional 3 years from April 2021 to March 31, 2024. Thus, the full four-year extension/renewal period (1-year extension and 3 years of renewal) would span from April 1, 2020 through March 31 , 2024.
The New York DSRIP program has already reduced Potentially Preventable Admissions through June 2018 of 21%, well on its way to the goal of 25% by the end of the demonstration. The waiver amendment seeks additional time and funding support for the community collaborations to be sustained and fully mature to successfully transition the DSRIP Promising Practices into Value Based Payment (VBP) arrangements. The State will focus on higher-value practices that are clearly aligned with federal priorities. These federal priority areas include: Substance Use Disorder (SUD) treatment and the Opioid Crisis; Serious Mental Illness and Severe Emotional Disturbance (SMI/SED); Social Determinants of Health; Primary Care Improvement and Value-Driving Payment Models.
In addition, the DSRIP promising practices would expand to certain high-need and highcost populations, such as higher-risk children and members needing long-term care. A continuation of workforce investments is essential to be responsive in meeting future needs, especially in the long-term care sector, as well as aid to financially distressed hospitals to help accelerate the transformation of acute and ambulatory health care.
The anticipated impact this demonstration would have on Tribal members includes:
- Improving patient-centered care by further sustaining the integration across physical health, behavioral health, addiction treatment, and social services in communities;
- Improving access through sustained workforce investments and aid to financially distressed hospitals; and
- Improving care for higher-risk children and Medicaid members in need of longterm care.
A draft of the amendment proposal is available for review here.
Written comments will be accepted by email at 1115waivers@health.ny.gov or by mail at the address below. All comments must be postmarked or emailed by November 4th, 2019.
NYS Department of Health
Office of Health Insurance Programs
Waiver Management Unit
99 Washington Avenue
12th Floor, Suite 1208
Albany, NY 12210We look forward to our continued collaboration.
Sincerely,
Gregory S. Allen, Director
Division of Program Development & Management
Office of Health Insurance Programscc: Sean Hightower
Vennetta Harrison
Phil Alotta, NYSDOH
Michele Hamel, NYSDOH
September 17, 2019
Paul O. Thompson, Chief
St. Regis Mohawk Tribe
412 State Route 37
Akwesasne, NY 13655Dear Chief Thompson:
The New York State Department of Health (NYSDOH) is providing notice of the State´s intent to request approval from the Centers for Medicare and Medicaid Services (CMS) for a four (4) year waiver amendment to further support the quality improvements and cost savings through the Delivery System Reform Incentive Payment (DSRIP) program. As with the original Medicaid Redesign Team (MRT) waiver, New York State seeks a continuation of DSRIP for the 1-year balance of the 1115 waiver ending on March 31, 2021 and conceptual agreement to an additional 3 years from April 2021 to March 31, 2024. Thus, the full four-year extension/renewal period (1-year extension and 3 years of renewal) would span from April 1, 2020 through March 31 , 2024.
The New York DSRIP program has already reduced Potentially Preventable Admissions through June 2018 of 21%, well on its way to the goal of 25% by the end of the demonstration. The waiver amendment seeks additional time and funding support for the community collaborations to be sustained and fully mature to successfully transition the DSRIP Promising Practices into Value Based Payment (VBP) arrangements. The State will focus on higher-value practices that are clearly aligned with federal priorities. These federal priority areas include: Substance Use Disorder (SUD) treatment and the Opioid Crisis; Serious Mental Illness and Severe Emotional Disturbance (SMI/SED); Social Determinants of Health; Primary Care Improvement and Value-Driving Payment Models.
In addition, the DSRIP promising practices would expand to certain high-need and highcost populations, such as higher-risk children and members needing long-term care. A continuation of workforce investments is essential to be responsive in meeting future needs, especially in the long-term care sector, as well as aid to financially distressed hospitals to help accelerate the transformation of acute and ambulatory health care.
The anticipated impact this demonstration would have on Tribal members includes:
- Improving patient-centered care by further sustaining the integration across physical health, behavioral health, addiction treatment, and social services in communities;
- Improving access through sustained workforce investments and aid to financially distressed hospitals; and
- Improving care for higher-risk children and Medicaid members in need of longterm care.
A draft of the amendment proposal is available for review here.
Written comments will be accepted by email at 1115waivers@health.ny.gov or by mail at the address below. All comments must be postmarked or emailed by November 4th, 2019.
NYS Department of Health
Office of Health Insurance Programs
Waiver Management Unit
99 Washington Avenue
12th Floor, Suite 1208
Albany, NY 12210We look forward to our continued collaboration.
Sincerely,
Gregory S. Allen, Director
Division of Program Development & Management
Office of Health Insurance Programscc: Sean Hightower
Vennetta Harrison
Phil Alotta, NYSDOH
Michele Hamel, NYSDOH
September 17, 2019
Ronald Lafrance, Jr., Chief
St. Regis Mohawk Tribe
412 State Route 37
Akwesasne, NY 13655Dear Chief Lafrance:
The New York State Department of Health (NYSDOH) is providing notice of the State´s intent to request approval from the Centers for Medicare and Medicaid Services (CMS) for a four (4) year waiver amendment to further support the quality improvements and cost savings through the Delivery System Reform Incentive Payment (DSRIP) program. As with the original Medicaid Redesign Team (MRT) waiver, New York State seeks a continuation of DSRIP for the 1-year balance of the 1115 waiver ending on March 31, 2021 and conceptual agreement to an additional 3 years from April 2021 to March 31, 2024. Thus, the full four-year extension/renewal period (1-year extension and 3 years of renewal) would span from April 1, 2020 through March 31 , 2024.
The New York DSRIP program has already reduced Potentially Preventable Admissions through June 2018 of 21%, well on its way to the goal of 25% by the end of the demonstration. The waiver amendment seeks additional time and funding support for the community collaborations to be sustained and fully mature to successfully transition the DSRIP Promising Practices into Value Based Payment (VBP) arrangements. The State will focus on higher-value practices that are clearly aligned with federal priorities. These federal priority areas include: Substance Use Disorder (SUD) treatment and the Opioid Crisis; Serious Mental Illness and Severe Emotional Disturbance (SMI/SED); Social Determinants of Health; Primary Care Improvement and Value-Driving Payment Models.
In addition, the DSRIP promising practices would expand to certain high-need and highcost populations, such as higher-risk children and members needing long-term care. A continuation of workforce investments is essential to be responsive in meeting future needs, especially in the long-term care sector, as well as aid to financially distressed hospitals to help accelerate the transformation of acute and ambulatory health care.
The anticipated impact this demonstration would have on Tribal members includes:
- Improving patient-centered care by further sustaining the integration across physical health, behavioral health, addiction treatment, and social services in communities;
- Improving access through sustained workforce investments and aid to financially distressed hospitals; and
- Improving care for higher-risk children and Medicaid members in need of longterm care.
A draft of the amendment proposal is available for review here.
Written comments will be accepted by email at 1115waivers@health.ny.gov or by mail at the address below. All comments must be postmarked or emailed by November 4th, 2019.
NYS Department of Health
Office of Health Insurance Programs
Waiver Management Unit
99 Washington Avenue
12th Floor, Suite 1208
Albany, NY 12210We look forward to our continued collaboration.
Sincerely,
Gregory S. Allen, Director
Division of Program Development & Management
Office of Health Insurance Programscc: Sean Hightower
Vennetta Harrison
Phil Alotta, NYSDOH
Michele Hamel, NYSDOH
September 17, 2019
Beverly Cook, Chief
St. Regis Mohawk Tribe
412 State Route 37
Akwesasne, NY 13655Dear Chief Cook:
The New York State Department of Health (NYSDOH) is providing notice of the State´s intent to request approval from the Centers for Medicare and Medicaid Services (CMS) for a four (4) year waiver amendment to further support the quality improvements and cost savings through the Delivery System Reform Incentive Payment (DSRIP) program. As with the original Medicaid Redesign Team (MRT) waiver, New York State seeks a continuation of DSRIP for the 1-year balance of the 1115 waiver ending on March 31, 2021 and conceptual agreement to an additional 3 years from April 2021 to March 31, 2024. Thus, the full four-year extension/renewal period (1-year extension and 3 years of renewal) would span from April 1, 2020 through March 31 , 2024.
The New York DSRIP program has already reduced Potentially Preventable Admissions through June 2018 of 21%, well on its way to the goal of 25% by the end of the demonstration. The waiver amendment seeks additional time and funding support for the community collaborations to be sustained and fully mature to successfully transition the DSRIP Promising Practices into Value Based Payment (VBP) arrangements. The State will focus on higher-value practices that are clearly aligned with federal priorities. These federal priority areas include: Substance Use Disorder (SUD) treatment and the Opioid Crisis; Serious Mental Illness and Severe Emotional Disturbance (SMI/SED); Social Determinants of Health; Primary Care Improvement and Value-Driving Payment Models.
In addition, the DSRIP promising practices would expand to certain high-need and highcost populations, such as higher-risk children and members needing long-term care. A continuation of workforce investments is essential to be responsive in meeting future needs, especially in the long-term care sector, as well as aid to financially distressed hospitals to help accelerate the transformation of acute and ambulatory health care.
The anticipated impact this demonstration would have on Tribal members includes:
- Improving patient-centered care by further sustaining the integration across physical health, behavioral health, addiction treatment, and social services in communities;
- Improving access through sustained workforce investments and aid to financially distressed hospitals; and
- Improving care for higher-risk children and Medicaid members in need of longterm care.
A draft of the amendment proposal is available for review here.
Written comments will be accepted by email at 1115waivers@health.ny.gov or by mail at the address below. All comments must be postmarked or emailed by November 4th, 2019.
NYS Department of Health
Office of Health Insurance Programs
Waiver Management Unit
99 Washington Avenue
12th Floor, Suite 1208
Albany, NY 12210We look forward to our continued collaboration.
Sincerely,
Gregory S. Allen, Director
Division of Program Development & Management
Office of Health Insurance Programscc: Sean Hightower
Vennetta Harrison
Phil Alotta, NYSDOH
Michele Hamel, NYSDOH
September 17, 2019
Roger Hill
Council Chairman
Tonawanda Seneca Indian Nation
7027 Meadville Road
Basom, NY 14013Dear Mr. Hill:
The New York State Department of Health (NYSDOH) is providing notice of the State´s intent to request approval from the Centers for Medicare and Medicaid Services (CMS) for a four (4) year waiver amendment to further support the quality improvements and cost savings through the Delivery System Reform Incentive Payment (DSRIP) program. As with the original Medicaid Redesign Team (MRT) waiver, New York State seeks a continuation of DSRIP for the 1-year balance of the 1115 waiver ending on March 31, 2021 and conceptual agreement to an additional 3 years from April 2021 to March 31, 2024. Thus, the full four-year extension/renewal period (1-year extension and 3 years of renewal) would span from April 1, 2020 through March 31 , 2024.
The New York DSRIP program has already reduced Potentially Preventable Admissions through June 2018 of 21%, well on its way to the goal of 25% by the end of the demonstration. The waiver amendment seeks additional time and funding support for the community collaborations to be sustained and fully mature to successfully transition the DSRIP Promising Practices into Value Based Payment (VBP) arrangements. The State will focus on higher-value practices that are clearly aligned with federal priorities. These federal priority areas include: Substance Use Disorder (SUD) treatment and the Opioid Crisis; Serious Mental Illness and Severe Emotional Disturbance (SMI/SED); Social Determinants of Health; Primary Care Improvement and Value-Driving Payment Models.
In addition, the DSRIP promising practices would expand to certain high-need and highcost populations, such as higher-risk children and members needing long-term care. A continuation of workforce investments is essential to be responsive in meeting future needs, especially in the long-term care sector, as well as aid to financially distressed hospitals to help accelerate the transformation of acute and ambulatory health care.
The anticipated impact this demonstration would have on Tribal members includes:
- Improving patient-centered care by further sustaining the integration across physical health, behavioral health, addiction treatment, and social services in communities;
- Improving access through sustained workforce investments and aid to financially distressed hospitals; and
- Improving care for higher-risk children and Medicaid members in need of longterm care.
A draft of the amendment proposal is available for review here.
Written comments will be accepted by email at 1115waivers@health.ny.gov or by mail at the address below. All comments must be postmarked or emailed by November 4th, 2019.
NYS Department of Health
Office of Health Insurance Programs
Waiver Management Unit
99 Washington Avenue
12th Floor, Suite 1208
Albany, NY 12210We look forward to our continued collaboration.
Sincerely,
Gregory S. Allen, Director
Division of Program Development & Management
Office of Health Insurance Programscc: Sean Hightower
Vennetta Harrison
Phil Alotta, NYSDOH
Michele Hamel, NYSDOH
September 17, 2019
Darwin Hill
Clerk
Tonawanda Seneca Indian Nation
7027 Meadville Road
Basom, NY 14013Dear Mr. Hill:
The New York State Department of Health (NYSDOH) is providing notice of the State´s intent to request approval from the Centers for Medicare and Medicaid Services (CMS) for a four (4) year waiver amendment to further support the quality improvements and cost savings through the Delivery System Reform Incentive Payment (DSRIP) program. As with the original Medicaid Redesign Team (MRT) waiver, New York State seeks a continuation of DSRIP for the 1-year balance of the 1115 waiver ending on March 31, 2021 and conceptual agreement to an additional 3 years from April 2021 to March 31, 2024. Thus, the full four-year extension/renewal period (1-year extension and 3 years of renewal) would span from April 1, 2020 through March 31 , 2024.
The New York DSRIP program has already reduced Potentially Preventable Admissions through June 2018 of 21%, well on its way to the goal of 25% by the end of the demonstration. The waiver amendment seeks additional time and funding support for the community collaborations to be sustained and fully mature to successfully transition the DSRIP Promising Practices into Value Based Payment (VBP) arrangements. The State will focus on higher-value practices that are clearly aligned with federal priorities. These federal priority areas include: Substance Use Disorder (SUD) treatment and the Opioid Crisis; Serious Mental Illness and Severe Emotional Disturbance (SMI/SED); Social Determinants of Health; Primary Care Improvement and Value-Driving Payment Models.
In addition, the DSRIP promising practices would expand to certain high-need and highcost populations, such as higher-risk children and members needing long-term care. A continuation of workforce investments is essential to be responsive in meeting future needs, especially in the long-term care sector, as well as aid to financially distressed hospitals to help accelerate the transformation of acute and ambulatory health care.
The anticipated impact this demonstration would have on Tribal members includes:
- Improving patient-centered care by further sustaining the integration across physical health, behavioral health, addiction treatment, and social services in communities;
- Improving access through sustained workforce investments and aid to financially distressed hospitals; and
- Improving care for higher-risk children and Medicaid members in need of longterm care.
A draft of the amendment proposal is available for review here.
Written comments will be accepted by email at 1115waivers@health.ny.gov or by mail at the address below. All comments must be postmarked or emailed by November 4th, 2019.
NYS Department of Health
Office of Health Insurance Programs
Waiver Management Unit
99 Washington Avenue
12th Floor, Suite 1208
Albany, NY 12210We look forward to our continued collaboration.
Sincerely,
Gregory S. Allen, Director
Division of Program Development & Management
Office of Health Insurance Programscc: Sean Hightower
Vennetta Harrison
Phil Alotta, NYSDOH
Michele Hamel, NYSDOH
September 17, 2019
Leo Henry, Chief
Tuscarora Indian Nation
2006 Mount Hope Road
Lewiston, NY 14092Dear Chief Henry:
The New York State Department of Health (NYSDOH) is providing notice of the State´s intent to request approval from the Centers for Medicare and Medicaid Services (CMS) for a four (4) year waiver amendment to further support the quality improvements and cost savings through the Delivery System Reform Incentive Payment (DSRIP) program. As with the original Medicaid Redesign Team (MRT) waiver, New York State seeks a continuation of DSRIP for the 1-year balance of the 1115 waiver ending on March 31, 2021 and conceptual agreement to an additional 3 years from April 2021 to March 31, 2024. Thus, the full four-year extension/renewal period (1-year extension and 3 years of renewal) would span from April 1, 2020 through March 31 , 2024.
The New York DSRIP program has already reduced Potentially Preventable Admissions through June 2018 of 21%, well on its way to the goal of 25% by the end of the demonstration. The waiver amendment seeks additional time and funding support for the community collaborations to be sustained and fully mature to successfully transition the DSRIP Promising Practices into Value Based Payment (VBP) arrangements. The State will focus on higher-value practices that are clearly aligned with federal priorities. These federal priority areas include: Substance Use Disorder (SUD) treatment and the Opioid Crisis; Serious Mental Illness and Severe Emotional Disturbance (SMI/SED); Social Determinants of Health; Primary Care Improvement and Value-Driving Payment Models.
In addition, the DSRIP promising practices would expand to certain high-need and highcost populations, such as higher-risk children and members needing long-term care. A continuation of workforce investments is essential to be responsive in meeting future needs, especially in the long-term care sector, as well as aid to financially distressed hospitals to help accelerate the transformation of acute and ambulatory health care.
The anticipated impact this demonstration would have on Tribal members includes:
- Improving patient-centered care by further sustaining the integration across physical health, behavioral health, addiction treatment, and social services in communities;
- Improving access through sustained workforce investments and aid to financially distressed hospitals; and
- Improving care for higher-risk children and Medicaid members in need of longterm care.
A draft of the amendment proposal is available for review here.
Written comments will be accepted by email at 1115waivers@health.ny.gov or by mail at the address below. All comments must be postmarked or emailed by November 4th, 2019.
NYS Department of Health
Office of Health Insurance Programs
Waiver Management Unit
99 Washington Avenue
12th Floor, Suite 1208
Albany, NY 12210We look forward to our continued collaboration.
Sincerely,
Gregory S. Allen, Director
Division of Program Development & Management
Office of Health Insurance Programscc: Sean Hightower
Vennetta Harrison
Phil Alotta, NYSDOH
Michele Hamel, NYSDOH
September 17, 2019
Kenneth Patterson, Chief
Tuscarora Indian Nation
1967 Upper Mountain Road
Lewiston, NY 14092Dear Chief Patterson:
The New York State Department of Health (NYSDOH) is providing notice of the State´s intent to request approval from the Centers for Medicare and Medicaid Services (CMS) for a four (4) year waiver amendment to further support the quality improvements and cost savings through the Delivery System Reform Incentive Payment (DSRIP) program. As with the original Medicaid Redesign Team (MRT) waiver, New York State seeks a continuation of DSRIP for the 1-year balance of the 1115 waiver ending on March 31, 2021 and conceptual agreement to an additional 3 years from April 2021 to March 31, 2024. Thus, the full four-year extension/renewal period (1-year extension and 3 years of renewal) would span from April 1, 2020 through March 31 , 2024.
The New York DSRIP program has already reduced Potentially Preventable Admissions through June 2018 of 21%, well on its way to the goal of 25% by the end of the demonstration. The waiver amendment seeks additional time and funding support for the community collaborations to be sustained and fully mature to successfully transition the DSRIP Promising Practices into Value Based Payment (VBP) arrangements. The State will focus on higher-value practices that are clearly aligned with federal priorities. These federal priority areas include: Substance Use Disorder (SUD) treatment and the Opioid Crisis; Serious Mental Illness and Severe Emotional Disturbance (SMI/SED); Social Determinants of Health; Primary Care Improvement and Value-Driving Payment Models.
In addition, the DSRIP promising practices would expand to certain high-need and highcost populations, such as higher-risk children and members needing long-term care. A continuation of workforce investments is essential to be responsive in meeting future needs, especially in the long-term care sector, as well as aid to financially distressed hospitals to help accelerate the transformation of acute and ambulatory health care.
The anticipated impact this demonstration would have on Tribal members includes:
- Improving patient-centered care by further sustaining the integration across physical health, behavioral health, addiction treatment, and social services in communities;
- Improving access through sustained workforce investments and aid to financially distressed hospitals; and
- Improving care for higher-risk children and Medicaid members in need of longterm care.
A draft of the amendment proposal is available for review here.
Written comments will be accepted by email at 1115waivers@health.ny.gov or by mail at the address below. All comments must be postmarked or emailed by November 4th, 2019.
NYS Department of Health
Office of Health Insurance Programs
Waiver Management Unit
99 Washington Avenue
12th Floor, Suite 1208
Albany, NY 12210We look forward to our continued collaboration.
Sincerely,
Gregory S. Allen, Director
Division of Program Development & Management
Office of Health Insurance Programscc: Sean Hightower
Vennetta Harrison
Phil Alotta, NYSDOH
Michele Hamel, NYSDOH
September 17, 2019
Harry Wallace, Chief
Unkechaug Indian Territory
2007 Poospatuck Lane
Mastic, NY 11950Dear Chief Wallace:
The New York State Department of Health (NYSDOH) is providing notice of the State´s intent to request approval from the Centers for Medicare and Medicaid Services (CMS) for a four (4) year waiver amendment to further support the quality improvements and cost savings through the Delivery System Reform Incentive Payment (DSRIP) program. As with the original Medicaid Redesign Team (MRT) waiver, New York State seeks a continuation of DSRIP for the 1-year balance of the 1115 waiver ending on March 31, 2021 and conceptual agreement to an additional 3 years from April 2021 to March 31, 2024. Thus, the full four-year extension/renewal period (1-year extension and 3 years of renewal) would span from April 1, 2020 through March 31 , 2024.
The New York DSRIP program has already reduced Potentially Preventable Admissions through June 2018 of 21%, well on its way to the goal of 25% by the end of the demonstration. The waiver amendment seeks additional time and funding support for the community collaborations to be sustained and fully mature to successfully transition the DSRIP Promising Practices into Value Based Payment (VBP) arrangements. The State will focus on higher-value practices that are clearly aligned with federal priorities. These federal priority areas include: Substance Use Disorder (SUD) treatment and the Opioid Crisis; Serious Mental Illness and Severe Emotional Disturbance (SMI/SED); Social Determinants of Health; Primary Care Improvement and Value-Driving Payment Models.
In addition, the DSRIP promising practices would expand to certain high-need and highcost populations, such as higher-risk children and members needing long-term care. A continuation of workforce investments is essential to be responsive in meeting future needs, especially in the long-term care sector, as well as aid to financially distressed hospitals to help accelerate the transformation of acute and ambulatory health care.
The anticipated impact this demonstration would have on Tribal members includes:
- Improving patient-centered care by further sustaining the integration across physical health, behavioral health, addiction treatment, and social services in communities;
- Improving access through sustained workforce investments and aid to financially distressed hospitals; and
- Improving care for higher-risk children and Medicaid members in need of longterm care.
A draft of the amendment proposal is available for review here.
Written comments will be accepted by email at 1115waivers@health.ny.gov or by mail at the address below. All comments must be postmarked or emailed by November 4th, 2019.
NYS Department of Health
Office of Health Insurance Programs
Waiver Management Unit
99 Washington Avenue
12th Floor, Suite 1208
Albany, NY 12210We look forward to our continued collaboration.
Sincerely,
Gregory S. Allen, Director
Division of Program Development & Management
Office of Health Insurance Programscc: Sean Hightower
Vennetta Harrison
Phil Alotta, NYSDOH
Michele Hamel, NYSDOH
September 17, 2019
Curtis Harris-Davia
Executive Director
American Indian Community House
39 Eldridge Street, 4th Floor
New York, NY 10002Dear Mr. Harris-Davia:
The New York State Department of Health (NYSDOH) is providing notice of the State´s intent to request approval from the Centers for Medicare and Medicaid Services (CMS) for a four (4) year waiver amendment to further support the quality improvements and cost savings through the Delivery System Reform Incentive Payment (DSRIP) program. As with the original Medicaid Redesign Team (MRT) waiver, New York State seeks a continuation of DSRIP for the 1-year balance of the 1115 waiver ending on March 31, 2021 and conceptual agreement to an additional 3 years from April 2021 to March 31, 2024. Thus, the full four-year extension/renewal period (1-year extension and 3 years of renewal) would span from April 1, 2020 through March 31 , 2024.
The New York DSRIP program has already reduced Potentially Preventable Admissions through June 2018 of 21%, well on its way to the goal of 25% by the end of the demonstration. The waiver amendment seeks additional time and funding support for the community collaborations to be sustained and fully mature to successfully transition the DSRIP Promising Practices into Value Based Payment (VBP) arrangements. The State will focus on higher-value practices that are clearly aligned with federal priorities. These federal priority areas include: Substance Use Disorder (SUD) treatment and the Opioid Crisis; Serious Mental Illness and Severe Emotional Disturbance (SMI/SED); Social Determinants of Health; Primary Care Improvement and Value-Driving Payment Models.
In addition, the DSRIP promising practices would expand to certain high-need and highcost populations, such as higher-risk children and members needing long-term care. A continuation of workforce investments is essential to be responsive in meeting future needs, especially in the long-term care sector, as well as aid to financially distressed hospitals to help accelerate the transformation of acute and ambulatory health care.
The anticipated impact this demonstration would have on Tribal members includes:
- Improving patient-centered care by further sustaining the integration across physical health, behavioral health, addiction treatment, and social services in communities;
- Improving access through sustained workforce investments and aid to financially distressed hospitals; and
- Improving care for higher-risk children and Medicaid members in need of longterm care.
A draft of the amendment proposal is available for review here.
Written comments will be accepted by email at 1115waivers@health.ny.gov or by mail at the address below. All comments must be postmarked or emailed by November 4th, 2019.
NYS Department of Health
Office of Health Insurance Programs
Waiver Management Unit
99 Washington Avenue
12th Floor, Suite 1208
Albany, NY 12210We look forward to our continued collaboration.
Sincerely,
Gregory S. Allen, Director
Division of Program Development & Management
Office of Health Insurance Programscc: Sean Hightower
Vennetta Harrison
Phil Alotta, NYSDOH
Michele Hamel, NYSDOH
September 17, 2019
Dear Colleague:
The New York State Department of Health (NYSDOH) is providing notice of the State´s intent to request approval from the Centers for Medicare and Medicaid Services (CMS) for a four (4) year waiver amendment to further support the quality improvements and cost savings through the Delivery System Reform Incentive Payment (DSRIP) program. As with the original Medicaid Redesign Team (MRT) waiver, New York State seeks a continuation of DSRIP for the 1-year balance of the 1115 waiver ending on March 31, 2021 and conceptual agreement to an additional 3 years from April 2021 to March 31, 2024. Thus, the full four-year extension/renewal period (1-year extension and 3 years of renewal) would span from April 1, 2020 through March 31 , 2024.
The New York DSRIP program has already reduced Potentially Preventable Admissions through June 2018 of 21%, well on its way to the goal of 25% by the end of the demonstration. The waiver amendment seeks additional time and funding support for the community collaborations to be sustained and fully mature to successfully transition the DSRIP Promising Practices into Value Based Payment (VBP) arrangements. The State will focus on higher-value practices that are clearly aligned with federal priorities. These federal priority areas include: Substance Use Disorder (SUD) treatment and the Opioid Crisis; Serious Mental Illness and Severe Emotional Disturbance (SMI/SED); Social Determinants of Health; Primary Care Improvement and Value-Driving Payment Models.
In addition, the DSRIP promising practices would expand to certain high-need and highcost populations, such as higher-risk children and members needing long-term care. A continuation of workforce investments is essential to be responsive in meeting future needs, especially in the long-term care sector, as well as aid to financially distressed hospitals to help accelerate the transformation of acute and ambulatory health care.
The anticipated impact this demonstration would have on Tribal members includes:
- Improving patient-centered care by further sustaining the integration across physical health, behavioral health, addiction treatment, and social services in communities;
- Improving access through sustained workforce investments and aid to financially distressed hospitals; and
- Improving care for higher-risk children and Medicaid members in need of longterm care.
A draft of the amendment proposal is available for review here.
Written comments will be accepted by email at 1115waivers@health.ny.gov or by mail at the address below. All comments must be postmarked or emailed by November 4th, 2019.
NYS Department of Health
Office of Health Insurance Programs
Waiver Management Unit
99 Washington Avenue
12th Floor, Suite 1208
Albany, NY 12210We look forward to our continued collaboration.
Sincerely,
Gregory S. Allen, Director
Division of Program Development & Management
Office of Health Insurance Programscc: Sean Hightower
Vennetta Harrison
Phil Alotta, NYSDOH
Michele Hamel, NYSDOH
Appendix F – Compliance with Public Comment Circulation Requirements
Appendix G – Glossary of Terms
ACE – Adverse Childhood Experience
ACO – Accountable Care Organization
APM – Alternative Payment Models
BHCC – Behavioral Health Care Collaboratives
CAG – Clinical Advisory Group
CBO – Community-Based Organization
CHW – Community Health Worker
CMMI – Center for Medicare & Medicaid Innovation
CMS – Center for Medicare & Medicaid Services
COC – Continuum of Care
COTI – Center Of Treatment Innovation
CQM – Clinical Quality Measure
DATA – Drug Addiction Treatment Act
DSRIP – Delivery System Reform Incentive Payment
ED – Emergency Department
EHR – Electronic Health Record
EMR – Electronic Medical Record
FFP – Federal Financial Participation
FQHC – Federally Qualified Health Center
HEDIS – Healthcare Effectiveness Data and Information Set
HH – Health Home
HITECH – Health Information Technology for Economic and Clinical Health Act
IAAF – Interim Access Assurance Fund
I/DD – Intellectual/Developmental Disabilities
IMD – Institution of Mental Disease
IMPACT – Improving Mood–Promoting Access to Collaborative Treatment
INTERACT – Interventions to Reduce Acute Care Transfers
IPA – Independent Practice Association
iPOS – Integrated Palliative Care Outcome Scale
LHD – Local Health Department
LTC – Long-Term Care
LTCPAC – Long-Term Care and Palliative Care
LTSS – Long-Term Support Services
LPN – Licensed Practical Nurse
MAPP – Medicaid Analytics and Performance Portal
MAT – Medication-Assisted Treatment
MAX – Medicaid Accelerated eXchange
MCO – Managed Care Organization
MCT – Mobile Crisis Team
MDW – Medicaid Data Warehouse
MMRB – Maternal Mortality Review Board
MRT – Medicaid Redesign Team
NYS – New York State
OASAS – Office of Addiction Services And Supports
OHIP – State Office of Health Insurance Programs
OUD – Opioid Use Disorder
P4P – Pay For Performance
P4R – Pay For Reporting
PCMH – Patient-Centered Medical Home
PCP – Primary Care Practice
PPA – Potentially Preventable Admission
PPR – Potentially Preventable Readmission
PPS – Performing Providers System
PPV – Potentially Preventable Visit
PQC – Perinatal Quality Collaborative
QE – Qualified Entity
RCCI – Rapid-Cycle Continuous Improvement
SBIRT – Screening Brief Intervention Treatment
SDHN – Social Determinant of Health Network
SDOH – Social Determinants of Health
SED – Serious Emotional Disturbance
SIM – State Innovation Model
SMI – Serious Mental Illness
SNF – Skilled Nursing Facility
SUD – Substance Use Disorder
TCN – Transitional Care Nurse
TCT – Transitional Care Team
VBP – Value-Based Payment
VMO – Value Management Organization
________________________________________
1. NYS Prevention Agenda 1
2. VMOs replace the concept of value-driving entities (VDE) from the comment period. 2
3. A link to the report from the United Hospital Fund may be accessed here 3
4. For the purposes of this paper, SDOH provider is used to represent CBOs, local health departments, social care providers and social services providers. 4
5. "CMS Administrator Seema Verma´s Speech to the National Association of Medicaid Directors in Washington, D.C." CMS, 12 Nov. 2019. 5
6. Care Management for All is a State initiative focused on having virtually all Medicaid enrollees served in care management by 2019. More information is available here. 6
7. The LACE tool has been validated by a number of studies, such as: Van Wal raven, C., et. al.. 2010. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. Canadian Medical Association Journal. 182(6), pp.551-557. Available here. 7
8. VBP Roadmap 2019 8
9. NY DOH. First 1000 Days Preventative Pediatric Care Clinical Advisory Group. Oct. 2019. 9
10. "HealthySteps." HealthySteps, ZERO to THREE, 2019. 10
11. New York State Taskforce Maternal Mortality and Disparate Racial Outcomes. Recommendations to the Governor to Reduce Maternal Mortality and Racial Disparities. Mar. 2019. 11
12. New York State Taskforce Maternal Mortality and Disparate Racial Outcomes. Recommendations to the Governor to Reduce Maternal Mortality and Racial Disparities. Mar. 2019. 12
13. New York State Taskforce Maternal Mortality and Disparate Racial Outcomes. Recommendations to the Governor to Reduce Maternal Mortality and Racial Disparities. Mar. 2019. 13
14. Provider Contract Guidelines for Article 44 MCOs, IPAs, and ACOs 14
15. Managed Long Term Care Partial Subpopulation: VBP Quality Measure Set MY 2019 15
16. New York´s 1115 Waiver Programs Public Comment Days 16
17. MRT Formal 1115 Waiver Amendment Request Submitted to the CMS. 17
18. Additional information regarding public comments are available online here. 18
19. American Indian Health Program in New York State 19
20. HHS NEWS: HHS To Deliver Value-Based Transformation in Primary Care 20
21. MPACT Act of 2014 Data Standardization & Cross Setting Measures 21
Follow Us