DSRIP Breakthrough Webinar Series
- Presentation is also available in Portable Document Format (PDF)
Jake Bowling
Assistant Vice President, Practice Improvement
Brie Reimann
Deputy Director, SAMHSA–HRSA Center for Integrated Health Solutions
The National Council for Behavioral Health
December 2015
Agenda
- Introduction to SBIRT
- Validated Screening Tools
- Brief Intervention Framework
- Referral Best Practices
- Staff Buy–in
- Workflow Redesign
- SBIRT Protocols
- NY SBIRT Resources
New York State SBIRT Introduction
What is SBIRT?
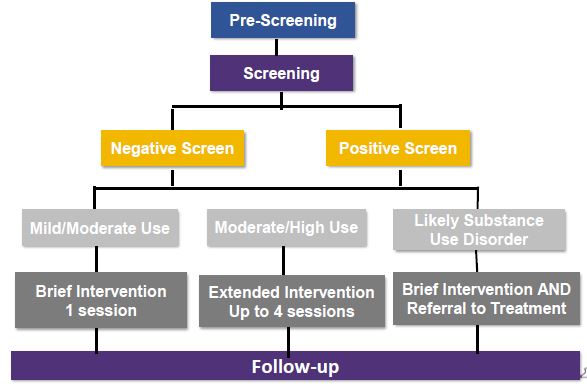
- Screening to identify patients at–risk for developing substance use disorders.
- Brief Intervention to raise awareness of risks, elicit internal motivation for change, and help set healthy goals.
- Referral to Treatment to facilitate access to specialized services and coordinate care between systems
SBIRT Decision Tree
SBIRT Paradigm Shift
- Not looking for addiction
- Looking for unhealthy substance use patterns
- Looking for opportunities for intervention
- Meeting people where they are
Screening
A systematic way of identifying potential for problems using a standardized, reliable and valid tool
Validated Screening Instruments
- AUDIT: Alcohol Use Disorder Identification Test.
- DAST: Drug Abuse Screening Test.
- CRAFFT: Car, Relax, Alone, Forget, Family or Friends, Trouble (for adolescents).
- ASSIST: Alcohol, Smoking, and Substance Abuse Involvement Screening Test.
- GAIN–SS: Global Appraisal of Individual Needs Short Screen
- NIAAAA and NIDA single question pre–screens
http://www.oasas.ny.gov/adMed/sbirt/index.cfm#screening
Screening Considerations
- When will the client be screened?
- Intake
- Clinician assessment/first interview
- Frequency of screenings after first screen – integration with counseling sessions
- Population to be screened
- Adolescents
- Adults
- Special populations
Brief Intervention
To motivate patients to be aware of their patterns of use, understand the associated risks, and make their own decisions. – CDC, 2014
Motivational Interviewing Spirit and principles = foundational skills
Brief Intervention:
The Brief Negotiated Interview Format
- Raise the subject
- Provide feedback
- Enhance motivation
- Develop a plan
Low–Risk Drinking Guidelines
| Low–risk drinking limits | MEN | WOMEN | |
|---|---|---|---|
| NIAAA, 2010 | On any single DAY |
No more than 4 drinks on any day |
No more than 3 drinks on any day |
| ** AND ** | ** AND ** | ||
| Per WEEK |
No more than 14 drinks on any week |
No more than 7 drinks on any week |
|
| To stay low–risk, keep BOTH the single–day AND weekly limits. | |||
Single Occasion Weekly Over Time
IMMEDIATE RISKS
- Pedestrian injuries
- Drowning
- Falls
- Intimate partner violence
- Depressed mood
- Homicide & suicide
- Unintended firearm injuries
- Alcohol poisoning
- Unprotected sex (leading to STI’s & unintended pregnancy)
- Assaults
- Child abuse & neglect
- Property crimes
- Fires
LONG–TERM RISKS
- Gastric distress
- Hypertension
- Cardiovascular disease
- Permanent liver damage
- Cancer
- Pancreatitis
- Diabetes
- Alcoholism
- Chronic depression
- Neurologic damage
- Fetal alcohol spectrum disorders (which include physical, behavioral, and learning disabilities)
Referral to Treatment
Common Barriers to Effective Referral to Treatment
1855 adult patients with likely dependency (Brown, 2014)
- 24% expressed initial interest in a referral
- 10% entered treatment
- Lack of evidence based practice
- Stigma
- Inadequate breadth or duration
- Lack of cultural competence
- Waiting lists
- Inadequate transportation & child care
- Treatment modality constraints
Referral to Treatment: Considerations
- Availability of resources for treatment
- Knowledge by staff on available resources
- Relationships with treatment providers
Personalize the process:
- Facilitate call to the treatment provider with patient
- Assure the appointment is made
- Assist with barriers to accessing treatment
- Avoid just handing patient "a piece of paper"
- Document referral source and date of appointment
- Follow–up and provide reminders –release of information to follow–up
Partnership Development
- Start with providers with whom you already have a relationship
- Use areas of common interest and build on those areas
- Try out new service delivery process for a short period of time and revisit.
- Introduce staff at your agency to referral partners
Key Questions
- What services are provided through your referral network?
- What is your relationship with those providers?
- Are they new partners or long–standing ones?
- Are you able to track the referral to more formal substance use treatment?
- Are you notified if a client misses a referral appointment?
Nuts and Bolts of SBIRT Implementation
Why SBIRT?
- Reduce Unhealthy Drinking
- Patients who receive BI drink less and engage in less binge drinking
- Reduce Readmissions to Trauma Centers, EDs and Hospitals
- Lower Health Care Costs
- $3.81 return for each $1 invested in SBIRT
- Improves Public Safety
- Fewer injuries, reduced impaired driving, safer community
SBIRT Implementation
- Identify a Champion and Form a Change Team
- Assess Barriers and Facilitators
- Process Mapping
- PDSA Cycles
- Ongoing Performance Monitoring
CASA Columbia
An SBIRT Implementation and Process Change Manual for Practitioners
Identifying a Champion
- Leads efforts to implement SBIRT at your agency
- Should be a team player, knowledgeable about the health care setting, enthusiastic, and well–respected
- Helps to gain buy–in from staff!!
Building the Change Team
- Leadership
- Clinical staff
- IT/ EHR staff
- Billing staff
- HR
- Training
- Office Staff
How do you communicate with key stakeholders & speak to their priorities?
Common Barriers
- Provider Attitudes and Competence
- Workflow and Resources
- SBIRT Adaptability
- Organizational Support
- Client Characteristics and Background
CASA Columbia
An SBIRT Implementation and Process Change Manual for Practitioners
Workflow Redesign
- Current vs. future state
- Maximize efficiencies
- Improve care coordination
- Shadowing, Observing and Walkthroughs
- Mapping out EHR role
Implementation Questions: Screening
- Who will conduct the screening test?
- What alcohol and/or drug screens will we use?
- How much time will it take to complete?
- What population of patients will be screened?
- Where and when will the screening take place?
- How will the information be documented and passed on?
Implementation Questions: Brief Intervention (BI)
- Who will conduct the BI?
- When and where will the BI be performed?
- How will the BI be documented in the EMR?
- Who will set up protocols to bill for SBIRT?
- What is needed to ensure that staff are properly trained?
Implementation Questions: Referral to treatment
| Identify current referral resources for follow–up Identify different types of services Work with behavioral health specialists to develop list of available service providers |
Are the available resources appropriate for your patients? Culturally and age appropriate Language and access requirements |
Utilize discharge instructions to communicate Recommendations for follow–up sessions Provide list of local service providers Pamphlets/handouts on alcohol/drug limits and consequences |
Workflow Redesign
| Patient Completes Alcohol and Drug Screen | |||
|---|---|---|---|
| ⇩ | |||
| Low/No Risk | At Risk | Moderate/High Risk | High/Severe Risk |
| ⇩ | ⇩ | ⇩ | ⇩ |
| Reinforce behavior; Monitor |
Brief Intervention Goal: Lower Risk; Reduce use to acceptable levels |
BI/Referral to tx/BT Goal: Encourage pt. to accept a referral to tx, or engage in BT |
Referral to tx. Goal: Encourage pt. to accept referral to tx, or engage in BT |
| ⇩ | |||
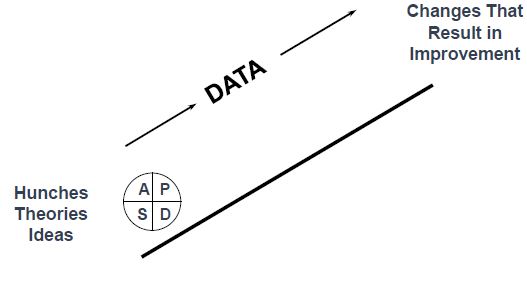
The PDSA Cycle
Act
- What changes are to be made?
- Next cycle?
Plan
- Objective
- Questions and predictions (why)
- Plan to carry out the cycle (who, what, where, when)
Do
- Carry out the plan
- Document problems and unexpected observations
- Begin analysis of the data
Study
- Complete the analysis of the data
- Compare data to predictions
- Summarize what was learned
Evaluation Measures Can Be Used to
- Identify processes that need improvement
- Assess and maintain staff competencies
- Provide data on cost effectiveness and program outcomes
- Demonstrate program success and sustainability
- Describe and quantify quality of care improvements
Repeated Use of the Cycle
Quality Improvement
- SBIRT data collection should become incorporated as a routine quality indicator
- Practices sustain ongoing SBIRT QI by:
- Identifying SBIRT measures for screening and brief intervention as part of the practice’s overall QI plan approved by leadership
- Protocol developed and approved defining:
- Specific indicators and targets (i.e. all patients at every visit will receive a screen – target 75% of patient encounters)
- Frequency of data collection
- Report format including data dictionary of all indicators
- Process for data abstraction from EHR
- Roles and responsibilities of staff for data abstraction, data monitoring, and plan of correction
- Reporting of measures to medical, administrative and board governance
SBIRT Guidelines and Protocols
- Clinical guidelines for SBIRT implementation
- Referral to treatment
- Quality improvement
- New staff on–boarding
SBIRT Guidelines and Protocols
- EHR Documentation
- Best Practice
- Billing
- Reimbursement rates are based on:
- Provider qualifications, facility type, and region
- Patient received screen, brief intervention or extended intervention
- Work directly with your billing department
- Reimbursement rates are based on:
Clinical Guidelines for SBIRT Implementation
- Defines the clinical pathway or protocol for SBIRT practice
- Identifies policy for SBIRT:
- Target population for screening and intervention
- Screening frequency
- Purpose of intervention
- Defines screening instruments
- Defines appropriate clinical responses
- Incorporates SBIRT into EHR
- Identifies staff roles and responsibilities (Champion and Change Team)
- Identifies SBIRT billing rates
Transcends transitions in leadership and staff – written and approved regardless of changes
Last step in Implementing SBIRT
- Training for SBIRT practitioners is available and recommended as the last step to implementing an SBIRT process
- Providers reimbursed under Medicaid, must complete an OASAS approved SBIRT training. Listed below are resources for approved trainings:
- Online Training
http://www.sbirttraining.com/nysbirt - In–person Training: 4 and 12 Hour Versions
http://www.oasas.ny.gov/training/providers.cfm?providerType=SBIRT4&sbirt=4
http://www.oasas.ny.gov/training/providers.cfm?providerType=SBIRT12&sbirt=12
Training, Technical Assistance and Implementation Support are Available
OASAS is a great resource to assist your PPS and network of community–based providers with planning, development and implementation of SBIRT
NYS OASAS SBIRT video link:
https://www.youtube.com/watch?v=Y5KEdMEcGts&index=2&list=PLNIxVjyAHXCPOzPqn6mNV9d4DRJ7E37e8
To inquire, please email:
SBIRTNY@oasas.ny.gov and a member of the NYS OASAS SBIRT team will contact you.
If SBIRT is part of your DSRIP project proposal and you are interested in participating in a learning collaborative with other providers, please send a separate email to:
Danielle.olsen@oasas.ny.gov
SBIRT Resources
Learn more about SBIRT implementation:
OASAS/CASA Implementation Manual:
http://www.casacolumbia.org/sites/default/files/files/An–SBIRT–implementation–and–process– change–manual–for–practitioners.pdf.
New York State Office of Alcoholism and Substance Abuse Services also offers a variety of SBIRT resources and tools:
http://www.oasas.ny.gov/AdMed/sbirt/index.cfm
DOH Guidelines for Billing Medicaid:
http://www.health.ny.gov/health_care/medicaid/program/update/2011/2011–06.htm#eme
For more resources and/or technical assistance, contact your PCG–KPMG Account Support Team via your PPS Lead
THANK YOU
Brie Reimann
brier@thenationalcouncil.org
Jake Bowling
jakeb@thenationalcouncil.org
Follow Us