Population Health Management Webinars
- Presentation is also available in Portable Document Format (PDF)
A Two–Part Webinar:
DSRIP and Population Health Introduction
DSRIP and Information Technology to Support Population Health
November, 2014
© 2012 KPMG LLP, a Delaware limited liability partnership and the U.S. member firm of the KPMG network of independent member firms affiliated with KPMG International Cooperative ("KPMG International"), a Swiss entity. All rights reserved. Printed in the U.S.A.
DSRIP Population Health Webinar
Agenda: Introduction to Population Health
- Population Health Defined
- DSRIP and population–based care
- Key components of population–based care
- Key considerations for PPS networks
Restriction on Disclosure and Use of Data – This document contains confidential or proprietary information of KPMG LLP, the disclosure of which would provide a competitive advantage to others; therefore, the recipient shall not disclose, use, or duplicate this document, in whole or in part, for any purpose other than recipient’s consideration of KPMG LLP’s proposal. This proposal is made by KPMG LLP, a Delaware limited liability partnership and the U.S. member firm of KPMG International Cooperative ("KPMG International"), and is in all respects subject to our client and engagement acceptance procedures as well as the execution of a definitive engagement letter or contract. KPMG International provides no client services. No member firm has any authority to obligate or bind KPMG International or any other member firm vis–à–vis third parties, nor does KPMG International have any such authority to obligate or bind any member firm. The KPMG name, logo and "cutting through complexity" are registered trademarks or trademarks of KPMG International.
Population Health Defined
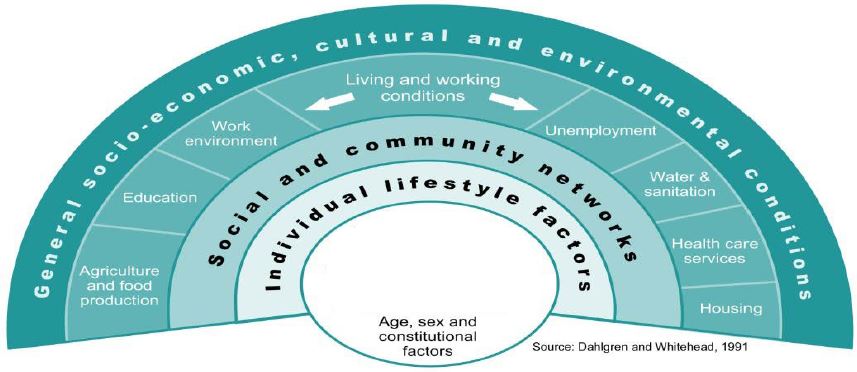
Population health is "the health outcomes of a group of individuals, including the distribution of such outcomes within the group". Medical care is one factor among many.
Population health management refers to the variety of individual, organizational and societal interventions to integrate healthcare, public health and socio–environmental determinants of health to improve health outcomes of a defined group of individuals
Population Health Management
DSRIP and Population Health
To thrive in the new value–based environment, PPSs must become high performing organizations, working together across the community, to provide a seamless continuum of coordinated, patient or "person–centered" services that are population health focused including:
- Transformation of the health care safety net at the system and state levels with near–term support for safety net providers
- Effective, safe, person–centered, timely, efficient, equitable and coordinated care
- Universal participation across the continuum
- Continuous improvement based on measurable outcomes
- The system has the "right tools" to provide a population health focus including:
- Infrastructure
- Personnel
- Payment reform
- Information Technology
DSRIP and Population Health (partial list)
Projects that specifically focus on population health include, but are not limited to Domain 4:
- 2.a.i. – Integrated Delivery System Using an Evidence–based and Population–based approach
- 2.a.iv. – Create a Medical Village Using Existing Hospital Infrastructure
- 2.b.iii. – ED Care Triage for At–Risk Populations
- 2.c.i. – To Develop a Community Based Health Navigation Service to Assist Patients to Access Healthcare Services Efficiently
- 3.a.i – Integration of Primary Care and Behavioral Health Services
- 3.b.i. – Evidence–Based Strategies for Disease Management in High Risk/Affected Populations (Adults Only)
- 3.f.i. – Increase Support Programs for Maternal and Child Health (Including High–Risk Pregnancies)
- 4.a.ii. – Prevent SA and other mental emotional disorders
- 4.a.iii. – Strengthen mental health substance abuse infrastructure
- 4.b.i. – Promote tobacco cessation
- 4.c.i. – Decrease HIV morbidity
- 4.c.ii. – Increase early access to, and retention in, HIV care
- 4.v.iii. – Decrease STD morbidity
- 4.c.iv. – Decrease HIV and STD disparities
- 4.a.i. – Promote mental, emotional, and behavioral (MEB) well–being in communities
- 4.b.ii. – Increase Access to High Quality Chronic Disease Preventative Care and Management in Both Clinical and Community Settings (Focus Area 3)
- 4.d.i. – Reduce premature births
DSRIP and Population Health Management: Key Components
NYS Prevention Agenda: Patient focus on wellness, disease and chronic care management programs
- Prevent Chronic Diseases Action Plan
- Promote a Healthy and Save Environment Action Plan
- Promote Healthy Women, Infants and Children Action Plan
- Promote Mental Health and Prevent Substance Abuse Action Plan
- Prevent HIV, STDs, Vaccine–Prevent able Diseases and Healthcare Associated Infections
These components are integral to the DSRIP projects including Domains 2, 3 and 4
These components or strategies will help your PPS achieve improved population health outcomes and cost–effectiveness
- Patient and Family – Patient–centered/Person–centered core delivery and NYS Population Health Priorities
- Organized System of Care with a Robust Infrastructure
- Identification of Population Needs Data Aggregation, Population Risk Stratification, Advanced Analytics
- Value–based Payment Practices Drive Performance
- Data–Driven Quality Measurement and Improvement
- Evidence–Based Medicine, Best Practices and Protocols
- Identification, Engagement, Outreach, Care Coordination and Care Management and Measurement
"Patient–Centered" vs. "Person Centered"
- Central to DSRIP is the consumer and their family
- Culturally, linguistically and ethnically appropriate care
- Recognizes cultural, racial, ethnic and linguistic needs and preferences
- Focus on education that promotes self–care
- Holistic approach that considers the complete needs of the patient – medical, behavioral and psychosocial – and meets them "where they are"
Key Components of Population Based Care Delivery
"Infrastructure and System–ness"
Infrastructure to support the central care delivery and leadership role of the PPS, providers and community–based supports
- Governance consistent with DSRIP requirements
- "System–ness" refers to how well the components of a system, collectively perform in achieving a common purpose
- The full continuum of care is addressed
- The PPS is structured to meet the needs of all populations and sub–populations
- Evidence–based protocols
- Data
- Care Management
- Administration
- Promotion of best practices
- Personnel
- Training
- Financial Management
- Has the PPS identified the right scale and speed to serve the greatest percentage of the population in areas (or for diagnoses) where the approach makes sense?
Determinants of Population Health
To achieve improvement in health outcomes and lower hospital use at the system and state level, PPSs will need to focus on population health with starting point to understand
- Population segment size and location
- Age Mix–Gender Mix
- Racial and Ethnicity Mix
- Previously Insured or Not (private or public coverage)
- Disease Load and Healthcare Utilization Experience
- Mix of Chronic vs. Acute Conditions (e.g. Diabetes and its complications, COPD, Heart Failure, Cancers vs. Injuries, Infections, Self–Limiting Conditions)
- Behavioral Health Conditions
- Relative Severity of Illness (driving the types and levels of interventions and care settings)
DSRIP and Population Health Management: Key Components (cont.)
Use the Community Needs Assessment (CNA) to select the highest priority DSRIP projects based on population needs
- Use broad data sources: Data books on the DOH website; regional results for metrics that will be utilized to assess PPS outcomes; LHD CNAs in conjunction with the NYS Prevention Agenda (full population)
- Identify and characterize health care resources
- Identify the main health and health service challenges facing the community
- Describe the relationship between the assessment and the projects selected?
The ability to clearly justify your population–based (and all other) DSRIP projects using data from your CNA accounts for a significant portion of the total possible points for each project.
| Community Need Identification # | CNA Title | Brief Description | Supporting Data |
|---|---|---|---|
| CNA 18 | High Diabetes prevalence | High diabetes prevalence |
|
| CNA 8 | Limited EHR linkages | Providers are unable to share patient information due to limited interconnectivity, limiting the PPS´s ability to deliver a population based approach | While some providers have joined RHIOs, they do not currently comply with state standards for information sharing as currently being developed. Survey of PPS members indicates that:
|
Organizational Application, page 15: Summary of CNA Findings
Key Components of Population Based Care Delivery (cont.)
Engagement and Outreach of Populations Identified
How do you outreach and engage Medicaid consumers?
- Outreach
- Direct communications with the member (e.g. F2F, mail, electronic or telephonic using claim or referral data)
- Escalation if the member doesn´t respond (e.g. letters to follow calls if no contact is made)
- Meet them "where they are"
- "No wrong door"
- Homeless individuals
- In the community
- Using motivational coaching
Data–Driven Quality Measurement and Improvement
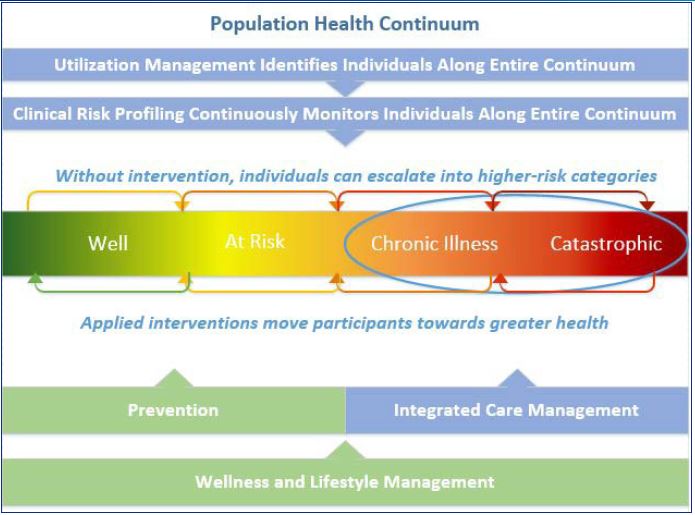
- Data must be aggregated across the population
- Data must be risk stratified to inform population needs
- Data is shared on population–based outcomes at the aggregate level, at the group level and for individual provider outcomes
- Data is stratified: by chronic condition (e.g. Serious Mental Illness + X co–morbid conditions; by race, ethnicity and primary language, by income strata)
- Data informs population health (e.g. gaps in care, outreach, registries) to identify opportunities to close gaps and improve quality overall
- The system values continuous learning and benchmarking of results; "defects" are seen as opportunities
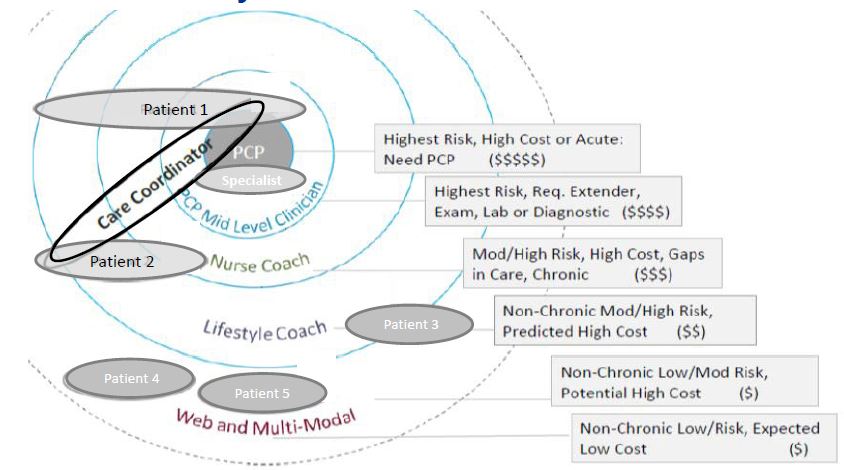
Care Management and Care Coordination
- Multidisciplinary approach across the full population and the full continuum to:
- Identify and track (e.g. Advanced Population Analytics, risk stratification, patient registries)
- Outreach (e.g. automated, telephonic and in–person)
- Assess needs (e.g. evidence–based assessment tools)
- Plan for care delivery (e.g. electronic care plans)
- Deliver care (e.g. using shared Electronic Health Records, patient and provider portals, remote patient monitoring, telemedicine, referral tracking)
- Evaluate outcomes
- Some key elements of a population–based approach include:
- Ability to address complex multi–morbid needs
- Motivational interviewing/Health coaching and self–care
- Shared decision–making
- Single plan of care across settings and providers including non–medical supports and community–based care
Value–based Payment Practice Will Drive Performance
Evidence–Based Protocols and Best Practices
Practical decisions made should: (1) be based on research studies and (2) that these research studies are selected and interpreted according to some specific norms characteristic for EBP. Typically such norms consider quantitative studies according to a narrow set of criteria of what counts as evidence.
- Take a population–based approach and consider consumer needs
- Consider racial, ethnic and linguistic adaptations
- Seek out best practices nationally with data behind them
- Design adaptations and implementation strategies with your providers to achieve buy–in and identify champions
Information Technology to identify, track and inform providers re: performance
- Meaningful Use IT, rigorous analysis and evidence–based assessment Aids in clinical decision–making support patient care, improved safety and prescribing patterns
- Tools and technology that support sharing of information are highly valued:
- Electronic Health Records (EHR)
- Patient Registries
- Health Information Exchange (HIE)
- Risk stratification tools
- Automated outreach
- Patient and provider portals
- Remote patient monitoring
- Advanced population analytics
- Telehealth/telemedicine
- Referral tracking
DSRIP Application Guidance
- Understand population health needs based on Community Needs Assessment data
- Respond to the specific requirements for each project with an eye toward population health
- Describe how and what your PPS will do – don´t just say you will meet the requirements
- Answer the question with an eye toward population health – no more and no less
- Participate in a webinar on IT and Population Health by the DSRIP Support Team, available shortly
Disclaimer
This document was prepared by the Delivery System Redesign Incentive Payment (DSRIP) Support Team (DST). The advice, recommendations and information in the document included with this notice were prepared for the sole benefit of the New York State Department of Health, based on the specific facts and circumstances of the New York State Department of Health, and its use is limited to the scope of KPMG´s engagement as DST for the New York State Department of Health. It has been provided to you for informational purposes only and you are not authorized by KPMG to rely upon it and any such reliance by you or anyone else shall be at your or their own risk. You acknowledge and agree that KPMG accepts no responsibility or liability in respect of the advice, recommendations or other information in such document to any person or organization other than the New York State Department of Health. You shall have no right to disclose the advice, recommendations or other information in such document to anyone else without including a copy of this notice and, unless disclosure is required by law or to fulfill a professional obligation required under applicable professional standards, obtaining a signed acknowledgement of this notice from the party to whom disclosure is made and you provide a copy thereof to New York State Department of Health. You acknowledge and agree that you will be responsible for any damages suffered by KPMG as a result of your failure to comply with the terms of this notice.
Follow Us