Community First Choice Option
Managed Care Organization Training
Recipient Restriction Exemption Codes for
Community First Choice Option
January 2019
Agenda
- Introduction
- CFCO Services
- CFCO Eligibility Criteria
- CFCO Recipient Restriction Exception (RR/E) Overview
- CFCO RR/E Roles and Responsibilities
- Activity Steps: CFCO Eligibility Criteria Determination
- Activity Steps: Does Meet CFCO Eligibility Requirement
- Activity Steps: Does Not Meet CFCO Eligibility Requirement
- Activity Steps: RR/E File Layout Submission
- Activity Steps: RR/E Placement – CF CO RRE Code
CFCO Services
- Current CFCO Services:
- Consumer Directed Personal Assistance Services (CDPAS)
- Home Health Aide
- Homemaker/Housekeeper (Personal Care Level 1)
- Personal Care Level 2
- Personal Emergency Response System (PERS)
- Non–Emergency Medical Transportation (NEMT)
- Additional CFCO Services Available July 1, 2019:
- Assistive Technology (AT)
- Environmental Modification (E–Mod)
- Vehicle Modification (V–Mod)
- Moving Assistance
- Community Transitional Services (CTS)
- Skill Acquisition Maintenance and Enhancement (SAME)
- Home Delivered/Congregate Meals
CFCO Eligibility Criteria
- An individual eligible to receive CFCO services must:
- Be Medicaid eligible for community coverage with community–based long term care (with or without a spend down) or be Medicaid eligible for coverage of all care and services;
- Have an assessed institutional level of care; and
- Reside in his/her own home, or the home of a family member.
- An individual´s Medicaid eligibility may not be dependent on:
- Spousal impoverishment post–eligibility rules;
- The Special Income Standard for Housing Expenses; or
- Family–of–one budgeting for a child participating in a HCBS waiver (State is seeking CMS approval to allow family–of–one children under the proposed consolidated Children´s 1915(c) Waiver to be eligible for CFCO services).
- All services must be offered to all eligible individuals across the disability spectrum.
- Recipients may participate in waiver programs and receive other State Plan services and supports as long as they are not duplicative.
- The CFCO services will be available in Medicaid Fee–for–Service (FFS) and in the Managed Care benefit packages (Mainstream Medicaid, Managed Long Term Care, Medicaid Advantage Plus, and Programs of All–Inclusive Care for the Elderly).
NOTE: Individuals enrolled in current 1915(c) waivers who may not meet CFCO eligibility criteria but do meet the waiver program criteria, will continue to access these services under the authority of the 1915(c) waiver.
All CFCO Services Must be Provided in a Home or Community Based Setting
- All CFCO services must be provided in a home or community–based setting
- All CFCO services must be provided in settings that comply with 42 CFR §441.530
- Settings include the individual´s own home or a family member´s home that meet the settings criteria outlined in 42 § CFR 441.530
- Settings do not include a nursing facility, a hospital providing long–term care services, an institution for mental disease, an intermediate care facility for individuals with an intellectual disability or related condition, or a setting with the characteristics of an institution
- Settings do not include a provider–owned or controlled residence
- Home and Community Based Services (HCBS) recipients must live in compliant settings, regardless of where the services are provided
- Must follow New York´s Statewide Transition Plan for HCBS Settings (approved by CMS on November 18, 2018)
CFCO Recipient Restriction Exception (RR/E) Overview
CFCO eligible individuals must be identified in the eMedNY system through a unique Recipient Restriction/Exemption (RR/E) code on the individual´s eligibility file. For individuals deemed eligible for CFCO, RR/E code placement started on April 1, 2018.
Two (2) RR/E Codes were created to identify CFCO eligible individuals. The CFCO RR/E Codes are ´CF´ and ´CO´ and contain the following system attributes:
- CF: Community First Choice Option (Non OPWDD)
- Short Description: ´CFCO´
- Long Description: COMMUNITY FIRST CHOICE OPTION (Non OPWDD)
- CO: Community First Choice Option (OPWDD)
- Short Description: ´CFCO–OPWDD´
- Long Description: COMMUNITY FIRST CHOICE OPTION OPWDD
With the addition of the ´CF´ and ´CO´ RR/E codes, eMedNY system edits were created based on CFCO criteria. These include:
- Specific RR/E codes cannot co–exist with a ´CF´ or ´CO´ (RR/E to RR/E Conflict);
- Specific RR/E codes can only exist with a ´CF´ or a ´CO´ based on populations;
- CF RR/E code cannot co–exist with a ´CO´ RR/E at the same time;
- Only specific Medicaid Eligibility Coverage Codes that meet the CFCO Medicaid eligibility are allowed to co–exist with a CFCO RR/E code; and
- Begin date for CFCO RR/E code cannot be prior to April 1, 2018.
- The ´CF´ or ´CO´ RR/E code on the individual´s eligibility file in eMedNY does not have an impact on the processing and payment of valid claims.
- The placement and/or update of the CFCO RR/E code can be completed through eMedNY Thin Client or through a New York Medicaid Choice (NYMC) batch file process.
- MCOs do not have access to EMedNY Thin Client and must utilize the NYMC batch file transmittal process to have the ´CF´ or ´CO´ RR/E code added to an individual´s eligibility file in eMedNY.
CFCO RR/E Roles and Responsibilities
- MCOs are responsible for implementing any necessary changes to their current processes and procedures to include the placement and maintenance of CF/CO RR/E code on an enrollee´s eligibility file.
- MCOs are responsible for updating their processes for both existing and new enrollees* who are in receipt of Long Term Services and Supports (LTSS), who are identified as part of a special population, or upon the enrollee´s request for CFCO services. This includes updates for:
- CFCO eligibility determination and
- The placement and maintenance of the ´CF´ and ´CO´ RR/E code on the enrollee´s eligibility file (NYMC batch file process).
- MCOs are responsible for transmitting the file, via the batch file process, to NYMC on at least a weekly basis.
*Except enrollees with RR/E 60/81 codes
Nursing Home Transition and Diversion (NHTD) or Traumatic Brain Injury (TBI): (RR/E 60/81 code)
MCO enrollees seeking participation in the Nursing Home Transition and Diversion (NHTD) or Traumatic Brain Injury (TBI) waivers must meet the nursing facility level of care to qualify for participation in the waivers. The Local Department of Social Services (LDSS) will be responsible for the placement of the ´CF´ RR/E code on the enrollee´s eligibility file. The LDSS, upon receipt of the Notice of Decision (NOD) Authorization from the Regional Resource Development Center (RRDC), is responsible for placing the waiver RRE code of 60 or 81 on the client´s file. In addition, the LDSS will now add the CF RRE code if the waiver participant meets CFCO eligibility and housing requirements.
Office for People With Developmental Disabilities (OPWDD) – ´CO´ RR/E
- Individuals are coded ´CO´ when determined to meet Intermediate Care Facilities for Individuals with Intellectual Disabilities (ICF/IID) level of care criteria, meet all other CFCO eligibility criteria, and are approved to receive at least some CFCO services from providers overseen by OPWDD.
- For this implementation of CFCO, OPWDD will add the ´CO´ RRE code to all eligible OPWDD individuals.
- This will include OPWDD individuals currently enrolled in MMC plans.
- Going forward, MMC plans will have the ability to add the ´CO´ RRE code to CFCO eligible OPWDD individuals enrolling in MMC using the established process. To be eligible for ´CO´ determination, the individual must have an active RRE code of 95 (OPWDD determined).
- Individuals already tagged with the OPWDD ´CO´ code can be identified in the ePACES eligibility response.
- OPWDD performs a ´CO´ RR/E upload on a monthly basis.
Note: MLTC enrollees will be coded with a ´CF´ RR/E code only.
|top of page|CFCO and NYSoH Individuals
NYSoH:
Individuals requesting CFCO services who are in receipt of NYSoH Medicaid and who are not enrolled in a Medicaid Managed Care (MMC) plan must enroll in a MMC (unless otherwise excluded).
The State is currently working on a process to assist the LDSS in transitioning Medicaid coverage for individuals who are excluded from enrollment into an MMC but otherwise eligible for CFCO services.
|top of page|Consolidated Children´s Waiver RR/E Codes
| RE code | RE code Description |
|---|---|
| K1 | HCBS LOC |
| K3 | HCBS Serious Emotional Disturbance (SED) |
| K4 | HCBS Medically Fragile (MF) |
| K5 | HCBS Developmentally Disabled (DD) |
| K6 | HCBS Developmentally Disabled and Medically Fragile (DD & MF) |
Note: This is not an all–inclusive list of K RR/E codes.
Upcoming Children´s Waiver and CFCO Services Training will be conducted on February 13, 2019.
CFCO and Consolidated Children´s Waiver Allowable RR/E Combinations
| RR/E | CF | CO | Justification |
|---|---|---|---|
| K1 (HCBS LOC) | Y | N | Consumers enrolled in the Children´s Waiver may be eligible for CFCO. DOH and the LDSS will be responsible for connecting these consumers to CFCO, unless the child is enrolled in MMC plan. |
| K3 (HCBS SED) | Y | N | |
| K4 (HCBS MF) | Y | N | |
| K5 (HCBS DD) | Y | N | |
| K6 (HCBS MF/DD) | Y | N |
CFCO and CCO/HH
People First Care Coordination Organization Health Homes (CCO/HHs) are designated to serve individuals with I/DD
- OPWDD uses the following RR/E codes for the CCO/HHs:
RR/E Description I5 CCO/HH Enrollment Level 1 I6 CCO/HH Enrollment Level 2 I7 CCO/HH Enrollment Level 3 I8 CCO/HH Enrollment Level 4 I9 CCO/Basic HCBS Plan Support - I5–I9 can only co–exist with a ´CO´ RR/E code (to be loaded by OPWDD).
- CCO/HH is responsible for the plan of care.
- OPWDD provider contact information: https://opwdd.ny.gov/sites/default/files/documents/CCO_Coverage_Chart.pdf
Activity Steps: CFCO Eligibility Criteria Determination
CFCO Eligibility Criteria Determination
MCOs are required to review an enrollee´s eligibility file, which will be utilized during the CFCO eligibility determination steps and placement of the CFCO RR/E code. MCOs must follow their existing process to review an enrollee´s eligibility file.
Note: CFCO has no impact on the current Medicaid eligibility determination process. To be eligible for CFCO, an individual must be Medicaid eligible for community coverage with community–based long term care (with or without a spend down) or be Medicaid eligible for coverage of all care and services. However, an individual´s Medicaid eligibility may not be dependent on:
- Spousal impoverishment post–eligibility rules;
- The Special Income Standard for Housing Expenses; or
- Family–of–One budgeting for a child participating in an HCBS waiver.
The State is currently working on a process for identifying individuals whose Medicaid eligibility is dependent on Spousal Impoverishment Post–Eligibility Rules and the Special Income Standard for Housing Expenses that impact MLTC enrollees.
- Review enrollee´s eligibility file for an active KK RR/E code during the applicable timeframe.
- If the enrollee does not have an active KK RR/E code during the applicable timeframe, proceed to step 2.
- If the enrollee has an active KK RR/E code during the applicable timeframe, proceed to Activity Steps: Does Not Meet CFCO Eligibility Requirement.
RR/E Code RR/E Description KK CHILD IS ELIGIBLE FOR MEDICAID AS FAMILY OF ONE
- Determine whether or not the individual meets the CFCO residential requirement.
- If enrollee meets the CFCO residential requirement, proceed to step 3.
- If enrollee does NOT meet the CFCO residential requirement, proceed to Does Not Meet CFCO Eligibility Requirement.
- All CFCO services must be provided in a home or community–based setting
- All CFCO services must be provided in settings that will comply with 42 CFR §441.530
- Settings include the individual´s own home or a family member´s home that meets the settings criteria outlined in 42 § CFR 441.530
- Does not include a nursing facility, hospital providing long–term care services, institution for mental disease, intermediate care facility for individuals with an intellectual disability or related condition, or setting with the characteristics of an institution
- Does not include provider–owned or controlled residential settings
- HCBS recipients must live in compliant settings, regardless of where services are provided
- Must follow New York´s Statewide Transition Plan for HCBS Settings (approved by CMS on November 18, 2018)
- Based on determination that an enrollee meets the CFCO residential requirement, review enrollee´s eligibility file for an active N1 – N9 RR/E.
- If there is an incorrect/outdated active RR/E N – code, MCOs must coordinate with nursing home facility to ensure that the proper form is sent to the LDSS. Proceed to step 4.
Note: The LDSS will follow their current process to review the N Code and update accordingly. MCOs will need to place the CFCO code on eligible enrollees once the N Code has been updated. The process to update/remove an inaccurate N code MUST NOT delay CFCO service authorization if the individual is otherwise found eligible for CFCO services. - If no active N Code, proceed to step 4.
- If there is an incorrect/outdated active RR/E N – code, MCOs must coordinate with nursing home facility to ensure that the proper form is sent to the LDSS. Proceed to step 4.
- If the enrollee meets the CFCO residential requirement, review enrollee´s eligibility file for an active 38, 48, or 49 RR/E code during the applicable timeframe.
- If the 38, 48, or 49 RR/E code is active and during the applicable timeframe, contact the OPWDD´s Revenue Support Field Office (RSFO) to determine if the coding is accurate.
- If the RSFO determines the 38,48, or 49 is not accurate, the RSFO updates the applicable RR/E code and informs the MCOs. Once completed, proceed to step 5.
Note: The process to remove an inaccurate 38,48, or 49 code MUST NOT delay CFCO service authorization if the enrollee is found eligible for CFCO services.
If the RSFO determines the 38,48, or 49 is accurate, the enrollee is not eligible for CFCO. Proceed to Activity Step: Does Not Meet CFCO Eligibility Requirement.
- If the RSFO determines the 38,48, or 49 is not accurate, the RSFO updates the applicable RR/E code and informs the MCOs. Once completed, proceed to step 5.
- If no active 38, 48, or 49 RR/E code and during the applicable time frame is identified on the enrollee´s eligibility file, proceed to step 5.
- If the 38, 48, or 49 RR/E code is active and during the applicable timeframe, contact the OPWDD´s Revenue Support Field Office (RSFO) to determine if the coding is accurate.
- Review enrollee´s eligibility file to determine whether or not the enrollee´s ICF/IID level of care (LOC) has already been determined by OPWDD or if enrollee should be referred to OPWDD for a LOC determination.
- If the RR/E N code is active and during the applicable timeframe, the code will need to be reviewed and a determination made.
- If the enrollee has an active RR/E code of 95 during the applicable timeframe, proceed to Activity Steps: Does Meet CFCO Eligibility Requirement.
- If the enrollee does not have an active 95 RR/E code and it appears the enrollee may benefit or qualify for OPWDD services, contact (telephone call) the applicable DDRO for OPWDD and CFCO eligibility.
- If the enrollee does not meet the criteria listed in 5.a – 5.b, proceed to step 6.
- If the RR/E N code is active and during the applicable timeframe, the code will need to be reviewed and a determination made.
- Review enrollee´s eligibility file to determine whether or not the enrollee is a 1915c waiver program participant and whether or not the LOC has already been determined.
- If the enrollee has an active 60 or 81 RR/E code (within the current date range), the enrollee meets CFCO LOC eligibility. No further action is needed for the placement of the CFCO RR/E Code. (LDSS is responsible for placing and maintaining CFCO RR/E code.)
- If the enrollee has one of the RR/E codes in the table below active within the current date range, the enrollee meets CFCO LOC eligibility. Proceed to Does Meet CFCO Eligibility Requirement.
- If the enrollee does not have one of the RR/E code in the table below as active, proceed to step 7.
RR/E Code RR/E Description CF/CO 62 CAH I CLIENT CF 63 CAH II CLIENT CF 72 BRIDGES TO HEALTH SERIOUSLY EMOTIONALLY DISTRUBED (B2H) CF 73 BRIDGES TO HEALTH SERIOUSLY DEVELOPMENTALLY DISABLE (B2H DD) CF 74 BRIDGES TO HEALTH MEDICALLY FRAGILE (B2H MEDF) CF - Determine whether or not LOC determination has been completed within six months.
- If a LOC assessment has been completed within the last six months and the LOC is 5 or greater, the enrollee meets the CFCO LOC requirement. Proceed to Does Meet CFCO Eligibility Requirement.
- If a LOC assessment has been completed and LOC is NOT 5 or greater, the enrollee does not meet the CFCO LOC requirement. Proceed to Does Not Meet CFCO Eligibility Requirement.
- If a current LOC does NOT exist or has not been completed within the last six months, utilize existing process to arrange for appropriate assessment of the enrollee.
- If the assessment confirms the LOC is 5 or greater, the enrollee meets the CFCO LOC requirement. Proceed to Does Meet CFCO Eligibility Requirement.
- If the assessment confirms the LOC is less than 5, the enrollee does NOT meet the CFCO LOC requirement. Proceed to Does Not Meet CFCO Eligibility Requirement.
Activity Steps: Does Meet CFCO Eligibility Requirement
Does Meet CFCO Eligibility Requirement
If the enrollee requested a CFCO services and was determined to be eligible for CFCO services,
- Inform the enrollee that CFCO requires a LOC reassessment every 6 months unless their case has been authorized for annual assessment.
- Determine CFCO service authorization path, and follow existing process.
- Review enrollee´s eligibility file to determine if the enrollee is enrolled in Care Coordination Organization/Health Home (CCO/HH).
Note: If the enrollee has an active I5 to I9 RR/E codes s/he is enrolled in a CCO/Health Home. The following steps must be completed:- Notify the enrollee´s CCO/HH Care Manager that the requested CFCO service has been authorized in order to continue the enrollee´s care planning.
- https://opwdd.ny.gov/sites/default/files/documents/CCO_Coverage_Chart.pdf
- Note: The CCO/HH maintains the plan of care.
- Notify the enrollee´s CCO/HH Care Manager that the requested CFCO service has been authorized in order to continue the enrollee´s care planning.
- Update plan of care to include CFCO eligibility determination, if applicable.
- Determine whether or not a physician´s order is on file and active, if applicable.
- Proceed to Activity Steps: CF RR/E File Layout and Submission.
Activity Steps: Does Not Meet CFCO Eligibility Requirement
Does Not Meet CFCO Eligibility Criteria
If the enrollee requested a CFCO service:
- Issue Notice of Determination.
- Notice must be provided to the enrollee and, if applicable, the enrollee´s designated representative.
- A copy of the notice must be maintained in the enrollee´s case record.
- Services available under an alternate State Plan or waiver authority should be initiated, as appropriate, for the individual using existing processes.
For all enrollees who do not meet CFCO eligibility criteria:
- Review enrollee´s eligibility file for ´CF´ or ´CO´ RR/E code.
- If an active CFCO RR/E code, proceed to add enrollee to weekly batch file to update CFCO RR/E code appropriately.
- If no active CFCO RR/E code, no further action is needed.
Activity Steps: RR/E File Layout Submission
RR/E File Submission Process
Medicaid Managed Care (MMC) and Managed Long Term Care (MLTC) plans are responsible for identifying CFCO eligible enrollees and are also required to create and transmit the enrollee CFCO RR/E data via a transmittal to New York Medicaid Choice (NYMC).
- Create File Layout: MMC and MLTC plans are expected to follow the designated file layout in submitting the RRE request.
| Field Title | Length | Start | End | Field Description | Required |
|---|---|---|---|---|---|
| Client ID | 8 | 1 | 8 | CLIENT.CLNT_CIN | Y |
| Restriction Code | 2 | 9 | 10 | CF or CO code | Y |
| Start Date | 8 | 11 | 18 | YYYYMMDD | Y |
| End Date | 8 | 19 | 26 | YYYYMMDD | Y |
| Transaction Entry Date | 8 | 27 | 34 | sysdate | Y |
| Filler | 4 | 35 | 38 | –– | Y |
| County Code | 2 | 39 | 40 | County Code | Y |
| Plan Code | 2 | 41 | 42 | Plan Code | Y |
| Filler | 407 | 43 | 450 | –– | Y |
The naming convention for the file submitted by the MCOs will be
2CharacterPlanCodeYYYYMMDDCUCounter.txt
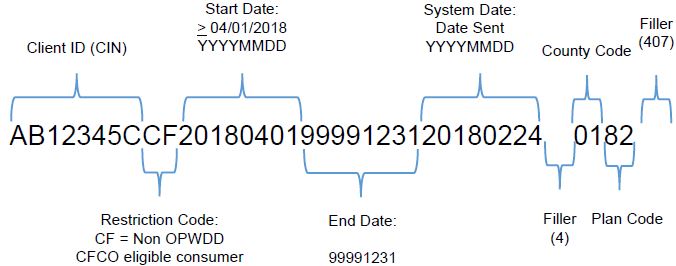
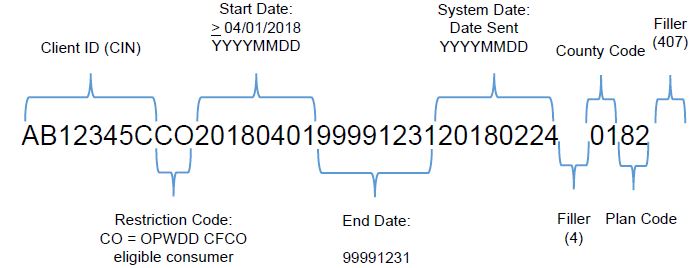
RR/E File Submission Process – File Layout
The below file layout will be utilized:
Client ID: Enter Client Identification Number (CIN)
- Format: 2 alphas, 5 numbers, 1 alpha
- Rules: Must be capitalized AB12345C
Restriction Code: Select ´CF´ or ´CO´
- Format: ´CF´ or ´CO´
- Rules: Must be Capitalized ´CF´ or ´CO´
Start Date: Enter date enrollee became eligible for CFCO
- Format: YYYYMMDD
- Rules: Must be ≥ 2018040
| Field Title | Length | Start | End | Field Description | Required |
|---|---|---|---|---|---|
| Client ID | 8 | 1 | 8 | CLIENT.CLNT_CIN | Y |
| Restriction Code | 2 | 9 | 10 | CF or CO code | Y |
| Start Date | 8 | 11 | 18 | YYYYMMDD | Y |
| End Date | 8 | 19 | 26 | YYYYMMDD | Y |
| Transaction Entry Date | 8 | 27 | 34 | sysdate | Y |
| Filler | 4 | 35 | 38 | –– | Y |
| County Code | 2 | 39 | 40 | County Code | Y |
| Plan Code | 2 | 41 | 42 | Plan Code | Y |
| Filler | 407 | 43 | 450 | –– | Y |
End Date: Enter applicable date
- Format: YYYYMMDD
- Rules:
- Enter 99991231 for CFCO eligible enrollees
- Enter date enrollees was no longer eligible for CFCO in the correct format
Transaction Entry Date: YYYYMMDD
- Date of submission to NYMC (system default)
Filler: Length 4
| Field Title | Length | Start | End | Field Description | Required |
|---|---|---|---|---|---|
| Client ID | 8 | 1 | 8 | CLIENT.CLNT_CIN | Y |
| Restriction Code | 2 | 9 | 10 | CF or CO code | Y |
| Start Date | 8 | 11 | 18 | YYYYMMDD | Y |
| End Date | 8 | 19 | 26 | YYYYMMDD | Y |
| Transaction Entry Date | 8 | 27 | 34 | sysdate | Y |
| Filler | 4 | 35 | 38 | –– | Y |
| County Code | 2 | 39 | 40 | County Code | Y |
| Plan Code | 2 | 41 | 42 | Plan Code | Y |
| Filler | 407 | 43 | 450 | –– | Y |
County Code: Enter the two (2) digit county code associated with the district of fiscal responsibility (DFR) for the enrollee.
- Format: 00
- Rules: If the client resides in NYC counties (58, 59, 60, 61, & 62), enter county code 66
Plan Code: Enter unique two (2) digit plan code
- Format: 00
- Rules: To locate applicable Plan Codes refer to Managed Care Information document located here.
Filler: Length 407
| Field Title | Length | Start | End | Field Description | Required |
|---|---|---|---|---|---|
| Client ID | 8 | 1 | 8 | CLIENT.CLNT_CIN | Y |
| Restriction Code | 2 | 9 | 10 | CF or CO code | Y |
| Start Date | 8 | 11 | 18 | YYYYMMDD | Y |
| End Date | 8 | 19 | 26 | YYYYMMDD | Y |
| Transaction Entry Date | 8 | 27 | 34 | sysdate | Y |
| Filler | 4 | 35 | 38 | –– | Y |
| County Code | 2 | 39 | 40 | County Code | Y |
| Plan Code | 2 | 41 | 42 | Plan Code | Y |
| Filler | 407 | 43 | 450 | –– | Y |
File Layout Example: Non OPWDD
File Layout Example: OPWDD
RR/E File Submission Process
Transmit File Layout: On a weekly basis, MCOs are expected to transmit to NYMC newly CFCO eligible enrollees and any updates to existing CFCO RR/E on an enrollee´s eligibility file.
NYMC Role: NYMC receives the files and combines the submission from all MCOs on a daily basis and submits to eMedNY on behalf of the MCO.
- NYMC will act as a middle agent (data passing) and is not responsible for trouble shooting with MCOs.
- MCOs should not be submitting RR/E updates for the same enrollee at the same time. However, should that occur, NYMC will submit these requests in the daily file and allow eMedNY to perform the edits on duplication.
RR/E File Layout and Submission
Receive File and Systematically Review
eMedNY systematically reviews the data and provides a response file. The response file is transmitted through NYMC who routes the response file back to the submitting MCO. The return file will include an acceptance or a rejection for the original MCO to review.
- For enrollee data that eMedNY has accepted, the enrollee´s file will be updated with the submitted RRE code. The RRE code will be viewable on ePACES.
Review Response File:
Upon the receipt of the processing result from eMedNY, NYMC will return the RRE responses back to individual MCOs.
- MCOs are responsible to review and work the responses accordingly to eMedNY´s RR/E guidelines.
Review Response File:
MCOs are responsible for reviewing the response file and determining if the data was accepted:
- If the response file is accepted no further action is needed. Example:
- If the enrollee data is rejected the MCO plan is responsible for reviewing the RRE edit code (RRE Edit Manual) and updating the file.
- Example:
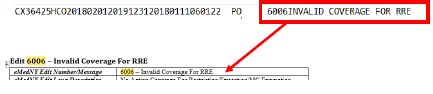
RR/E Edit Responses
Edit 6004 – Duplicate RR/E Exists: This occurs when the enrollee already has the same CFCO RR/E code on the eligibility file for the same or overlapping date of service.
Edit 6027 – Trans District Not Valid per Data Dictionary: To avoid this edit ensure that the Plan Code is entered into the file layout. To locate applicable Plan Code refer to Managed Care Information document located at: here.
Edit 6005 – RR/E to RR/E Conflict: The State has identified specific RR/E codes that cannot co–exist with a CFCO RR/E based on the CFCO eligibility requirements.
| Conflict RR/E Code | RR/E Description | RR/E Conflict Review |
|---|---|---|
| 38 | ICF/DD RESIDENT | Does NOT Meet CFCO Residential Requirement |
| 48 | SUPPORTIVE IRA´S AND CR´S | |
| 49 | SUPERVISED IRA AND CR | |
| N1 | REGULAR SNF RATE – MC ENROLLEE | |
| N2 | SNF AIDS – MC ENROLLEE | |
| N3 | SNF NEURO–BEHAVIORAL – MC ENROLLEE | |
| N4 | SNF TRAUMATIC BRAIN INJURY | |
| N5 | SNF VENTILATOR DEPENDENT – MC ENROLLEE | |
| N6 | MLTC ENROLLEE PLACED IN SNF | |
| N7 | NH BUDGET APPROVED | |
| N8 | TRANSFER PENALTY PERIOD DHPCO | |
| N9 | NH RESIDENT PENDING NH ELIGIBILITY DETERMINATION |
File Layout Example: End Date a CF or CO
For enrollees that are determined as no longer eligible for CFCO, MCOs are responsible for reviewing the enrollee´s eligibility file and end dating any existing CF/CO RRE codes. The following layout must be used:
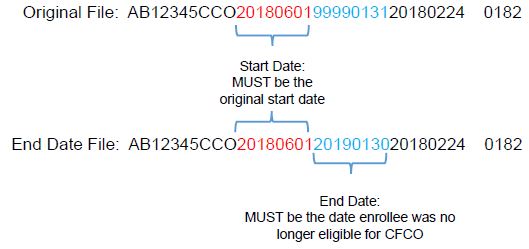
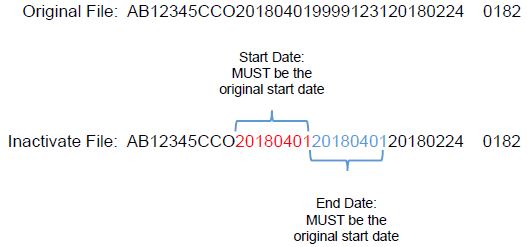
File Layout Example: Inactivate a CF or CO
When a CF or CO code was placed on a enrollee´s eligibility file and needs to be removed, the following layout must be used:
Activity Steps: RR/E Placement – CF CO RRE Code
|top of section| |top of page|Activity Steps: RR/E Placement – CF CO RRE Code
RR/E Placement – CF CO RRE Code
- Determine appropriate ´CF´ or ´CO´ RR/E code for placement on enrollee´s eligibility file.
- If enrollee is enrolled in MLTC, FIDA IDD, mainstream MMC, HIV SNP, or HARP and has RR/E 95, then ´CO´ must be placed on enrollee´s eligibility file. Proceed to step 2.
- If enrollee is enrolled in mainstream MMC, HIV SNP or HARP and does not have a 95 on file, then ´CF´ must be placed on enrollee´s eligibility file.
- If enrollee is enrolled in MLTC (excluding MLTC FIDA IDD), then ´CF´ must be placed on enrollee´s eligibility file. Proceed to step 2.
- Determine if a ´CF´ or ´CO´ code already exists and is active during the applicable time frame.
- If the enrollee has the incorrect ´CF´ or ´CO´ code, the code must be end dated or inactivated prior to the placement of the CFCO code identified in step 1.
- If the enrollee has the correct ´CF´ or ´CO´ code already on the eligibility file, no further action is needed.
- If the enrollee does not have the correct ´CF´ or ´CO´ code, then proceed to submit the CFCO RR/E code through the NYMC batch file process.
Contact Information
Questions/Comments: Email CFCO@health.ny.gov
More information can be found here.
|top of section| |top of page|
Follow Us