State Discussion with Children's Waiver HCBS Providers
January 2024
- Document is also available in Portable Document Format (PDF)
Purpose
- For the Department of Health (DOH) to share updates, guidance, and policy changes, and obtain feedback from Home and Community Based Service (HCBS) providers.
- Provide an opportunity for HCBS providers to discuss barriers and be a part of the problem-solving discussion.
- Have an open dialogue to communicate issues and concerns.
Agenda
Respite Billing Reminders
Planned Respite group of 2 rates included in the recent Waiver Amendment are not yet approved by DOB. Providers are not yet able to submit claims for this new rate code and should continue to use the applicable existing Planned Respite group rate code until DOB approval is received and announced.
| Respite up to 6 hours | Respite 6-12 hours | Respite 12-24 hours |
|---|---|---|
Billed in 15-minute units. Billed when service is provided for less than 6 hours. |
Billed as a per diem. Billed when service is provided
|
Billed as a per diem. Billed when service is provided
|
HCBS Provider Case Reviews
It is a requirement of the Children's Waiver to conduct an annual case review and fiscal audit. A number providers will be participating in case reviews this Winter; the remaining providers will participate in case reviews later this year. Those participating this Winter have already been notified and started submitting documents.
Several challenges were observed during the first review (Waiver Year 2021-22):
- Due to the findings, all HCBS providers received a corrective action plan (CAP).
- Many providers had their CAPs returned to them due to not meeting Waiver requirements.
- The processes, systems, policies, and/or documentation for many providers were not aligned with the Children's Waiver.
- There were concerns with some providers' amount of claiming and F/S/D.
- Providers with various lines of business (i.e., HCBS, CFTSS, care management, etc.) experienced challenges with having distinct policies and procedures specific to each line of business.
Process:
- A group of providers received approval of their CAP and CAP remediation plans should be implemented
- A group of providers received approval of their CAP with recommendations and their CAP items should be implemented.
- Other remaining providers received their CAP with recommendations in fall of 2023; this group of providers will be participating in case reviews beginning January 2024.
- These providers are in the process of submitting documents for the case review
Next Steps:
- Winter HCBS provider reviews will be completed
- HH/CYES will be review starting April 2024
- Providers not involved in the Winter 2024 review will be reviewed in the Summer and Fall of 2024.
- Prior to the review, these providers will receive a spreadsheet of their CAP items to report back how their remediation plans were implemented
REMINDER: Providers participating in the Winter Case Review should send any questions related to the review via HCS SFT to KidsHCBSCaseReview@health.ny.gov
Reminder of F/S/D Determinations
Frequency/Scope/Duration (F/S/D) must be clearly defined for each HCBS provided and based upon:
- The member's need(s) in relation to their Target Population and risk of institutionalization
- The member's availability and access to other services
- The goal to be accomplished
- How the service provided will accomplish the goal and meet the need (objectives/interventions)
- Choice and participation of the member
- Medical Necessity
- F/S/D should be developed in partnership with the member's family, care manager, and other involved professionals and must be supported by the need, goal, service requirements, and medical necessity.
- After accepting a referral, HCBS providers must complete an assessment with the member/family that will help determine the HCBS and F/S/D that will be requested for authorization.
- F/S/D is determined for each HCBS and must be provided as is outlined in the POC and HCBS Service Plan. HCBS providers should be updating HCBS Service Plans with the F/S/D approved by the MMCP.
- If there is a continuation of not meeting F/S/D, then this should be discussed with the participant and family/caregiver and adjusted, if appropriate.
- Communication with the MMCP regarding the adjustment should occur and update authorization may be need
- Care managers should be monitoring F/S/D and collaborating with HCBS providers.
- No changes to the members services or service providers should occur without the Care Manager involvement
HCBS Provider Designation and How Services are Provided
HCBS Providers Serving Their Own CMA or within One HH
HH/CMAs must ensure participant freedom of choice in their provider when making referrals for HCBS. Conflict-free case management safeguards are in place when a CMA and HCBS provider are affiliated with the same organization.
| Conflict-Free Case Management | Children's Waiver Participant: Rights & Responsibilities | |
|---|---|---|
| Health Homes (HH) and Home and Community Based Services (HCBS) providers must adhere to the requirements for Conflict-Free Case Management (CFCM) for Health Home Serving Children (HHSC) members and the process for which CFCM should be implemented. If a member receives more than one HCBS, they may work with the same or different agency(s) to provide these services. Members must be made aware that the HHCM/HCBS providers must work in the member's best interest, ensure no conflict of interest, and continue to give of services and service providers. Any type of agreement involving sending referrals to a HH/CMA in exchange for an HCBS referral back is in conflict with the conflict-free requirements. | A member has the choice between HCBS or an institution such as a hospital, residential facility, or a nursing home. If a member chooses HCBS, they have a choice of Health Home/Care Management Agencies AND HCBS providers in their area. The member must be provided several HCBS provider options to choose from (i.e., the care manager cannot only provide HCBS provider options with whom the HH/CMA is affiliated with). A member may receive services and care management from different agencies or the same agency, based on their choice. The member must have choice. |
HCBS Provider Designation
HCBS providers are designated by county and services
- Designation was determined based upon the provider demonstrating the ability to serve the population within the county
- Waiver enrolled members need to have choice of HCBS providers and services they need and are medically necessary
- HCBS providers cannot limit providing services based upon the affiliation of the care management agency
HHCMs and C-YES are the only entities that can make referrals to HCBS providers
HCBS providers cannot move a member to another HCBS provider
Billing Updates & Discussion: Requirements
| Submitting Electronic Claims When submitting an electronic claim for Children's HCBS and CFTSS with dates of service on or after December 1, 2023, providers must enter Value Code 85 plus the applicable FIPS code. Providers must continue to include any other value code that is necessary to accurately report the claim (e.g., rate code) in this box. |
Submitting Paper Claims When submitting paper claims for dates of service on or after December 1, 2023, providers must enter Value Code 61 plus the applicable proxy locator code in the Value Code box of the claim. Providers must continue to include any other value code that is necessary to accurately report the claim (e.g., rate code) in this box. |
Systems Updates Are systems updated appropriately to be able to bill in compliance with new billing requirements? Note: Please contact bh.transition@health.ny.gov if systems are not ready by February 1, 2024. |
| HCBS providers can only provide services to members within their designated counties and bill for such | Resources Billing Changes for HCBS and CFTSS Providers Effective December 1, 2023 (ny.gov) AND changes_faqs.pdf (ny.gov) |
What is the status of each provider's configuration? Is there a need for delay reason codes? |
Telehealth for HCBS
| HCBS providers should be providing services in- person with the member/family by choice of home or community setting. | Until further notice / guidance is provided by DOH, telehealth for HCBS is currently still allowed (aside from Respite), when appropriate. Providers must ensure that telehealth modifiers are used, and service modality is indicated in the case notes. |
The FIPS/County Locator code used on a telehealth claim should reflect the location of staff during service delivery. If the staff member is telecommuting-the location of the agency's office should be reflected on the claim. |
HCBS Referral Portal
CFASS Example
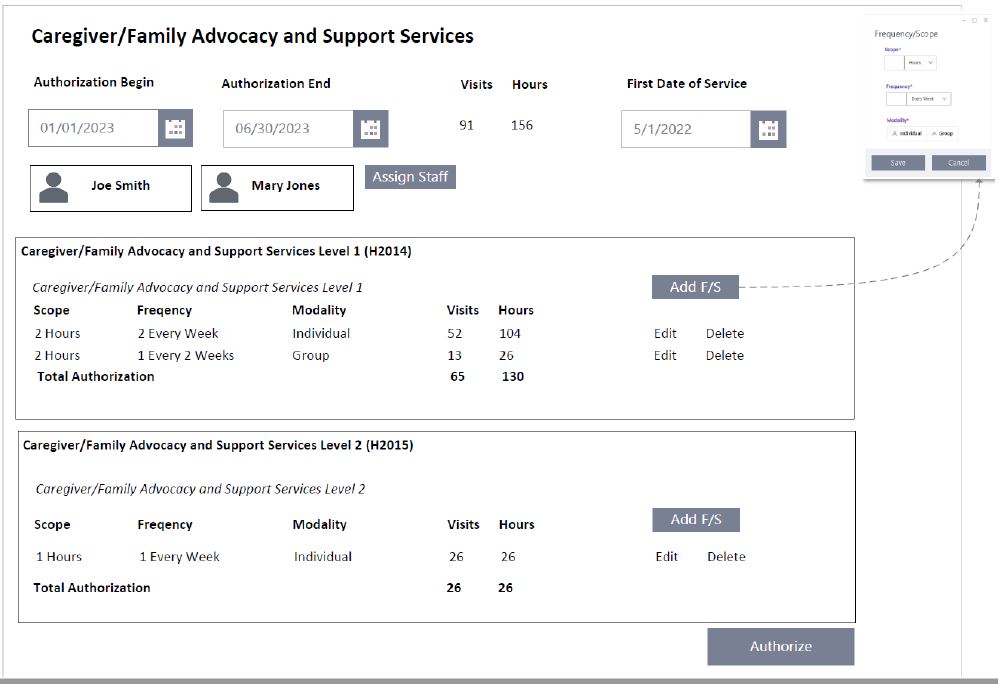
Question for Providers:
Would the addition of Units alongside hours and visits be helpful for visualizing a member's F/S/D?
*Data within these slides have been fabricated for the purpose of this webinar and do not reflect actual PHI
Planned Respite Example
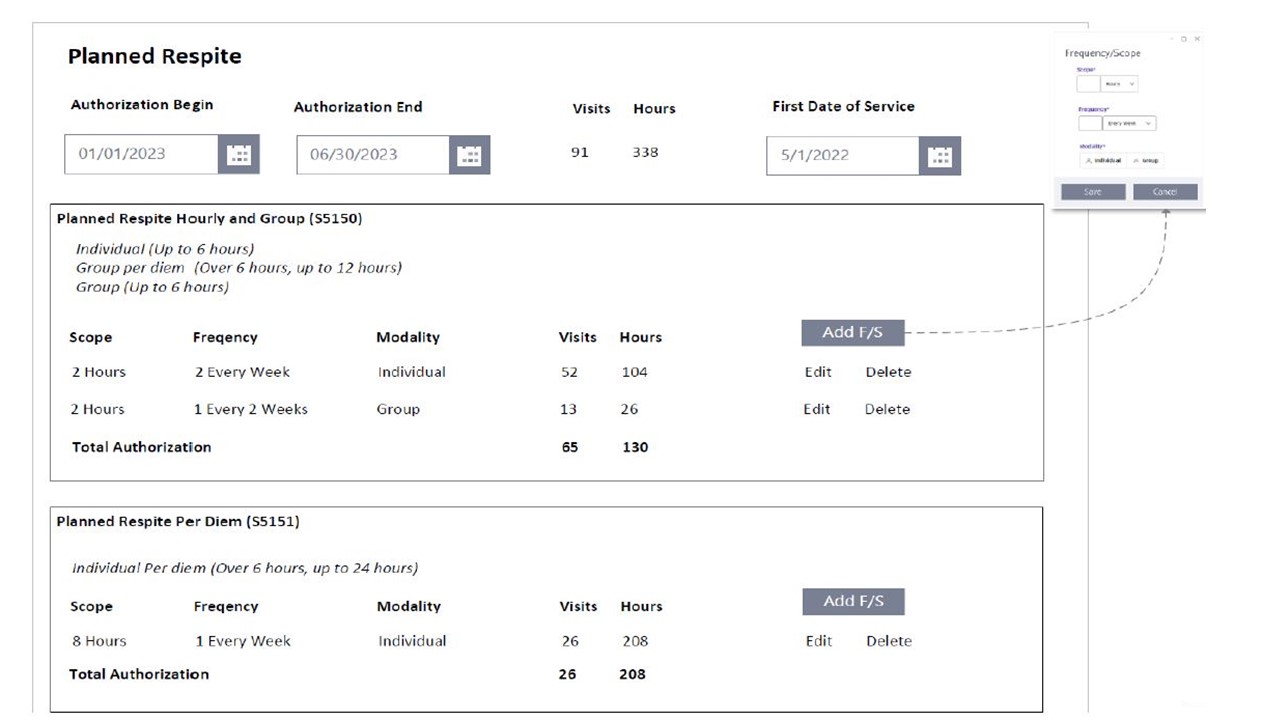
These new forms should capture feedback/info from stakeholders to help finalize the Referral Portal, which is slated to launch in Spring 2024
*Data within these slides have been fabricated for the purpose of this webinar and do not reflect actual PHI
Please submit feedback (by January 26, 2024) about the proposal to include service units on authorization here: BH.Transition@health.ny.gov.
Future Meetings & Contact Information
Future Meetings & Agenda Items
- Next Scheduled Monthly Meetings:
- February 21st 1:00 - 2:30 PM
- March 20th, 2024, from 1:00 PM - 2:30 PM
- April 17th, 2024, from 1:00 PM - 2:30 PM
- DOH would like to discuss topics of interest to the HCBS providers and also hear suggestions and ideas for improvement.
- Please submit your agenda requests, suggestions, or questions to BH.Transition@health.ny.gov.
All Children's Waiver HCBS questions and concerns, should be directed to the NYS Department of Health at BH.Transition@health.ny.govmailbox or (518) 473-5569.
Questions regarding the HCBS Settings Final Rule can be directed to ChildrensWaiverHCBSFinalRule@health.ny.gov.
New York State Department of Health Managed Care Complaint Line 1-800-206-8125 or managedcarecomplaint@health.ny.gov.
Follow Us