Waiver Public Forum
- Document is also available in Portable Document Format (PDF)
1115 Medicaid Redesign Team (MRT) Waiver Public Forum
October 30, 2019
1115 MRT Waiver Overview
1115 Demonstration Waiver
- Also known as Section 1115 of the Social Security Act, which gives the Secretary of Health and Human Services the authority to waive certain provisions and regulations, and also to allow Medicaid funds to be used in ways that are not otherwise allowed under federal rules.
- 1115 Demonstration Waivers grant flexibility to states for innovative projects that advance the objectives of Title XIX of the Medicaid program, and thus waive certain compliance requirements of federal Medicaid laws.
- A Waiver can be approved for up to five years and the State may request subsequent extensions.
General 1115 Demonstration Waiver Overview
- Special Terms and Conditions (STCs) outline the basis of an agreement between the State and the Centers for Medicare and Medicaid Services (CMS) including waiver and expenditure authorities. STCs specify the State´s obligation to CMS during the life of the demonstration, including general and financial reporting requirements and a timetable of State deliverables.
- Quarterly and annual reports are required, and an Independent Evaluation is completed at the end of a Demonstration program.
- Federal Medicaid expenditures with the Waiver cannot be more than federal expenditure without the Waiver during the course of the Demonstration.
- Also known as Budget Neutrality or Budget Neutral.
New York State´s 1115 Waiver
- TheNYS Medicaid Redesign Team (MRT) Waiver (formerly the Partnership Plan) has been in operation since 1997.
- New York´s 1115 MRT Waiver was renewed on December 6, 2016 and is effective through March 31, 2021.
- Key Goals for the Waiver are to:
- Improve access to health care for the Medicaid population;
- Improve the quality of health services delivered; and
- Expand coverage with resources generated through managed care efficiencies to additional low–income New Yorkers.
1115 MRT Waiver Programs
Medicaid Managed Care: Comprehensive health care services (including all benefits available through the Medicaid State Plan) to low–income, uninsured individuals.
An opportunity for enrollees to select a Managed Care Organization (MCO) with a focus on preventive health care.
- Programs include:
- Mainstream Medicaid Managed Care (MMMC)
- Health and Recovery Plans (HARPs) and Home and Community Based Services (HCBS)
- Managed Long Term Care (MLTC) and Long Term Services and Supports (LTSS)
Delivery System Reform Incentive Payment (DSRIP) program: Provides incentives for Medicaid providers to create and sustain an integrated, high performance health care delivery system.
Designed to effectively meet the needs of Medicaid beneficiaries and low–income uninsured individuals in their local communities and thereby improving quality of care, improving health outcomes & reducing costs (referred to as the CMS Triple Aim).
DSRIP Waiver ends March 31, 2020.
1115 MRT Waiver Pending Amendments
- Managed Long Term Care Partial Capitation Plans– Subject to CMS Approval
Nursing Home Benefit- DOH is continuing to work with CMS to modify the partial capitation long term plan benefit (MLTCPC) package to include only 3 calendar months of permanent nursing home care for individuals who are permanently placed.
- Plan Changes
- Consistent with mainstream managed care, amendment would allow a member to switch from one MLTC plan to another MLTC within a 90–day grace period following enrollment, but not permit MLTC plan switches for the remaining 9 months of the year unless a good cause exception is granted.
- Continuity of Coverage for Justice–involved Populations– Subject to CMS Approval
- Amendment outlines the provision of targeted services to eligible Medicaid–enrolled incarcerated individuals with two or more chronic physical/behavioral health conditions, a serious mental illness, or HIV/AIDS, or opioid use disorder.
- Objective of the demonstration is to provide in–reach transitional services 30 days prior to release, in order to ensure high–risk justice–involved populations receive needed care management, physical and behavioral health services, medication management and medication, and critical social supports upon release into the community.
- By introducing and linking individuals with serious physical and behavioral health conditions to a comprehensive system of care and transitional supports pre and post discharge, there is a higher likelihood of connectivity to care at release, leading to more stability once established in the community including improved health, lower recidivism, and lower costs.
- Coverage for these services is requested for individuals incarcerated in county and State facilities.
Work in Progress…
- DSRIP beyond March 2020
- 1115 MRT Waiver Renewal
- MRT Waiver authority expires March 31, 2021
- Submit renewal application to CMS by September 30, 2020
- Supportive Housing – under discussion with CMS
- Achieve federal financial participation in supportive housing services
DSRIP DRAFT WAIVER AMENDMEMNT PROPOSAL
DSRIP Demonstration Progress to Date
Additional Progress Information
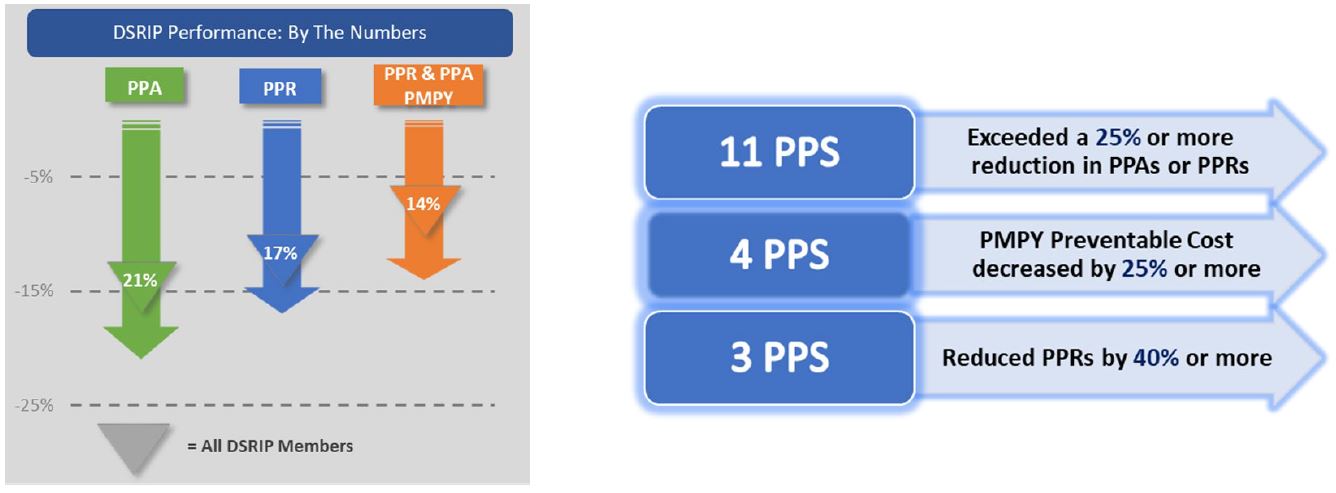
The DSRIP population grew by 8% from 4.453 to 4.809 million
- This is an additional 356,780 Medicaid members from 2014 through 2018 for engaging in care and measuring performance impact.
- Potentially Preventable Readmissions rate still decreased by 17%.
- 3,000 fewer people had PPR events in MY4 even with sizeable population growth.
- Number of people with asthma increased by 7,500 in 4 years. The rate of long term medication adherence still improved by 11% during this period.
- Follow–up after hospitalization for mental illness within 30 days improved by over 12% in three years.
- An additional 2,500 people in MY3 alone received more timely care.
DSRIP and VBP Performance Highlights
PPS Performance
- The 25 PPS have implemented 259 DSRIP projects across the state.
- System Transformation projects – 113
- PCMH Transformation – 2400 new recognized practices supported by PPS
- Behavioral Health and Substance Use treatment projects – 43
- Clinical Improvement for targeted chronic diseases and other areas – 55
- Prevention Agenda projects – 48
- System Transformation projects – 113
- Approximately 3.5 Million patient engagements in DY 4 – April 2018–March 2019
- PPS have earned $5.5 B (85%) of all available funds through DY4 (March 2019)
Value–based Payment Roadmap
- NYS has exceeded the DY4 goal with 65% of Medicaid managed care contracts at Level 1 and higher and 35% of those contracts at Level 2.
Continuing the Transformation
DSRIP Amendment Request
- New York seeks a four (4)–year waiver renewal to further support the cost savings and quality improvements by aligning with federal goals and through the DSRIP Promising Practices. New York is requesting $8 billion over this period to be invested as follows:
- $5 billion DSRIP performance;
- $1 billion workforce development;
- $1.5 billion social determinants of health (SDH); and
- $500 million Interim Access Assurance Fund (IAAF).
- More time is needed to sustain and scale the DSRIP promising practices with managed care organizations (MCOs) as part of value–based payment (VBP) arrangements, while driving more careful alignment with current federal healthcare initiatives.
DSRIP Promising Practices
United Hospital Fund – DSRIP Promising Practices for Meaningful Change for New York Medicaid
- Expansion of medication–assisted treatment into primary care and emergency department (ED) settings;
- Partnerships with the justice system and other cross–sector collaborations;
- Primary care and behavioral health integration;
- Care coordination, care management, and care transitions;
- Expansion of Mobile Crisis Teams (MCT) and crisis respite services;
- Focus on patients transitioning from institutions for mental diseases (IMDs) to the community;
- Focus on seriously mentally ill/seriously emotionally disturbed populations;
- Addressing social determinants of health through community partnerships; and
- Transforming primary care and supporting alternative payment models.
Value–Driving Entities (VDEs)
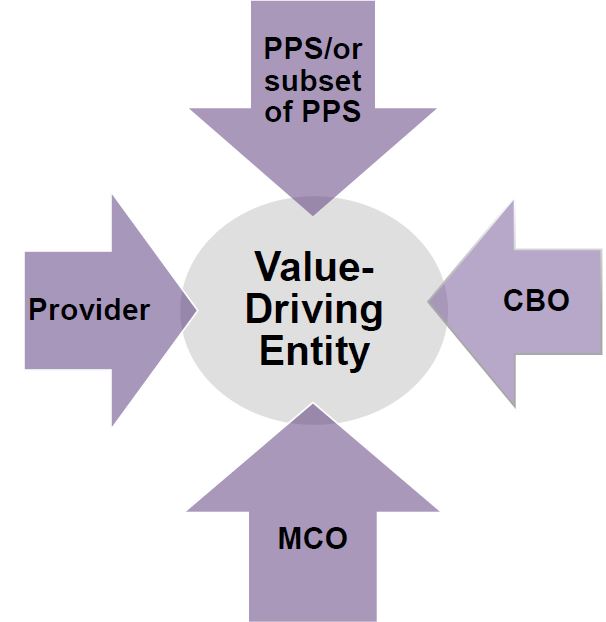
- Performing Provider Systems (PPS) or a subset of PPS, provider, community–based organization (CBO) and MCO teams specifically approved by the state to replicate and scale the high–priority DSRIP promising practices
- VDEs will be required to have MCOs as active partners in the delivery system collaboration for the development of more sophisticated VBP models to support the maturing networks;
- VDEs will continue to be assigned specific regions/markets and attributed populations;
Expand Practices to Additional High–Need Areas and Populations
Reducing Maternal Mortality – 50 percent of the state´s births are covered by Medicaid
- In April 2018, Governor Andrew M. Cuomo announced a comprehensive initiative to target maternal mortality and reduce racial disparities in health outcomes.
Children´s Population Health – 47 percent of the state´s children are covered by Medicaid
- Promising practices would extend to chronic care management, behavioral health integration, pediatric–focused patient–centered medical homes, and attention to adverse childhood experiences and social determinants.
Long–Term Care Reform
- Address the needs of the rapidly growing senior population and the long term care sector and workforce that will be needed to support future needs.
Continued Improvements/Investments
Workforce Flexibility and Investment
- DSRIP promising practices have relied on non–traditional, non–clinical workforce to achieve project goals and ongoing flexibility for VDEs to invest earned dollars to support this workforce as MCOs and CBOs design VBP approaches to sustain these models in the long term.
Addressing the Opioid Epidemic
- Build on best practices of broad screening for Substance Use Disorder/Opioid Use Disorders (OUD/SUD) in primary care and medication–assisted treatment initiated in EDs and primary care settings. Further focus on the justice–involved population, hospital to community linkages, and deployment of peers in care transitions, navigation, and recovery.
Interim Access Insurance Fund
- IAAF 2.0 will be structured to ensure sufficient numbers and types of providers to Medicaid and uninsured individuals while the state continues its transformation path of driving down avoidable hospitalizations.
Coordinated Population Health Improvement
A Multi–Payer Context for Reform
- Value–Driving Entities to integrate Prevention Agenda goals and considera multi–payer lens when implementing the promising practices to promote 360–degree population health and to further the sustainability of these reform approaches.
Social Determinant of Health (SDH) Networks
- Continuing New York´s pioneering investments, Social Determinant of Health (SDH) Networks will be formed to deliver socially focused interventions linked to VBP.
Performance Measures and Payments to Facilitate Future Value–Based Payment Models
- Align with the Centers for Medicare and Medicaid Services (CMS) Meaningful Measures Framework, CMS core measure sets, and other federal and state measures already in use.
Recap and Timeline
- In order to sustain this success and move transformation forward to a higher level, New York seeks to continue its partnership with the federal government through an amendment to the DSRIP waiver.
- Expanding DSRIP promising practices will further drive up quality while lowering cost to the state and our federal partners.
- Draft DSRIP Waiver Amendment Proposal.
- Public comment period open until November 4, 2019 – written comments to be sent to: 1115waivers@health.ny.gov
- Downstate MRT Public Comment – October 25, 2019 – NYC
- Upstate MRT Public Comment – October 30, 2019 – Syracuse
- Application to CMS due November 27, 2019 for notification before March 31, 2020 expiration
1115 MRT Waiver Resources
1115 MRT Waiver Website
http://www.health.ny.gov/health_care/medicaid/redesign/medicaid_waiver_1115.htm
Managed Care
https://www.health.ny.gov/health_care/managed_care/index.htm
DSRIP
http://www.health.ny.gov/health_care/medicaid/redesign/dsrip/
08/02/2019 STCs DOH website
https://www.health.ny.gov/health_care/managed_care/appextensi on/docs/2019–08–02_ny1115_stc.pdf
Quality Strategy
CMS Homepage
Medicaid Homepage
Guidelines for Public Comments
- If you´d like to speak, please sign up at the registration table.
- When your number is called, please come up to the microphone.
- Comments will be timed. You will have 5 minutes to speak.
- Please return your number to one of the timekeepers.
Written comments can be submitted at the registration table.
You may also submit written comments by November 4, 2019 to:
1115waivers@health.ny.gov
Subject: MRT Public Comment
Follow Us