Meeting 1

- Meeting Presentation also available in Portable Document Format (PDF)
August 7, 2017
Welcome
Nancy Zimpher, Chair, First 1000 Days on Medicaid
Kate Breslin, Vice Chair, First 1000 Days on Medicaid
|top of section|
|top of page|
Meeting Agenda
| Item # | Agenda Items | Time | Duration |
|---|---|---|---|
| 1. | Welcome and Introductions | 11:00am | 15 mins |
| 2. | Problem Definition, Committee Charge, and Process | 11:15am | 75 mins |
| 3. | Lunch | 12:30pm | 45 mins |
| 4. | Idea Generation | 1:15pm | 90 mins |
| 5. | Next Steps and Adjourn | 2:45pm | 15 mins |
Participants joining by audio only: please email ggroenke@uhfnyc.org with your name and organization so we may record your attendance
Big Picture: Why We´re Here
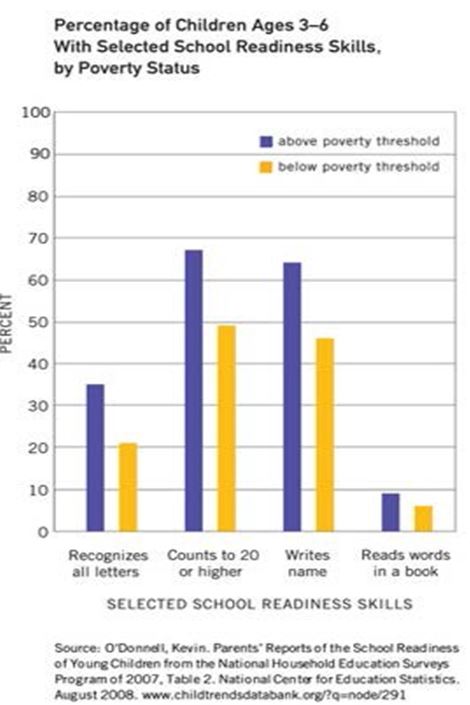
Point 1: A child´s brain develops rapidly in the first 3 years of life, and we now know what kinds of interventions can help or hinder this process.
Point 2: Early experiences´ effect on the brain and body partially explain significant disparities in health and learning by school entry – especially for children living in poverty.
Our Leaking Education Pipeline
- 40% of children enter kindergarten not ready*
- 42% of 3rd Graders are Proficient in Reading
- 24% of 8th Graders are Proficient in Math*
- 80% of High Schoolers Graduate in 4 Years
- 65% of graduates enroll in post–secondary
- 50.5% of SUNY 4–year students complete in 4 years; 67% complete in 6yrs
Every Child, Cradle to Career
Point 3: These early experiences have serious, long–term consequences for children in the education pipeline.
And it´s our collective responsibility to fix this.
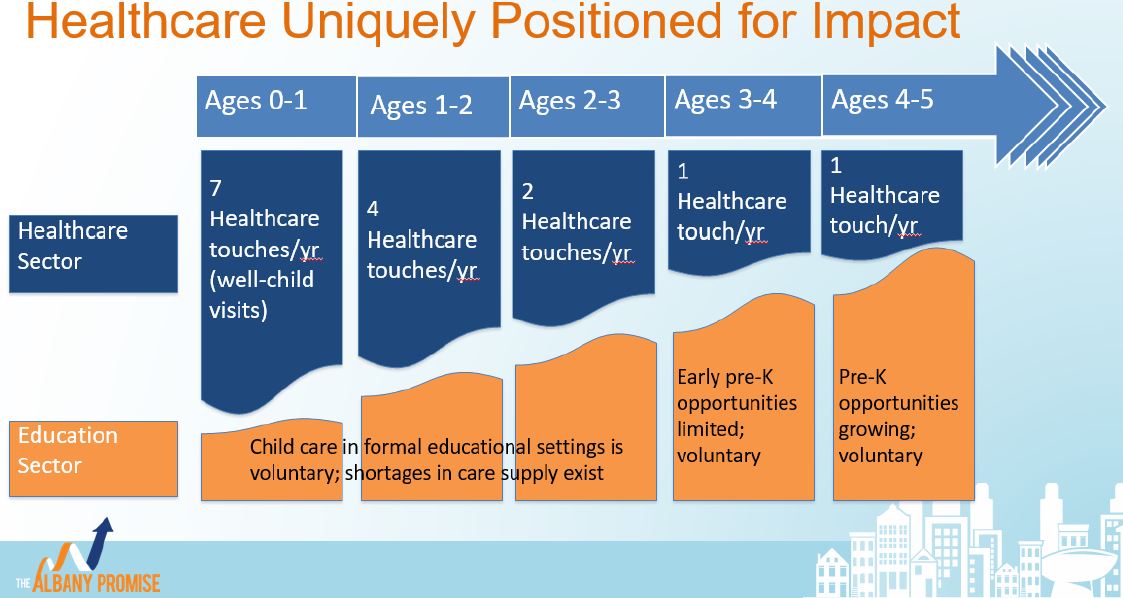
Point 4: Medicaid has a big role to play.
Source: http://www.albanypromise.org/
Work Group Leadership
Chair:
Nancy Zimpher, Chancellor,
The State University of New York
Vice Chairs:
Kate Breslin, President & CEO,
Schuyler Center for Analysis and Advocacy
Jeff Kaczorowski, MD, Senior Advisor,
The Children´s Agenda
Work Group Members
| Name | Organization |
|---|---|
| Jeanne Alicandro, MD | New York State Department of Health |
| Wilma Alvarado–Little | New York State Department of Health |
| Benjamin Anderson | Children´s Defense Fund New York |
| Lori Andrade | Health and Welfare Council of Long Island |
| Angela Angell | Staten Island Alliance for North Shore Children and Families |
| Anita Appel | Sachs Policy Group |
| George Askew, MD | New York City Department of Health and Mental Hygiene |
| Sonia Barbosa | Healthfirst |
| Amir Bassiri | Executive Chamber |
| Gary Belkin, MD | New York City Department of Health and Mental Hygiene |
| Susan Beane, MD | Healthfirst |
| Wendy Bender | New York State Association for Infant Mental Health |
| Evelyn Blanck | New York Center for Child Development |
| Donna Bradbury | New York State Office of Mental Health |
| Alexandra Brandes | Lenox Hill Neighborhood House |
| Carla Braveman | Hospice and Palliative Care Association of New York State |
| Kate Breslin (Vice–Chair) | Schuyler Center for Analysis & Advocacy |
| Rahil Briggs | Montefiore |
| LuAnne Brown | Buffalo Prenatal–Perinatal Network, Inc. |
| Monica Brown | Health Foundation of Western and Central New York |
| Suzanne Brundage | United Hospital Fund |
| John Burke | WellCare of New York, Inc. |
| Betsy Campisi | Allliance for Better Health |
| Dina Carreras | The Staten Island North Shore Alliance for Children and Families |
| Joanne Casarella | New York City Department of Health and Mental Hygiene |
| Nora Chaves | Healthfirst |
| Meredith Chimento | Early Care & Learning Council |
| Andrew F. Cleek | McSilver Institute for Poverty Policy and Research, NYU Silver School of Social Work |
| Lauri Cole | NYS Council for Community Behavioral Healthcare |
| David Collins | The Children´s Village |
| Mary Comtois | United Way |
| Pradine Content | The New York Foundling |
| J. Coppola | NY Association of Psychiatric Rehabilitation Services, Inc. |
| Shawna Craigmile–Sciacca | Upstate University Health System |
| Maria Cristalli | Hillside Family of Agencies |
| Barbara Crosier | Cerebral Palsy Associations of New York |
| Enrico Cullen | a.i.r. NYC |
| Amber Decker | Independent Provider of Peer Support Services |
| Lauren Deutsch | Healthy Baby Network |
| Ellyce di Paola | EmblemHealth |
| Sean Doolan | Hinman Straub |
| Lana Earle | New York State Department of Health |
| MaryEllen Elia | New York State Education Department |
| David Fagan, MD | Northwell Health |
| Lindsay Farrell | Open Door Family Medical Center |
| Lowell Feldman | The Castleton Group |
| Diane Ferran, MD | CHCANYS |
| Mildred Ferriter | Community Health Center of St. Marys and Littauer |
| Beth Finnerty | Cardinal McCloskey Community Services |
| Douglas Fish | New York State Department of Health |
| Maura D. Frank, MD | Weill Cornell Medical College |
| Taylor Frazier | Community Service Society of New York |
| David Goldstein | JCCA |
| Aimee Gomlak | Catholic Health System |
| Bob Graham | New York State Bleeding Disorders Coalition |
| Victoria Grimshaw | New York City Department of Health and Mental Hygiene |
| Michael Grossfeld | All About Kids |
| Lisa B. Handwerker, MD | The Children´s Aid Society |
| Steve Hanson | New York State Office of Alcoholism and Substance Abuse Services |
| Jennifer F. Havens, MD | NYU Langone / Bellevue |
| Ariel Hayes | Northwell Health |
| Christian Heiss | Nurse–Family Partnership |
| Jason Helgerson | New York State Department of Health |
| Zachariah Hennessey | Public Health Solutions |
| Dirk Hightower | Children´s Institute |
| Emily Horn | Alliance for Better Health |
| Sajidah Husain, MD | Empire BlueCross BlueShield, Healthplus |
| Liz Isakson, MD, FAAP | Docs for Tots |
| Viju Jacob, MD, FAAP | Urban Health Plan, Inc. |
| Sophia Jan, MD | Northwell Health |
| Marilyn Kacica | New York State Department of Health |
| Jeffrey Kaczorowski, MD (Vice–Chair) | Children´s Agenda; University of Rochester Medical Center |
| Karen Kalaijian | Nurse Family Partnership |
| John Kastan | The Jewish Board of Family and Children´s Services |
| Paul Kaye, MD | Hudson River Healthcare |
| Eunhye Grace Kim | The Korean Community Service of Metropolitan New York, Inc. |
| Dennis Z. Kuo, MD, MHS | University at Buffalo |
| Audrey LaFrenier | Northern Rivers Family of Services |
| Jason Lippman | The Coalition for Behavioral Health, Inc. |
| Jaime Madden | NYC Administration for Children´s Services |
| Kallanna Manjanuth, MD | Albany Medical Center, Better Health for Northeast New York PPS |
| Jennifer March | Citizens´ Committee for Children of New York |
| Daniel Maughan | St. Luke´s Cornwall Hospital |
| Alexandra Maul | Center for Health Care Strategies |
| Mary McCord, MD | Gouverneur Health Services (Gotham) / NYU |
| Bernadette McDaniel | Ellis Medicine |
| Philip McDowell | Independent Psychotherapist |
| Matthew McLarnon | Capital Health Consulting |
| Adrienne Mercer | Northern Manhattan Perinatal Partnership |
| Heather Mermel | Beacon Health |
| Dodi Meyer, MD | Columbia University Medical Center / New York Presbyterian Morgan Stanley Children´s Hospital |
| Margaret Mikol | SKIP of NY |
| Acklema Mohammad, MD | Urban Health Plan, Inc. |
| Ann Monroe | Former Health Foundation for Western and Central New York |
| Kristen Mucitelli–Heath | St. Joseph´s Health |
| Sandra Murawski | Amerigroup Partnership Plan |
| Kerri Neifield | Office of Governor Andrew M. Cuomo |
| Karen Norman | ANDRUS |
| Chris Norwood | Health People |
| Ciearra Norwood | NYS Council on Children and Families |
| David Oakley | Manatt, Phelps & Phillips, LLP |
| Briannon O´Connor | Center for Collaboration in Community Health |
| Alex Okun, MD | New Alternatives for Children |
| Alda Osinaga | NYSDOH OHIP |
| Christy Parque | The Coalition for Behavioral Health |
| Matthew Perkins, MD | Children´s Services |
| Frank Pindiak | St. Catherine´s Center for Children |
| Lauren Pollow | NYS Health Facilities Associations |
| Suniti Ponkshe | Optum |
| Sheila Poole | NYS Office of Children and Family Services |
| Kira Pospesel | Greene County DSS |
| Juliette Price | The Albany Promise |
| Joyce Riemer | Independent Consultant |
| Reneee Rider | New York State Education Department |
| David Rock | Grant Thornton |
| Marci Rosa | Public Health Solutions |
| Harvey Rosenthal | NY Association of Psychiatric |
| Sylvia Rowlands | The New York Foundling |
| Joseph R. Saccoccio, MD | The New York Foundling |
| Rebecca Sanin | Health and Welfare Council of Long Island |
| Wendy Saunders | Hinman Straub |
| Christine Schuyler | Chautauqua County Department of Health & Human Services |
| Kalin Scott | New York State Department of Health |
| Chad Shearer | United Hospital Fund |
| Peter Sherman, MD, MPH | Bronx Lebanon Hospital |
| Phyllis Silver | Partnership for Quality Care |
| Edwin Simper, MD | St. Mary´s Health Systems for Children |
| Brendon Smith | Better Health for Northeast New York |
| Sheila Smith | Columbia Universtity – National Center for Children |
| Richard Soden, OD | SUNY College of Optometry |
| Stephen Somers | Center for Health Care Strategies |
| Tonia Spence | The Jewish Board of Family and Children´s Services |
| Joseph A. Stankaitis, MD | YourCare Health Plan |
| Danny Stephens, MD | The Children´s Aid Society |
| Marjorie Stuckle | Empire BlueCross BlueShield, Healthplus |
| Lauren Tobias | New York State Department of Health |
| John Torres | Liberty Resources |
| Christopher Treiber | INTERAGENCY COUNCIL of Developmental Disability Agencies, Inc. |
| Alia Udhiri | New York City Department of Health and Mental Hygiene |
| Omolara Thomas Uwemedimo, MD, MPH | Northwell Cohen Children´s Medical Center |
| Jane Vail | Central New York Health Home Network |
| Abigail Velikov | New York City Department of Health and Mental Hygiene |
| Susan Vierczhalek, MD | NYU Langone Health |
| Norma Villanueva, MD, MPH | Family Health Center at NYU Langone |
| Bridget Walsh | Schuyler Center for Analysis & Advocacy |
| Elie Ward | American Academy of Pediatrics District II, NYS |
| Nicholas Weatherbee | Assembly Majority Leader Joe Morelle |
| Kristin Weller | NYS Council on Children and Families |
| Judy Wessler | Coalition to Protect Medicaid |
| Kara Williams | The Allyn Foundation |
| Carrie Edwards Wolkoff | Sparks Therapeutics |
| David Woodlock | ICL |
| Nancy Yassa | Anthem |
| Shawn Yetter | Tioga County DSS |
| Fern Zagor | Staten Island Mental Health Society |
| Nancy Zimpher, Ph.D (Chair) | The State University of New York |
Defining the Problem, Work Group Charge, and Decision–Making Framework
Jason Helgerson, Deputy Commissioner and Medicaid Director, NYSDOH
Kate Breslin, President and CEO, Schuyler Center for Analysis and Advocacy
What´s the problem?
Pregnant women depend on Medicaid:
51% of all births are covered by Medicaid.
Kids depend on Medicaid:
48% of New York´s children 0–18 are covered by Medicaid.
Children in their first 1000 days of life depend on Medicaid:
59% of kids 0–3 in New York are covered by Medicaid.
Sources:
1. http://www.kff.org/medicaid/state–indicator/births–financed–by–medicaid/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22a sc%22%7D
2. U.S. Census Bureau, Population Division. Medicaid enrollment count as of December 2015.
Young Children on Medicaid...
- Do not have high expenditures
- Children ages 0–4 averaged only $3,837 in annual expenditures in 2014
- Children ages 18–20 averaged $5,312
- Use the emergency department more frequently than older kids
- 36% of children ages 0–4 had at least one ED visit in 2014
- No other age group is higher than 26%
- Use primary care frequently
- 88% of children under age 1 had at least one outpatient evaluation and management or preventive care claim in 2014 (average 8.95 claims/child)
- 93% of children ages 1–4 had at least one of these claims (averaged 6.03 claims/child)
Source: United Hospital Fund, Understanding Medicaid Utilization for Children in New York: A Chartbook. http://uhfnyc.org/assets/1516
Medicaid serves children at highest risk for poor health outcomes
U.S. Children´s Health Outcomes and Risk, by Income Gradient, 2011 – 2012

Source: Data from Halfon N, PH Wise, and CB Forrest. 2014. The changing nature of children´s health development: new challenges require major policy solutions. Health Affairs 33(12): 2116–2124.
And at high–risk for poor lifetime outcomes
The first 1,000 days of a child´s life are a critical window for development. Exposure to adverse childhood experiences dramatically increases the potential for life–long negative health and social outcomes.
Adverse Childhood Experiences
- Abuse
- Neglect
- Family Dysfunction
- Exposure to Violence
Can Lead to....
- Poor School Performance
- Developmental Delays
- Juvenile Justice Involvement
- Poor Health in Adulthood
Source: "The First 1,000 Days: Medicaid´s Critical Role." Center for Health Care Strategies, June 2017.
Available at: https://www.chcs.org/resource/first–1000–days–medicaids–critical–role/.
Medicaid Already Helps Children Have Better Outcomes
- Increases the rates of high school and college graduation
- Medicaid results in better health and lifetime outcomes for children
- The most important time for coverage is during pregnancy, infancy and early years
- We get the highest return for investments in improving SDH and human development
- Medicaid coverage also improves educational outcomes, employment, and reduces welfare dependency
- Medicaid gives kids a better chance to maximize lifetime outcomes
Medicaid Already Helps Children Have Better Outcomes
| Performance Measure | New York Medicaid Statewide Average |
National Median | New York Ranking |
|---|---|---|---|
| Well child visits first in the first 15 months of life | 68.5 | 62.1 | 2nd Quartile of reporting states |
| Access to Primary Care 12–24 months | 96.9 | 96.4 | 2nd Quartile of reporting states |
| Childhood Immunization Status at age 2 | 73.2 | 66.9 | 2nd Quartile of reporting states |
Source: United Hospital Fund, Understanding Medicaid Utilization for Children in New York: A Chartbook. http://uhfnyc.org/assets/1516
- We won´t be able to help kids without a focus on the social determinants of health (SDH)
- These include poverty, unequal access to health care, poor environmental conditions, educational inequities.
- SDH disproportionately affect poor and minority children.
- We must work cross–system to address these issues.
What´s the charge to this group?
- ☒ The "First 1000 Days on Medicaid" initiative will be a collaborative effort, bringing together stakeholders to develop recommendations for a ten–point plan.
- ☒ Builds off of the successful VBP Advisory Group on Children´s Health.
- ☒ The group´s ten–point plan will focus on improving outcomes and access to services for children in their first 1000 days: the most crucial years of their development.
Focusing the Charge
- ☒ Goal is broad population level improvement in child health and development "Moving upstream to prevent future super–utilizers"
- ☒ Initial phase recommendations focused on the large majority of children ages 0–3 not already receiving specialized services (e.g., OPWDD, children with medically complex conditions)
Ten–point plan should be:
- ☒ Specific and laser focused on improving outcomes and access to services for children in their first 1000 days
- ☒ Focused on what is doable in the near–term Affordable
- ☒ Implementable through Medicaid levers
The group will work for a little over two months with a completion date slated for early November.
How do we get started?
| Long–term Goal | Desired Outcomes for Children Ages 0–3 Source: NYS Children´s VBP Subcommittee and Clinical Advisory Group |
Primary Drivers for Brain Development and Lifelong Health Source: Harvard Center on the Developing Child (2010). The Foundations of Lifelong Health |
||
|---|---|---|---|---|
| All children in New York are well and thriving | ||||
| ← | Optimal birth outcomes for mother and child | |||
| ← | Secure caregiver–child attachment established by age 1 | ← | Stable, responsive, and nurturing caregiving early in life lays the groundwork for the development of a wide range of basic biological processes that support emotion regulation, sleep–wake patterns, attention, and ultimately all psychosocial functioning. Access to comprehensive, patient–centered medical care for pregnant women and children can help prevent threats to healthy development as well as ensure correction and/or management of health problems. Sound and appropriate nutrition is essential at every stage of the life course, beginning with the mother´s pre–conception nutritional status, extending through pregnancy to early infant feeding and weaning, and continuing with diet and activity throughout childhood. Safe environments, free from toxic chemicals and toxic stress, are necessary for protecting children´s immediate physical well–being as well as their future health and development. |
|
| ← | Optimal physical health and developmental trajectory (motor, language, cognitive, and social–emotional) by age 3. | |||
Healthy and Ready Children and Families
pK–12 Education Levers
- Provider of pre–kindergarten services (3– and 4–year–old seats)
- Compulsory education beginning at age 5
- Student achievement data
- Regulatory and State-level policy
Higher Education Levers
- Largest provider of post–secondary opportunity
- Reconnection efforts (EOC, non–credit/degree programs)
- Workforce development & credentialing
- State–level policy
Social Service Provider Levers
- Largest provider of family support services
- Family income support
- Connection to child & family services
- State–level policy
Medicaid Levers
- Medicaid payment and incentives
- Quality improvement infrastructure
- Medicaid managed care contracts
- Non–federal regulatory changes
- Enabling innovation through pilots and more
- Continuity of health coverage
- Convening power
- Provider and Community Education
Medicaid Provider Levers
- Continued access to children and families during key years (0–5)
- Ability to influence family decision– making
- Connection to child & family services
- Patient data
- Practice–level policy
Recommendations must meet following criteria:
- Specifically address a foundation of health from the agreed upon framework
- Be evidence based, or at least strongly evidence informed
- Have measurable results, or include a viable strategy for collecting new data to measure results
- Reach a large percentage of the affected population or be a targeted pilot with strong potential for wider adoption
- Consider disparities in access, quality of care, and outcomes.
- Have sufficient detail to be actionable and implementable by New York Medicaid and any relevant partners
- Be affordable and cost–efficient given limited resources
- Consider the potential effect on various constituencies (including potential perverse incentives, political considerations)
|top of section| |top of page|
Lunch
|top of section| |top of page|Idea Generation
Nancy Zimpher, Chair
Kate Breslin, Vice Chair
| Long–term Goal | Key Drivers | Change Ideas | |
|---|---|---|---|
| Improve Outcomes in Learning, Behavior, and Health of NY´s Vulnerable Children During Early Childhood | |||
| ← | Universal access to basic medical care for pregnant women and children | Integrating physical and behavioral health in pediatric practices | |
| ← | Home visiting for vulnerable families | Improving OBGYN / PCP referrals to home visiting programs | |
| ← | High–quality, center based, early education | ||
| ← | Two–generation programs in health and education | Assessing parents for referral to workforce development opportunities | |
| ← | Prevention and mitigation of toxic stress in early childhood | Universal ACEs screening during first year of life | |
| ← | Economic stability supports (e.g., SNAP, TANF, EITC, child care subsidies, housing supports) | Referral of all Medicaid–eligible families to local DSS for benefit eligibility check | |
| ← | Reducing neurotoxin exposure |
Use data to drive continuous improvement and reliable implementation of effective strategies →
Source: http://developingchild.harvard.edu/resources/a–science–based–framework–for–early–childhood–policy/
Pathway to Creating a Recommendation
- What´s the outcome you are trying to improve? How does it fit into the framework?
- What is preventing us from improving in this area? What are the barriers preventing Medicaid and partners from addressing this need?
- What could work? What are the potential solutions to the identified issue (are they consistent with the primary drivers in the framework)?
- Which solutions can Medicaid effect? What Medicaid system levers could be used to implement the solution(s)?
- What´s the recommendation? How would a recommendation be framed given all of the above? What should Medicaid do?
What are your ideas?
|top of section| |top of page|Next Steps
Nancy Zimpher, Chair
Hold Your Calendar
- September 13 (webinar)
- October 11 (webinar)
- November 1 (in–person, Albany)
Next Steps
- We´ll follow up with an email summarizing the ask to this workgroup, and with specific instructions for submitting recommendation ideas for the ten– point plan.
- Join the conversation on twitter: #First1KDaysNY @NewYorkMRT
Contact Information
Chad Shearer
Vice President for Policy Director, Medicaid Institute
cshearer@uhfnyc.org (212) 494–0793
@chadeshearer
Suzanne Brundage
Program Director, Children´s Health Initiative
sbrundage@uhfnyc.org (212) 494 – 0729@suzbrundage
Appendix
Outcome Metrics for Children
Medicaid Low-Birth Weight Newborns (PQI 9):
| Year | Statewide Average (observed rate per 1,000 births) |
|---|---|
| 2012 | 68.11 |
| 2013 | 69.23 |
Source: https://health.data.ny.gov/Health/QARR–Medicaid–Child–Preventive–Care–by–Year–Beginn/jrkm–jtwz
Medicaid Managed Care Child Immunization Status (Combo 3):
| Year | Statewide average (rate) |
|---|---|
| 2009 | 73 |
| 2011 | 74 |
| 2013 | 73.3 |
| 2015 | 74.8 |
Source: https://health.data.ny.gov/Health/QARR–Medicaid–Child–Preventive–Care–by–Year–Beginn/jrkm–jtwz
Percent of children ages 4 months – 5 years at moderate or
high risk of developmental, behavioral, and social delays
based on parent concern (NSCH Survey):
| Year | New York estimate | National estimate |
|---|---|---|
| 2007 | 28.6% | 26.4% |
| 2011/2012 | 33.1% | 26.2% |
Source: http://childhealthdata.org/docs/nsch–docs/childhealthmeasures_2007vs2011–2012.pdf?sfvrsn=3
Follow Us