New York State Medicaid Update - December 2023 Volume 39 - Number 17
In this issue …
- Pharmacy
- All Providers
- Policy and Billing
- Medical Nutritional Therapy Services Provided by Qualified Dietitians/Nutritionists
- New York State Medicaid Coverage of Testing for Lynch Syndrome
- Expanded Eligibility for Community Health Worker Services
- Reimbursement for Adverse Childhood Experiences Screening
- Medicaid Practitioner Administered Drugs Update
- Medicaid Managed Care and Prescription Coverage for Undocumented Non-Citizens 65 Years of Age and Over
- New York State Medicaid Expansion of Prognostic Tests for Breast Cancer Treatment
- Clarification to Updated Billing Guidance for Vagus Nerve Stimulators
Information in gray boxes in this issue indicates material abridged but linked from the succinct interactive Portable Document Format (PDF) version.
NYRx Prior Authorization Programs Update
On September 21, 2023, the New York State (NYS) Medicaid Drug Utilization Review (DUR) Board recommended changes to the NYS Medicaid Pharmacy prior authorization (PA) programs. The Commissioner of Health (COH) has reviewed the recommendations and has approved changes to the NYRx Preferred Drug Program (PDP).
Effective December 14, 2023, PA requirements will change for some drugs in the following PDP classes:
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
- Opioids, Short Acting
- Pulmonary Arterial Hypertension (PAH) Agents, Other - Oral
- Antimigraine Agents - Other
- Antipsychotics - Injectable
- Antipsychotics - Second Generation
- Central Nervous System (CNS) Stimulants
- Multiple Sclerosis Agents
- Steroids, Topical - Medium Potency
- Steroids, Topical - High Potency
- Growth Hormones
- Sodium Glucose Co-Transporter 2 (SGLT2) Inhibitors
- Immunomodulators - Systemic Sedative Hypnotics/Sleep Agents
- Beta2 Adrenergic Agents, Inhaled, Short-Acting
- Corticosteroids - Inhaled
- Corticosteroids - Intranasal
For detailed information regarding the DUR Board and the September 21 meeting summary, providers can refer to the NYS Department of Health (DOH) Drug Utilization Review (DUR) web page.
For current information on the NYRx Pharmacy PA programs, providers can refer to the NYRx, the Medicaid Pharmacy Program Preferred Drug List, as this document contains a full listing of drugs subject to the NYRx Pharmacy programs. For practitioner-administered drug Clinical Criteria Worksheets, providers can refer to the NYS DOH "New York State Medicaid Fee-for-Service Practitioner Administered Drug Policies and Billing Guidance" web page.
To obtain a PA, prescribers must contact the Clinical Call Center at (877) 309-9493. The Clinical Call Center is available 24 hours per day, seven days per week, and staffed with pharmacy technicians and pharmacists who will work with prescribers and their agents to quickly obtain a PA.
NYS Medicaid-enrolled prescribers can also initiate PA requests using the web-based pharmacy PA request/response application, PAXpress®. PAXpress® is accessible from the eMedNY homepage, by selecting the PAXpress® button located near the bottom right side of the eMedNY homepage.
Resources:
Questions and Additional Information:
- The NYRx Education and Outreach Call Center is available Monday through Friday, excluding holidays, from 8 a.m. to 5 p.m. EST, by telephone at (833) 967-7310 and by email at NYRxEO@magellanhealth.com.
- The NYRx Education and Outreach team hosts virtual office hours every week for stakeholders to ask questions related to NYRx and care coordination. Stakeholders are encouraged to visit the Magellan Rx Management, LLC., NYRx, the Medicaid Pharmacy Program "NYRx Education & Outreach" web page, for more information.
Care Coordination and Clinical Management of Pharmacy Services for Medicaid Managed Care Enrollees
Care coordination and clinical management for Medicaid Managed Care (MMC) enrollees continue to be the responsibility of their MMC Plan. Care coordination is defined as the organization of patient care across multiple health care providers to ensure appropriate management and delivery of health care services. The goal of care coordination and clinical management is to enhance care quality, improve health outcomes, and optimize the use of health care resources. To support care coordination and clinical management activities, prior to and following the April 2023 Pharmacy Benefit Transition, the New York State (NYS) Medicaid Pharmacy program provides pharmacy utilization data to the MMC Plans. This data assists MMC Plans with enrollee care coordination, medication management and adherence, disease management, as well as enrollee and provider outreach.
MMC Plans are responsible for coordinating care and clinical management as they relate to pharmacy services and other services per the Scope of Benefits document, and as noted within the NYRx Medicaid Pharmacy Program: Post-Transition Roles & Responsibilities document.
These responsibilities include, but are not limited to, the following for all MMC enrollees:
- All oversight and maintenance activities necessary to ensure appropriate medication management, such as reviewing the pharmacy drug utilization data sent to the MMC Plans from NYRx, to avoid duplication of services between the pharmacy and medical benefit.
- Assist MMC enrollees with any activities related to coordinating their pharmacy and medical services related to drug therapy.
- Coordinate and engage with NYRx and their vendors for any pharmacy services that may impede the delivery of medical services, such as prior authorizations and medical supplies.
- MMC Plans must report any information regarding care coordination of pharmacy services to NYRx.
Providers should work with the NYS Medicaid member and MMC Plan enrollee on issues and/or concerns regarding coordinating pharmacy services. MMC Plan contact information can be found in the eMedNY New York State Medicaid Program Information for All Providers - Managed Care Information document.
Questions and Additional Information:
- Questions regarding this guidance should be directed to NYRx@health.ny.gov.
- Information regarding post-transition services that remain the responsibility of MMC Plans is listed in the Scope of Benefits document.
Reminder: Sign Up for eMedNY Training Webinars
eMedNY offers several online training webinars to providers and their billing staff, which can be accessed via computer and telephone (no travel is necessary). Valuable provider webinars offered include:
- ePACES for: Dental, Durable Medical Equipment Supplier (DME), Institutional, Nursing Home, Physician, Private Duty Nursing (PDN), Professional (Real-Time), Transportation, and Vision
- ePACES Dispensing Validation System (DVS) for DME
- ePACES Dispensing Validation System (DVS) for Rehabilitation Services
- eMedNY Website Review
- Medicaid Eligibility Verification System (MEVS)
- New Provider / New Biller
- Pharmacy - New Provider / New Biller
- Provider Enrollment Maintenance Portal - Practitioner
Webinar registration is fast and easy. To register and view the list of topics, descriptions and available session dates, providers should visit the eMedNY "Provider Training" web page. Providers are reminded to review the webinar descriptions carefully to identify the webinar(s) appropriate for their specific training needs.
Questions
All questions regarding training webinars should be directed to the eMedNY Call Center at (800) 343-9000.
Provider Reports Available on eMedNY Website
New York State (NYS) Medicaid providers may request several types of reports on eMedNY.org. The Request for Provider Reports form may be used by enrolled providers to request information regarding their NYS Medicaid file. The reports available to providers include:
- Rate Report (Institutional Providers Only)
- Locator Code Report
- Specialty Code Report
- Group Affiliation Report
The "Request for Provider Reports" tab is located under the "Provider Enrollment" tab on the eMedNY homepage.
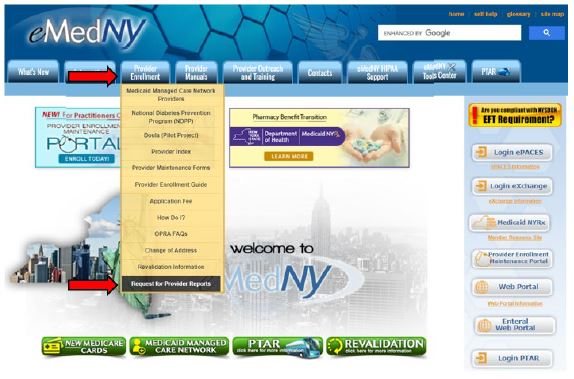
Requests for reports will be processed no more than once every six months for the same provider.
Questions
Questions should be directed to the eMedNY Call Center at (800) 343-9000.
Medicare Begins Coverage of Licensed Mental Health Counselors and Licensed Marriage Family Therapists Beginning January 1, 2024
The Centers for Medicare & Medicaid Services (CMS) expanded coverage to include Licensed Marriage and Family Therapists (LMFTs) and Licensed Mental Health Counselors (LMHCs), effective January 1, 2024. LMFTs/LMHCs providing services to New York State (NYS) Medicaid members with Medicare are required to accept Medicare assignment and bill Medicare prior to seeking reimbursement for services from NYS Medicaid. Medicare enrollment, FAQs, background information defining LMFTs/LMCHs and Medicare billing criteria can be found in the CMS Marriage and Family Therapists (MFT) and Mental Health Counselors (MHC) Provider Enrollment Frequently Asked Questions (FAQs) document.
Questions
NYS Medicaid fee-for-service (FFS) medical coverage and policy questions should be directed to the Office of Health Insurance Programs (OHIP) Division of Program Development and Management (DPDM) by telephone at (518) 473-2160 or by email at FFSMedicaidPolicy@health.ny.gov.
Medical Nutritional Therapy Services Provided by Qualified Dietitians/Nutritionists
Effective January 1, 2024, for New York State (NYS) Medicaid fee-for-service (FFS) members and Medicaid Managed Care (MMC) enrollees, NYS Medicaid will allow qualified dietitians/nutritionists to enroll and bill directly for medically necessary Medical Nutritional Therapy (MNT) provided to NYS Medicaid-eligible individuals. Dietitians/nutritionists must be certified in accordance with NYS Education Law Article 157.
MNT services are preventative health services, and as such, must be recommended by a licensed practitioner of the healing arts acting within their scope of practice under State law, to be eligible for NYS Medicaid reimbursement. Certified dietitians/nutritionists assess nutrition needs and food patterns, plan for and direct the provision of food appropriate for physical and dietary needs, provide nutrition counseling, such as advice on dietary changes, and plan menus and direct the preparation of food to meet dietary needs. A certified dietitian/nutritionist must be enrolled with the NYS Medicaid FFS program to receive NYS Medicaid reimbursement for MNT provided to a NYS Medicaid FFS or to contract with MMC Plans to serve MMC enrollees.
Certified dietitians/nutritionists providing services in an Article 28 facility must be enrolled in the NYS Medicaid FFS program as an Ordering/Prescribing/Referring/Attending (OPRA) provider and must be affiliated with the Article 28 facility for the facility to receive NYS Medicaid reimbursement for nutrition services.
NYS Medicaid Provider Enrollment Options
Dieticians/nutritionists enrollment instructions and forms will be available on the eMedNY "Provider Enrollment & Maintenance" web page, with the following options:
- Option 1: Enroll as an Individual Billing NYS Medicaid - For providers who will bill NYS Medicaid FFS.
- Option 2: Enroll as a Non-Billing-OPRA or Managed Care Network Provider - For providers who will not bill NYS Medicaid FFS.
- Option 3: Change from Non-Billing (OPRA or Managed Care Network Provider) to Billing Provider - For providers enrolled as a non-billing OPRA or MMC network provider and wish to bill NYS Medicaid FFS.
Billing
NYS Medicaid FFS
| Current Procedural Terminology (CPT) Code |
Description | Unit Description |
Unit Price |
|---|---|---|---|
| 97802 | MNT; initial assessment and intervention, individual, face-to-face with patient | each 15 minutes | $25.04 |
| 97803 | MNT; re-assessment and intervention, individual, face-to-face with patient | each 15 minutes | $21.74 |
| 97804 | MNT; group [two or more individual(s)] | each 30 minutes | $11.50 |
Please note: Other codes, not specific to nutrition services, are also available such as "T1013" (sign language or oral interpreter services, per 15 minutes).
MMC
The billing instructions and fees listed above are specific to Medicaid FFS. For individuals enrolled in MMC, providers should refer to the MMC Plan of the enrollee for implementation details, reimbursement fees and billing instructions.
Questions and Additional Information:
- Additional information can be found in the Nutrition Services Provider Manual, located on the eMedNY "Provider Manuals" web page.
- FFS billing/claim questions should be directed to the eMedNY Call Center at (800) 343-9000.
- FFS coverage and policy questions should be directed to MaternalandChild.HealthPolicy@health.ny.gov.
- MMC questions should be directed to the MMC Plan of the enrollee. MMC Plan contact information can be found in the eMedNY New York State Medicaid Program Information for All Providers - Managed Care Information document.
New York State Medicaid Coverage of Testing for Lynch Syndrome
Effective December 1, 2023, New York State (NYS) Medicaid will expand its coverage of genetic testing for Lynch syndrome deoxyribonucleic acid (DNA) mismatch repair (MMR) gene mutations (MLH1, MSH2, MSH6, and PMS2) to include Current Procedural Terminology (CPT) code "81288". This article clarifies this coverage. Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer or HNPCC, is the cause of approximately three percent (one in 30) of cases of colorectal cancer. Patients identified with Lynch syndrome have an increased risk for developing colorectal and extracolonic cancers in a variety of tissues before 50 years of age. This genetic condition is usually caused by an inherited mutation in a DNA MMR gene. First degree relatives of an individual positive for an MMR mutation have a 50 percent chance of inheriting the mutation. Approximately 70 percent of individuals affected by Lynch syndrome have mutations in the MLH1 or MSH2 gene. As a result, MSH6 testing should only be performed following a negative test result in the MLH1 and MSH2 genes.
NYS Medicaid reimbursement is available for initial screening of the MLH1 and MSH2 genes; genetic testing for Lynch syndrome mutations will be covered when one or more of the following criteria are met:
- Individuals diagnosed with colorectal cancer (CRC) under 70 years of age.
- Individuals 70 years of age or older who meet the Bethesda criteria outlined below as applicable.
- Women who were diagnosed with endometrial cancer at less than 50 years of age.
- Individuals who meet the Amsterdam II criteria.
| CPT Code | Description |
|---|---|
| 81288 | MLH1 (MUTL HOMOLOG 1, COLON CANCER, NONPOLYPOSIS TYPE 2) (E.G., HEREDITARY NONPOLYPOSIS COLORECTAL CANCER, LYNCH SYNDROME) GENE ANALYSIS; PROMOTER METHYLATION |
| 81292 | MLH1 (MUTL HOMOLOG 1, COLON CANCER, NONPOLYPOSIS TYPE 2) (EG, HEREDITARY NON-POLYPOSIS COLORECTAL CANCER, LYNCH SYNDROME) GENE ANALYSIS; FULL SEQUENCE ANALYSIS |
| 81294 | MLH1 (MUTL HOMOLOG 1, COLON CANCER, NONPOLYPOSIS TYPE 2) (EG, HEREDITARY NON-POLYPOSIS COLORECTAL CANCER, LYNCH SYNDROME) GENE ANALYSIS; DUPLICATION/DELETION VARIANTS |
| 81295 | MSH2 (MUTS HOMOLOG 2, COLON CANCER, NONPOLYPOSIS TYPE 1) (EG, HEREDITARY NON-POLYPOSIS COLORECTAL CANCER, LYNCH SYNDROME) GENE ANALYSIS; FULL SEQUENCE ANALYSIS |
| 81297 | MSH2 (MUTS HOMOLOG 2, COLON CANCER, NONPOLYPOSIS TYPE 1) (EG, HEREDITARY NON-POLYPOSIS COLORECTAL CANCER, LYNCH SYNDROME) GENE ANALYSIS; DUPLICATION/DELETION VARIANTS |
| 81298 | MSH6 (MUTS HOMOLOG 6 YE, COLI") (EG, HEREDITARY NON-POLYPOSIS COLORECTAL CANCER, LYNCH SYNDROME) GENE ANALYSIS; FULL SEQUENCE ANALYSIS |
| 81300 | MSH6 (MUTS HOMOLOG 6 YE, COLI") (EG, HEREDITARY NON-POLYPOSIS COLORECTAL CANCER, LYNCH SYNDROME) GENE ANALYSIS; DUPLICATION/DELETION VARIANTS |
| 81317 | PMS2 (POSTMEIOTIC SEGREGATION INCREASED TWO YS. CEREVISIAE") (EG, HEREDITARY NON-POLYPOSIS COLORECTAL CANCER, LYNCH SYNDROME) GENE ANALYSIS; FULL SEQUENCE ANALYSIS |
| 81319 | PMS2 (POSTMEIOTIC SEGREGATION INCREASED TWO YS. CEREVISIAE") (EG, HEREDITARY NON-POLYPOSIS COLORECTAL CANCER, LYNCH SYNDROME) GENE ANALYSIS; DUPLICATION/DELETION VARIANTS |
Additional information on NYS Medicaid coverage of Lynch syndrome testing and specific criteria referenced above can be found in the New York State Medicaid Coverage of Testing for Lynch Syndrome article published in the October 2015 issue of the Medicaid Update. Providers can also refer to the NYS Medicaid Laboratory Services Fee Schedule.
Questions and Additional Information:
- FFS coverage and policy questions should be directed to the Office of Health Insurance Programs (OHIP) Division of Program Development and Management (DPDM) by telephone at (518) 473-2160 or by email at FFSMedicaidPolicy@health.ny.gov.
- FFS billing/claim questions should be directed to the eMedNY Call Center at (800) 343-9000.
- MMC reimbursement, billing, and/or documentation requirement questions should be directed to the specific MMC Plan of the enrollee. MMC Plan contact information can be found in the eMedNY New York State Medicaid Program Information for All Providers - Managed Care Information document.
- Additional laboratory information, as well as coding and billing guidance, is available in the New York State Medicaid Program Fee-for-Service Laboratory Procedure Codes and Coverage Guidelines Manual.
Expanded Eligibility for Community Health Worker Services
Effective January 1, 2024, for New York State (NYS) Medicaid fee-for-service (FFS) and for NYS Medicaid Managed Care (MMC) Plans [inclusive of Mainstream MMC Plans, Human Immunodeficiency Virus-Special Needs Plans (HIV-SNPs), as well as Health and Recovery Plans (HARPs)], NYS Medicaid will expand the populations eligible for Community Health Worker (CHW) services beyond pregnant and postpartum populations, to include all children under 21 years of age, adults with chronic conditions, justice-involved individuals, those with unmet health-related social care needs, and individuals experiencing community violence. NYS Medicaid members are eligible for CHW services during pregnancy and up to 12 months after the end of pregnancy, regardless of the pregnancy outcome.
A Community Health Worker (CHW) is a public health worker, not otherwise recognized as a licensed or certified NYS Medicaid provider type, that reflects the community served through lived experience that may include but is not limited to, pregnancy and birth; housing status; mental health conditions; substance use or other chronic conditions; shared race, ethnicity, language, and/or sexual orientation; or community of residence. The CHW functions as a liaison between health care systems, social services, and community-based organizations to improve overall access to services and resources and to facilitate improved health outcomes for the populations served.
Covered CHW services include health advocacy, health education, and health navigation supports aimed at improving health outcomes and overall health literacy, and preventing the development of adverse health conditions, injury, illness, or the progression thereof. Individual or group based CHW services are defined as direct interaction with the eligible NYS Medicaid member or group of members.
At this time, CHWs will not enroll in or bill NYS Medicaid directly. CHW services are billed by the supervising NYS Medicaid-enrolled clinician, entity, or facility identified below:
- Clinic
- Hospital Outpatient Department (HOPD)
- Physician
- Midwife (MW)
- Nurse Practitioner (NP)
- Psychologist
- Licensed Clinical Social Worker (LCSW)
- Licensed Mental Health Counselor (LMHC)
- Licensed Marriage Family Therapist (LMFT)
Additional provider types (e.g., health homes) may be identified at the discretion of the NYS Department of Health (DOH).
CHW services are preventative health services, and as such, must be recommended by a physician or other licensed practitioner of the healing arts acting within their scope of practice under State law, to be eligible for NYS Medicaid reimbursement.
NYS Medicaid covers CHW services for the following NYS Medicaid FFS members and MMC enrollees:
- children under 21 years of age;
- pregnant and postpartum individuals during pregnancy, and up to 12 months after pregnancy ends, regardless of the pregnancy outcome;
- adults with chronic conditions;
- individuals with justice system involvement within the past 12 months;
- individuals with an unmet health-related social need in the domains of housing, nutrition, transportation, or interpersonal safety, which have been identified through screening using the Centers for Medicare & Medicaid Services (CMS) Accountable Health Communities Health-Related Social Needs Screening Tool; and
- individuals who have been exposed to community violence or have a personal history of injury sustained as a result of an act of community violence, or who are at an elevated risk of violent injury or retaliation resulting from another act of community violence.
Please note: NYS Medicaid members who receive care coordination services through the Health Home program, a Health Home Care Coordination Organization (CCO - Health Home), certified community behavioral health clinics (CCBHCs), Assertive Community Treatment (ACT), are not eligible for CHW service coverage at this time. NYS Medicaid members who do not receive care coordination through these entities are eligible for CHW service coverage. NYS Medicaid members in institutional settings are not eligible for CHW service coverage.
NYS Medicaid FFS Billing:
- Article 28 freestanding clinics and HOPDs can bill for CHW services using the codes below on Ambulatory Patient Groups (APG) claim.
- Federally Qualified Health Centers (FQHCs) may bill for CHW services only if the FQHC has elected to be reimbursed under APGs when the CHW service is provided in conjunction with a threshold visit with a licensed health care provider.
- When billing for CHW services that are not community violence prevention services, modifiers U1 and U3 must be included consecutively, in this order, on the claim line when seeking reimbursement for Current Procedural Terminology (CPT) codes "98960", "98961", or "98962".
- For community violence prevention services provided by a CHW, modifiers U3 and U1 must be included consecutively, in this order, on the claim line when seeking reimbursement for CPT codes "98960", "98961", or "98962".
- For individuals 21 years of age and older, providers must include a diagnosis on the claim that identifies the chronic condition, social care need, or qualifying risk criteria of the NYS Medicaid member using the appropriate diagnostic code / International Classification of Diseases, or Tenth Revision (ICD-10) Z codes.
| Code | Modifier | Description | Annual Allowance Per NYS Medicaid Member |
Reimbursement Rate |
|---|---|---|---|---|
| 98960 | U1, U3 | Self-management education and training face-to-face using a standardized curriculum for an individual NYS Medicaid member, each 30 minutes. | 12 units total for adult populations 24 units total for pediatric population (under 21 years of age) (30 minutes = 1 unit*) |
$35.00 |
| 98961 | U1, U3 | Self-management education and training face-to-face using a standardized curriculum for two to four NYS Medicaid members, each 30 minutes. | $16.45 | |
| 98962 | U1, U3 | Self-management education and training face-to-face using a standardized curriculum for five to eight NYS Medicaid members, each 30 minutes. | $12.25 |
*One unit must be a minimum of 16 minutes with a maximum of 37 minutes.
Please note: For community violence prevention services, modifier combination U3 and U1 must be used, in this order, on claim line when seeking reimbursement for CPT Codes "98960", "98961", or "98962".
MMC Billing Instructions
For NYS Medicaid members enrolled in an MMC Plan, providers must contact the MMC Plan of the enrollee for billing instructions. MMC Plan contact information can be found in the eMedNY New York State Medicaid Program Information for All Providers - Managed Care Information document.
Questions and Additional Information:
- Additional information can be found in the Community Health Worker Policy Manual, located on the eMedNY "Provider Manuals" web page.
- FFS claim questions should be directed to the eMedNY Call Center at (800) 343-9000.
- FFS coverage and policy questions should be directed to MaternalandChild.HealthPolicy@health.ny.gov.
- MMC questions should be directed to the MMC Plan of the enrollee. MMC Plan contact information can be found in the eMedNY New York State Medicaid Program Information for All Providers - Managed Care Information document..
Reimbursement for Adverse Childhood Experiences Screening
Effective January 1, 2024, for New York State (NYS) Medicaid fee-for-service (FFS), and effective April 1, 2024, for Medicaid Managed Care (MMC) Plans [including mainstream MMC Plans, and Human Immunodeficiency Virus-Special Needs Plans (HIV-SNPs)], NYS Medicaid provides reimbursement for Adverse Childhood Experiences (ACEs) screening conducted in primary care settings for children and adolescents up to 21 years of age. An annual ACEs screening will be covered, as determined appropriate and medically necessary.
ACEs are strongly related to brain development and a wide range of health problems throughout the lifetime of an individual. ACEs have been associated with chronic conditions in adulthood, such as obesity, cancer, depression, and substance misuse. Positive Childhood Experiences (PCEs) are protective factors and can mitigate ACEs and promote resiliency. A critically important component of screening includes conversations with youth and caregivers in identifying PCEs to build resilience. NYS Medicaid recommends integrating protective factors into ACEs screening.
ACEs are categorized into three experience groups: abuse, neglect, and household challenges. These include emotional, physical, and sexual abuse; emotional and physical neglect; and household challenges that include exposure to domestic violence, a family member with household substance abuse, a family member with mental illness, an incarcerated household member, or parental separation or divorce.
ACEs screening should take place in the context of trauma-informed care to ensure a safe, empowering environment for the child and family. Trauma-informed care enables responsiveness to specific ACE(s) of a child by enhancing prevention education and activities, such as recommended treatment interventions and connections to community supports and services, as guided by the interests and needs of the child and family. Screening for ACEs is always voluntary, to minimize the risk of retraumatizing the individual/family. Parents/caregivers should complete the ACEs screening on behalf of children under 13 years of age.
Eligible providers are licensed or unlicensed individuals under the supervision of a licensed provider, with training and experience using the screening tools and delivery of trauma-informed care. Providers conducting the screening must use a research-based screening tool to assess the exposure to adversity and factors that influence risk for associated negative outcomes of the child. Providers and practice sites should consider which screening/assessment tool to use, who should administer the tool and how, and which NYS Medicaid members should be screened. NYS Medicaid also recommends integrating screening for protective factors as a component of ACEs screening. Suggested screening tools and guidance are shown below.
Specific ACEs do not need to be recorded; however, identification of the screening tool and positive or negative result must be documented. Following administration, the provider reviews the screen results along with the patient and parent/caregiver history. If the screen is determined to be positive for ACEs, based on provider discretion, the provider must consider the factors that influence the risk of the child for associated negative outcomes, along with PCEs, and develop a treatment plan in partnership with the patient or parent/caregiver. Medical practices should ensure that they have the capacity to evaluate and treat children who screen positive for ACEs before implementing standardized screening. Providers are expected to make referrals to appropriate resources, such as mental health providers or community-based organizations, for any needs identified or requested as the result of the screening.
ACEs Screening Tool Examples
Use of a research-based tool is required when screening for ACEs to be eligible for NYS Medicaid reimbursement. Health care practices should adopt the tool that meets the needs of their population and clinical workflow. Examples of recommended screening tools include:
- modified ACEs questionnaire based on the original Centers for Disease Control and Prevention (CDC)-Kaiser Permanente ACEs study (providers should refer to 1 and 2 of the "References" section below);
- part 1 of the Pediatric ACEs and Related Life Events Screener (PEARLS) - Child tool, for individuals zero to 19 years of age, to be completed by the parent/caregiver or by the youth based on the age of the patient (providers should refer to 2 of the "References" section below); and
- Adverse Childhood Experiences Questionnaire for Adults, for individuals 18 to 21 years of age, to be completed by the patient (providers should refer to 2 of the "References" section below).
References:
Billing
NYS Medicaid FFS:
- The supervising licensed provider (billing provider) must be enrolled as a NYS Medicaid provider and obtain a National Provider Identifier (NPI).
- ACEs screening is reimbursed one time annually for NYS Medicaid members from birth to 21 years of age.
- Approved categories of service and providers:
- Physicians ("0460")
- Nurse Practitioners (NPs) ("0469")
- Ordered Ambulatory
- Clinic ("0163")
- Hospital Outpatient Department (HOPD) ("0282")
ACEs screening is included within the Prospective Payment System (PPS) primary care rate for Federally Qualified Health Centers (FQHCs).
| Code | Modifier | Description | Annual Allowance Per NYS Medicaid Member |
Reimbursement Rate |
|---|---|---|---|---|
| G9919 | U1 and U9 | Screening was performed and positive*, provision of recommendations is used for high-risk patients. | 1 Screen | $29.00 |
| G9920 | Screening was performed and negative. |
*Clinician to determine if an ACEs screen is positive.
MMC
The billing instructions and fees listed in the chart are specific to NYS Medicaid FFS. For individuals enrolled in MMC, providers should refer to the MMC Plan of the individual for implementation details, reimbursement fees and billing instructions.
Suggested Resources:
- NYS Office of Children and Family Services (OCFS) "Adverse Childhood Experiences (ACEs)" web page;
- CDC Violence Prevention "Adverse Childhood Experiences" web page;
- CDC 2022 BRFSS Questionnaire (see module 15, pages 95 through 98).
- ACEs Aware "Screening Tools" web page;
- Project TEACH (Training and Education for the Advancement of Children's Health) is a statewide program that supports reproductive, primary care, and pediatric clinicians to deliver quality mental health care in NYS. The program strives to strengthen and support the delivery of care to children, families, and individuals who experience mental health concerns. Education, resources, and primary care provider consultations with child, adolescent, and maternal psychiatrists are available.
- Project TEACH "Provider Resources" web page;
- Project TEACH "About" web page;
- For consultations with a child, adolescent, or maternal psychiatrist, contact (855) 227-7272;
- Medicaid Update articles:
- Project TEACH Maternal Mental Health Services article published in the January 2023 issue of the Medicaid Update;
- Understanding How Adverse Childhood Experiences Affect Patients' Health Across the Lifespan article published in November 2022 issue of the Medicaid Update.
Questions and Additional Information:
- NYS Medicaid FFS claim questions should be directed to the eMedNY Call Center at (800) 343-9000.
- NYS Medicaid FFS coverage and policy questions should be directed to the Office of Health Insurance Programs (OHIP) Division of Program Development and Management (DPDM) by telephone at (518) 473-2160 or by email at FFSMedicaidPolicy@health.ny.gov.
- MMC reimbursement, billing, and/or documentation requirement questions should be directed to enrollee MMC Plans. MMC Plan contact information can be found in the eMedNY New York State Medicaid Program Information for All Providers - Managed Care Information document.
Medicaid Practitioner Administered Drugs Update
Effective January 18, 2024, the coverage criteria for SKYSONA® (elivaldogene autotemcel) and HEMGENIX® (etranacogene dezaparvovec-drlb) are as follows:
SKYSONA® (elivaldogene autotemcel)
- The patient is a candidate for hematopoietic stem cell transplant (HSCT), but ineligible due to the absence of a donor.
- The patient does not have human immunodeficiency virus (HIV) or human T-lymphotropic virus (HTLV).
- The patient is not utilizing anti-retroviral drugs at least one month prior to initiating medications for stem cell mobilization and until all cycles of apheresis are completed.
HEMGENIX® (etranacogene dezaparvovec-drlb)
- The patient must have a confirmation of moderately severe to severe, congenital hemophilia B.
- The patient does not have a history of factor IX inhibitors.
- The patient does not have a positive factor IX inhibitor test.
Practitioner Administered Drug (PAD) Clinical Criteria Worksheets are available on the New York State (NYS) Department of Health (DOH) "New York State Medicaid Fee-for-Service Practitioner Administered Drug Policies and Billing Guidance" web page. For more information regarding the development of the coverage criteria above, providers should refer to the NYS DOH "Drug Utilization Review (DUR) Board - 2023" web page.
Billing
Fee-for-Service
Coverage for the aforementioned drugs will be provided through the medical benefit. Drugs listed in the NYS Medicaid Physician Drug and Drug Administration Services Fee Schedule, with a notation of BR (By Report) under the "Maximum Fee" column, must use the Medical Assistance Health Insurance Claim Form (eMedNY 150003 form), via paper with a copy of the itemized invoice that must be dated within six months prior to the date of service and/or should include the expiration date of the drug. Additional information can be found in the New York State Medicaid General Billing Guidelines document.
Medicaid Managed Care
Individual Medicaid Managed Care (MMC) Plans should be contacted for their specific reimbursement and billing guidance. MMC Plan information can be found in the eMedNY New York State Medicaid Program Information for All Providers - Managed Care Information document.
Questions and Additional Information:
- Fee-for-service (FFS) billing and claim questions should be directed to the eMedNY Call Center at (800) 343-9000.
- FFS pharmacy and PAD coverage policy questions should be directed to the Medicaid Pharmacy Policy Unit by telephone at (518) 486-3209 or by email at NYRx@health.ny.gov.
- Information regarding the DUR Board is available on the NYS DOH "Drug Utilization Review (DUR)" web page.
- Additional information can be found at the following web pages:
Medicaid Managed Care and Prescription Coverage for Undocumented Non-Citizens 65 Years of Age and Over
Effective January 1, 2024, undocumented non-citizens who are 65 years of age and older are eligible for comprehensive health insurance coverage through a mainstream Medicaid Managed Care Plan. Previously, this population qualified for New York State (NYS) Medicaid coverage for the treatment of an emergency medical condition, only. NYS Social Services Law §366.1(g)(4)(a), was amended to authorize this new coverage to undocumented non-citizens 65 years of age and older, who are otherwise eligible (e.g., income eligible, NYS resident) except for their immigration status. Consumers eligible for this expanded coverage will also access pharmacy benefits through NYRx, the Medicaid Pharmacy program.
To implement this new and expanded coverage, several new codes have been developed: a new Client Category of Eligibility (COE) Aid Category Code and two new COE Medicaid Coverage Codes, which are as follows:
- "37" - Medicaid Eligibility Verification System (MEVS) response will read "Eligible PCP, 65 and over with pharmacy carve out."
- "38" - MEVS response will read "Eligible Fee-for-Service, 65 and over, pharmacy, emergency only."
Consumers will only have coverage code "38" for a brief period to facilitate enrollment into their MMC Plan. During the time they are enrolled with coverage code "38", consumers are eligible for NYS Medicaid per the treatment of an emergency medical condition and pharmacy benefits through NYRx. Once enrolled in their MMC Plan, enrollees will be assigned coverage code "37" and will be eligible for covered plan services and pharmacy benefits through NYRx.
Questions
Questions regarding the coverage expansion or eligibility should be directed to MCfor65PlusUndoc@health.ny.gov.
New York State Medicaid Expansion of Prognostic Tests for Breast Cancer Treatment
Effective December 1, 2023, New York State (NYS) Medicaid will expand its coverage of prognostic breast cancer assays eligible for reimbursement for NYS Medicaid fee-for-service (FFS) and Medicaid Managed Care (MMC) to include Breast Cancer Index® (BCI) and MammaPrint®, in addition to Oncotype DX®, EndoPredict® and Prosigna®. Breast Cancer Index®, MammaPrint®, Oncotype DX®, EndoPredict®, and Prosigna® prognostic gene expression tests assist practitioners in making determinations regarding the effective and appropriate use of chemotherapy in female or male patients with malignant neoplasms of the breast, when all the following criteria are met:
- The test results will aid the patient and practitioner in making the decision regarding chemotherapy (i.e., when chemotherapy is a therapeutic option and is not precluded due to any other factor).
- The tumor is estrogen receptor positive (ER+), progesterone receptor positive (PR+), or both.
- The tumor is human epidermal growth factor receptor 2 (HER2) negative.
- The tumor is T1 or T2.
- The tumor is node-negative or one to three positive nodes.
Please note: NYS Medicaid criteria for Breast Cancer Index®, MammaPrint®, Oncotype DX®, EndoPredict® and Prosigna® tests is in accordance with current National Comprehensive Cancer Network (NCCN) guidelines. In between policy reviews, providers are encouraged to follow the most recent NCCN guidance.
Additional information on NYS Medicaid coverage of prognostic breast cancer assays may be found in the New York State Medicaid Expansion of Prognostic Tests for Breast Cancer Treatment article published in the July 2019 issue of the Medicaid Update.
Questions and Additional Information:
- FFS coverage and policy questions should be directed to the Office of Health Insurance Programs (OHIP) Division of Program Development and Management (DPDM) by telephone at (518) 473-2160 or by email at FFSMedicaidPolicy@health.ny.gov.
- FFS billing/claim questions should be directed to the eMedNY Call Center at (800) 343-9000.
- MMC reimbursement, billing, and/or documentation requirement questions should be directed to the specific MMC Plan of the enrollee. MMC Plan contact information can be found in the eMedNY New York State Medicaid Program Information for All Providers - Managed Care Information document.
- Additional laboratory information and billing guidance is available in the eMedNY New York State Medicaid Program Fee-for-Service Laboratory Procedure Codes and Coverage Guidelines Manual.
Clarification to Updated Billing Guidance for Vagus Nerve Stimulators
This article clarifies billing guidance for Vagus Nerve Stimulator (VNS) devices provided in the Updated Billing Guidance for Vagus Nerve Stimulators article published in the May 2023 issue of the Medicaid Update.
Facilities are to continue to submit an Ambulatory Patient Group (APG) claim to be reimbursed for the surgical procedure. To be reimbursed for the VNS device, providers should submit an ordered ambulatory claim under Current Procedural Terminology (CPT) code "64999" with the following documentation:
- copy of the operative report showing implantation of the device; and
- copy of the invoice showing the acquisition cost to the facility, less any manufacturer rebates.
Any facility who has submitted for the VNS device using CPT code "64999" within the APG band after July 1, 2023, may have been underpaid. Providers should adjust their APG claim, remove CPT code "64999" from their APG claim, and resubmit a separate ordered ambulatory claim for the VNS device as directed above.
Questions and Additional Information:
- NYS Medicaid fee-for-service (FFS) coverage and policy questions should be directed to the Office of Health Insurance Programs (OHIP) Division of Program Development and Management (DPDM) by telephone at (518) 473-2160 or by email at FFSMedicaidPolicy@health.ny.gov.
- NYS Medicaid FFS claim questions should be directed to the eMedNY Call Center at (800) 343-9000.
- Medicaid Managed Care (MMC) general coverage questions may be directed to OHIP Division of Health Plan Contracting and Oversight (DHPCO) by email at covques@health.ny.gov or by telephone at (518) 473-1134.
- MMC reimbursement and/or billing requirements questions should be directed to the MMC Plan of the enrollee. Providers can refer to the eMedNY New York State Medicaid Program Information for All Providers - Managed Care Information document, for MMC Plan information.
The Medicaid Update is a monthly publication of the New York State Department of Health.
Kathy Hochul
Governor
State of New York
James McDonald, M.D., M.P.H.
Commissioner
New York State Department of Health
Amir Bassiri
Medicaid Director
Office of Health Insurance Programs