New York State Medicaid Update - April 2023 Volume 39 - Number 8
In this issue …
- All Providers
- Policy and Billing
- Home Health Care Medicare Maximization Initiative Reminder: Medicare Third Party Liability Demand Billing
- Attention: Transportation Providers
- Attention Family Planning Providers: New York State Medicaid-Covered Long-Acting Reversible Contraceptives
- Proper Billing for the Recipient Restriction Program
- Reminder of the New York State Medicaid Policy for Durable Medical Equipment Prosthetics, Orthotics, and Supplies for Members in Residing in Nursing Homes
- Pharmacy
eMedNY "Provider Outreach and Training" Resource Tab
Providers are encouraged to routinely use the "Provider Outreach and Training" tab located on the eMedNY homepage, as it contains useful billing resources, training information, contacts, and additional reference documents for provider billing and training needs.
The eMedNY "Provider Training" web page also contains a calendar of upcoming webinars which cover a variety of topics, such as New Provider/New Biller, ePACES, Medicaid Eligibility Verification System (MEVS), and more. Providers that are unable to attend training sessions can conveniently access training videos as their schedule permits. Providers with additional training needs should contact the eMedNY Call Center at (800) 343-9000.
Reminder: Sign Up for eMedNY Training Webinars
eMedNY offers several online training webinars to providers and their billing staff, which can be accessed via computer and telephone. Valuable provider webinars offered include:
- Provider Enrollment Portal - Practitioner
- ePACES for: Dental, Durable Medical Equipment Supplier (DME), Institutional, Physician, Private Duty Nursing, Professional (Real-Time), and Transportation
- ePACES Dispensing Validation System (DVS) for DME
- eMedNY Website Review
- Medicaid Eligibility Verification System (MEVS)
- New Provider / New Biller
- Pharmacy - New Provider / New Biller
Webinar registration is fast and easy. To register and view the list of topics, descriptions and available session dates, providers should visit the eMedNY "Provider Training" web page. Providers are reminded to review the webinar descriptions carefully to identify the webinar(s) appropriate for their specific training needs.
Questions
All questions regarding training webinars should be directed to the eMedNY Call Center at (800) 343-9000.
Home Health Care Medicare Maximization Initiative Reminder: Medicare Third Party Liability Demand Billing
The New York State (NYS) Office of the Medicaid Inspector General (OMIG) contracts with the University of Massachusetts Chan Medical School (UMass Chan) to perform Medicare Home Health Maximization for dual-eligible Medicare/Medicaid members. For these dually eligible members, NYS OMIG identifies home health services that were previously paid by Medicaid and directs the provider to "demand bill" Medicare for the services. Providers identified in the Medicare Home Health Maximization initiative will receive official notification from OMIG/UMass Chan requesting the disputed claims be demand billed to Medicare for a full medical review and coverage determination.
When submitting the demand bill claims to Medicare, providers are required to comply with all Medicare conditions of payment and claiming instructions to avoid payment liability for the services. Providers must submit all documentation requested by the Medicare Administrative Contractor (MAC) necessary for medical review. All claims must be monitored; and corrections are required for any claims rejected or suspended by the MAC. Failure to comply with all Medicare claims and documentation submission and/or billing requirements may result in an audit to recoup the amount reimbursed by the medical assistance program.
Questions and Additional Information:
- Questions regarding submitting demand bills to Medicare, including information on filing timeframes, should be directed to the local MAC of the provider.
- For additional development requests and required documentation, as well as claims submission errors, providers should contact their local MAC.
Attention: Transportation Providers
Effective April 20, 2023, a new system edit #02343 in eMedNY went into effect for up front screening of the vehicle license plate number and driver's license number fields on Transportation claims submissions. The new system edit automatically denies any claim submission where there is a special character or symbol in either the vehicle license plate number field or the driver's license number field. Providers can rebill any denied claims for this edit with the correct information in the vehicle plate number field and the driver's license number field.
Billing Reminder for New York State Medicaid Providers Submitting Claims for Transportation Services
The New York State (NYS) Department of Motor Vehicles (DMV) allows up to eight numbers, letters, or spaces in a vehicle license plate number (the driver's license number is nine characters in length). Special characters or symbols are not allowed in either a vehicle license plate number or a NYS DMV driver's license number. Providers should follow the NYS Medicaid provider billing guidelines when submitting Transportation claims requiring vehicle license plate number and a driver's license number.
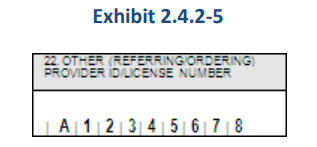
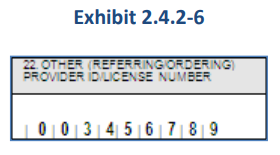
Please note: When reporting an out-of-state driver's license number with more than nine characters, only the first nine characters should be reported. Exhibit 2.4.2-5 below shows an entry where the driver's license is "A123456789B". If a driver's license number contains fewer than nine characters, the entry must be right justified and zero-filled to complete the nine characters. Exhibit 2.4.2-6 below shows an entry where the driver's license is "3456789". Special characters or symbols are not allowed in a vehicle plate or DMV driver's license number.
For additional information, providers can refer to the eMedNY New York State Billing Guidelines - Transportation.
Ambulette and Taxi/Livery Providers
As a reminder, effective March 1, 2016, in addition to historically required acceptable trip verification, the NYS Department of Health (DOH) requires the full printed name and signature of the driver providing the transport attesting that the referenced trip was completed. The full list of required trip verification information includes, at a minimum:
- the name and NYS Medicaid identification number for the NYS Medicaid member;
- the date of transport;
- the origination of the trip and time of pickup;
- the destination of the trip and time of drop off;
- the vehicle license plate number;
- the driver's license number;
- the full printed name and signature of the driver providing the transport; and
- an attestation from the driver that the trip was completed.
The use of electronic record-keeping methodology is becoming more prevalent. Transportation vendors using electronic methods to prepare and maintain contemporaneous documentation to support NYS Medicaid claims must produce documentation with an accurate system-generated, unmodifiable date and time stamp for each leg of a billable trip including the pickup and drop-off, as well as driver attestation as required.
Attention Family Planning Providers: New York State Medicaid-Covered Long-Acting Reversible Contraceptives
The New York State (NYS) Medicaid program provides coverage for United States (U.S.) Food and Drug Administration (FDA)-approved birth control methods, devices, and supplies [e.g., birth control pills, injectables, patches, condoms, diaphragms, implantables, and intrauterine devices (IUDs)]. Long-acting reversible contraceptives (LARCs), such as IUDs and contraceptive implants shown in chart below, are the most effective forms of contraceptives covered by NYS Medicaid.
Procedure Code LARC Description J7296 Levonorgestrel-releasing intrauterine contraceptive system, 19.5 mg, (Kyleena®) J7297 Levonorgestrel-releasing intrauterine contraceptive system, 52 mg, three-year duration (Liletta®) J7298 Levonorgestrel-releasing intrauterine contraceptive system, 52 mg, five-year duration (Mirena®) J7300 Intrauterine copper contraceptive (Paragard®) J7301 Levonorgestrel-releasing intrauterine contraceptive system, 13.5 mg, three-year duration (Skyla®) J7306 Levonorgestrel (contraceptive) implant system, including implants and supplies J7307 Etonogestrel (contraceptive) implant system, including implant and supplies (Implanon™ or Nexplanon®) One major advantage of LARCs is that they do not require ongoing effort on the part of the user for long-term and effective use. Medicaid Managed Care (MMC) members may receive family planning and reproductive health services, including abortion services, from any qualified NYS Medicaid provider inside or outside their health plan, without prior approval from the health plan or primary care provider, as long as the provider accepts NYS Medicaid and offers the needed services.
Prior approval (PA) is not required for any LARC, or other birth control method, device, or supply covered by NYS Medicaid FFS. NYS Medicaid FFS reimbursement for LARC is based on the acquisition cost of the provider (actual, invoiced cost). For important claims processing rules, providers should refer to the Reasonability Edits for Practitioner-Administered Drugs article published in the August 2015 issue of the Medicaid Update. Additional information can be found in the eMedNY New York State Medicaid Program Physician - Procedure Codes - Section 2 - Medicine, Drugs, and Drug Administration manual.
Additional Information:
- Hospital outpatient department clinics and free-standing diagnostic and treatment centers (D&TCs) with the designated category of service of "0163" (ordered ambulatory diagnostic and treatment center) or "0282" (hospital-based ordered ambulatory) may bill the invoiced LARC cost as an ordered ambulatory service.
- The cost of LARC is carved out of Ambulatory Patient Group (APG) facility reimbursement and the prospective payment system (PPS) reimbursement of Federally Qualified Health Centers (FQHCs).
- Hospitals may bill for the cost of the LARC provided to NYS Medicaid FFS members during a postpartum inpatient hospital stay. LARCs provided during an inpatient stay can be billed to NYS Medicaid on an ordered ambulatory claim, separate from the inpatient claim. Additional information can be found in the eMedNY Inpatient Clarification on Reimbursement for Long Acting Reversible Contraception (LARC) Provided as an Inpatient Post-Partum Service document. MMC Plans also cover immediate postpartum LARC separately from reimbursement for the inpatient stay.
- NYS Medicaid FFS billing guidelines for IUDs and contraceptive implants can be found in the applicable provider policy and billing manuals, located on the eMedNY homepage, and in the eMedNY New York State Medicaid Family Planning and Reproductive Health Services - Frequently Asked Questions document.
- Beginning April 1, 2023, NYS Medicaid members enrolled in mainstream MMC Plans, Health and Recovery Plans (HARPs), and Human Immunodeficiency Virus-Special Needs Plans (HIV-SNPs) will have their pharmacy benefits transitioned to NYRx, the NYS Medicaid Pharmacy program. For more information, visit the NYS Department of Health (DOH) "Welcome to the NY Medicaid Pharmacy Program (NYRx)" web page. The transition will not apply to NYS Medicaid members enrolled in Managed Long Term Care (MLTC) Plans [e.g., Programs of All-Inclusive Care for the Elderly (PACE), Medicaid Advantage Plus (MAP), MLTC Plans, Essential Plan (EP), or Child Health Plus (CHPlus)].
Questions:
- Questions on billing or claims should be directed to the eMedNY Call Center at (800) 343-9000.
- Policy questions regarding NYS Medicaid FFS may be directed to the Office of Health Insurance Programs (OHIP) Division of Program Development and Management (DPDM) by telephone at (518) 473-2160 or by email at maternalandchild.healthpolicy@health.ny.gov.
- MMC enrollment, reimbursement, billing, and/or documentation requirement questions should be directed to the specific MMC Plan of the enrollee. MMC Plan contact information can be found in the eMedNY New York State Medicaid Program Information for All Providers - Managed Care Information document.
- NYRx, billing policy and other pharmacy-related information can be found in the NYS MMIS Pharmacy Provider Manual, located on the eMedNY "Pharmacy Manual" web page, and the Medicaid Update. Providers may also email NYRx@health.ny.gov or call (518) 486-3209, for NYS Medicaid pharmacy policy-related questions.
Proper Billing for the Recipient Restriction Program
The Recipient Restriction Program (RRP) is a medical review and administrative mechanism whereby New York State (NYS) Medicaid members with a demonstrated pattern of abusing or misusing NYS Medicaid services may be restricted to a specific healthcare provider (i.e., hospital, clinic, physician) or pharmacy to coordinate services. RRP is administered by the Office of the Medicaid Inspector General (OMIG) in coordination with local Departments of Social Services (LDSS). The objectives of RRP include:
- providing NYS Medicaid members with coordinated medical and pharmacy services, thus improving the quality of their care;
- reducing the inappropriate utilization of health care by identifying NYS Medicaid members exhibiting abusive or fraudulent behavior; and
- utilizing Medicaid Managed Care (MMC) Plans and community providers to provide specific specialty and case management services. MMC Plans may add or modify restrictions only with the approval of OMIG.
NYS Medicaid members who have been restricted as part of RRP to a designated health care provider (i.e., physician or clinic, hospital) or pharmacy are required to receive care only from the designated health care provider or pharmacy. A primary pharmacy is responsible for identifying the ordering prescriber and managing the delivery of medications.
It is important to remember that the primary health care provider, whether a physician, hospital, or clinic, is responsible for the provision of most health care services for the restricted NYS Medicaid member. A referral will be needed from these primary health care providers for any non-emergency medical services rendered by similar providers, including the ordering of transportation or prescriptions.
When a restricted NYS Medicaid member is assigned to a designated provider and pharmacy, the provider and pharmacy will receive a letter informing them that the restricted NYS Medicaid member is restricted to them. The letter also details the referral process. Additionally, the recipient is notified via the Notice of Intent to Restrict, which informs them of their restriction, their assigned providers, as well as their fair hearing instructions.
Claims submitted for a restricted NYS Medicaid member will be denied if the information of the primary care provider is not included on the claim as the referring provider. Providers with questions regarding the submission of claims should contact eMedNY Provider Services at (800) 343-9000 or refer to the provider manuals located on the eMedNY homepage.
Billing a Referral for a Restricted Recipient
As a result of the NYRx Pharmacy Benefit Transition, pharmacy services (outpatient prescriptions) for MMC enrollees are now being billed through NYRx, the NYS Medicaid Pharmacy Program, on a fee-for-service (FFS) basis. Medical claims for restricted MMC enrollees should follow guidelines established by the MMC Plan of the enrollee. Proper billing procedures for FFS recipients and the NYS Medicaid Pharmacy Program for restricted recipients are explained below.
NYS Medicaid Claims
For NYS Medicaid claims, providers should refer to page 17 of the NYS Medicaid General Billing Guidelines - Professional. Per the New York State Medicaid Companion Guide V 4.0, "when providing services to a member who is restricted to a primary physician or facility, the National Provider Identifier (NPI) of the referring professional must be entered. If a member is restricted to a facility, the NPI of the facility's referring professional must be entered. The identification (ID) of the facility cannot be used."Paper claims submission field location:
Identification Number [Ordering/Referring Provider] (Field 19C)
837P Ref: Loop 2310A NM109
Electronic claims submission field location:
Page Number Loop ID Reference Name Codes Length Comments 292 2110C EB01 Eligibility or Benefit Information N 1 When EB01=N, the patient has provider restrictions for the service type identified in EB03. The provider the patient is restricted to is reported in Loop 2120C. 330 2120C NM101 Entity Identifier Code P3 2 When NM101=P3, the entity being identified is the provider the patient is restricted to for the service type reported in EB03. 333 2120C NM108 Identification Code Qualifier XX 2 NYS Department of Health (DOH) will send "XX" when identifying a Restricted Provider. Pharmacy Claims
For pharmacy claims, providers should refer to page 15 of the eMedNY New York State Billing Guidelines - Pharmacy. Per page 39 of the eMedNY Prospective Drug Utilization Review/Electronic Claims Capture and Adjudication ProDUR/ECCA Provider Manual, "when filling prescriptions/orders for a member who is restricted to a primary provider (physician, clinic, podiatrist, or dentist) and the primary provider is the prescribing/ordering provider, the NPI of this provider must be entered in the ordering/prescribing field."Additionally, "if the restricted member was referred by the primary provider to another provider and the referred-to provider is the prescribing/ordering provider, the pharmacy provider must enter the referred-to provider's NPI in the ordering/prescribing field. The primary provider's NPI must be entered as the referring/primary care provider."
Paper claims submissions field location:
Other Referring/Ordering Provider ID/Licence Number (Field 11A)
Prescriptions for Restricted Members
Name [Other Referring/Ordering Provider] (Field 11B)
Enter the name of the member's primary provider if an NPI has been entered in field 11A.
Electronic claims submission field location:
Primary Care Provider ID Enter the NPI of the primary care provider the NYS Medicaid member is restricted to. 421-DL Primary Care Provider ID Qualifier Enter "01" (NPI). 468-2E Changing Primary Providers
It is the responsibility of the restricted NYS Medicaid member to initiate a relationship with their primary health care providers or pharmacy location. The NYS Medicaid member may request a change of a primary medical care provider or pharmacy location every three months, or at an earlier time for good cause. Provider change requests should be made to the following agencies:
Pharmacy Provider Changes:
- For upstate NYS Medicaid members [all counties outside of New York City (NYC)], providers should contact their LDSS (see the Contact Listing for LDSS By County).
- For New York City (NYC) Medicaid members, providers should contact the NYC Human Resources Administration (HRA) at (888) 692-6116.
- Providers should complete the MAP-3046a form to request a change for a recipient. The MAP-304a form can be found on the Health Commerce System (HCS) website.
- For coverage obtained through the Health Benefit Exchange (HBE), providers should contact HBE by telephone at (855) 355-5777 or (518) 457-0761 (direct line).
NYS Medicaid Provider Changes:
- For upstate NYS Medicaid FFS members, providers should contact their LDSS (see the Contact Listing for LDSS By County).
- For NYC Medicaid FFS members, providers should contact NYC HRA at (888) 692-6116.
- Providers should complete the MAP-3046a form to request a change for a recipient. The MAP-304a form can be found on the HCS website.
- For MMC enrollees (upstate and NYC), providers should contact their MMC Plan.
Questions:
- Questions regarding NYS Medicaid billing or eligibility should be directed to the eMedNY Call Center at (800) 343-9000.
- Questions regarding the Recipient Restriction Program should be directed to the OMIG RRP helpline by telephone at (518) 474-6866 or by email at omig.sm.RRP@omig.ny.gov.
Reminder of the New York State Medicaid Policy for Durable Medical Equipment, Prosthetics, Orthotics, and Supplies for Members in Residing in Nursing Homes
Nursing homes are generally reimbursed by all-inclusive rates for (NYS) Medicaid members. Costs for most Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) are included in these all-inclusive rates paid to the facility. Per Title 18 New York Codes, Rules and Regulations (NYCRR) §505.5(d)(1)(iii), payment will not be made for items provided by a facility or organization when the cost of these items is included in the rate. Generally, DMEPOS providers should not seek NYS Medicaid reimbursement for the costs of these items when the NYS Medicaid member is a resident of a nursing home. There is an exception for custom-made DEMPOS, defined as any durable medical equipment, orthopedic footwear, orthotics, or prosthetics fabricated solely for a particular NYS Medicaid member that cannot be readily changed to conform to the needs of another NYS Medicaid member. Custom-made DEMPOS are not included in a nursing homes rate and DMEPOS providers may seek reimbursement for these items. DMEPOS providers should confirm whether a NYS Medicaid member resides in a nursing home before submitting a claim for reimbursement.
Where the nursing home services are included in the plan benefit package, plans are responsible for educating providers and monitoring claims to eliminate any potential duplicate payments. Providers should ensure the items are not included in the rate of the facility before billing NYS Medicaid fee-for-service (FFS) or the Medicaid Managed Care (MMC) Plan.
Questions:
- FFS questions regarding this policy should be directed to OHIPMEDPA@health.ny.gov.
- MMC questions regarding this policy should be directed to the specific plan of the enrollee. An MMC Plan directory can be found in the eMedNY New York State Information for All Providers - Managed Care Information Information document.
Pharmacy Program Integrity Spotlight
The Pharmacy Program Integrity Spotlight is a regular monthly series intended to reinforce pharmacy program requirements and share program integrity information with providers. Pharmacy providers who service New York State (NYS) Medicaid members must be enrolled in NYS Medicaid and comply with all federal and NYS laws, rules and/or regulations, and must comply with NYS Medicaid rules and policies.
As enrolled providers, pharmacy owners and supervising pharmacists have a corresponding responsibility to ensure:
- recognized standards of pharmacy practice are maintained, and that the pharmacy is always under the immediate supervision of a licensed pharmacist when the pharmacy is operating;
- changes in pharmacy enrollment are reported to the NYS Department of Health (DOH) promptly, including changes in ownership, service location, and supervising pharmacist;
- prescription claims submitted for payment are true, accurate, and for a legitimate medical purpose;
- prescription records related to NYS Medicaid payments are maintained for at least six years including, but not limited to, prescription dispensing logs, inventory records, and patient pick up/delivery records;
- Please note: Providers continue to be subject to any additional record retention requirements outlined in their contracts with Medicaid Managed Care (MMC) or Managed Long Term Care (MLTC) Plans.
- a compliance program, if required, is maintained in accordance with NYS Social Services Law (SOS) §363-d, and Title 18 of the New York Codes, Rules and Regulations (NYCRR) SubPart 521-1, located in the NYS Office of the Medicaid Inspector General (OMIG) Summary of Regulation document; and
- any identified NYS Medicaid overpayments are reported and returned through the OMIG Self-Disclosure Program.
Additional information related to NYRx pharmacy policy and billing guidelines can be found on the eMedNY "Pharmacy Manual" web page. Compliance on the providers part as a NYS Medicaid-enrolled provider ensures NYS Medicaid funds are properly expended and NYS Medicaid members continue to have access to high quality patient care. Providers who suspect that a provider or NYS Medicaid member has committed NYS Medicaid fraud should submit a report by telephone at (877) 87-FRAUD [(877) 873-7283] or through the NYS OMIG "File an Allegation" web page.
Resources:
- NYS OMIG "Provider Resources" web page
- NYS OMIG "Compliance Library" web page
- NYS OMIG "Self-Disclosure" web page
- NYS OMIG "Medicaid Managed Care Fraud, Waste, and Abuse Prevention Programs Guidance and Forms" web page
Questions and Additional Information:
- Additional information related to NYRx pharmacy policy and billing guidelines can be found on the eMedNY "Pharmacy Manual" web page.
- As a NYS Medicaid-enrolled provider, compliance with laws, rules, regulations, and guidance ensures NYS Medicaid funds are properly expended and NYS Medicaid members continue to have access to high quality patient care. All questions regarding compliance program requirements should be directed to the OMIG Bureau of Compliance at compliance@omig.ny.gov.
- For additional information, providers can refer to the NYS OMIG "Compliance" web page.
The Medicaid Update is a monthly publication of the New York State Department of Health.
Kathy Hochul
Governor
State of New YorkJames McDonald, M.D., M.P.H.
Commissioner
New York State Department of HealthAmir Bassiri
Medicaid Director
Office of Health Insurance Programs