October 2008
Volume 24, Number 11
New York State Medicaid Update
The official newsletter of the New York Medicaid Program
David A. Paterson, Governor
State of New York
Richard F. Daines, M.D. Commissioner
New York State Department of Health
Deborah Bachrach, Deputy Commissioner
Office of Health Insurance Programs
Dear Medicaid Provider,

Welcome to the October 2008 edition of the Medicaid Update where it is our goal to keep you apprised of changes in Medicaid policies and procedures.
This month's newsletter includes information on two important initiatives: a smoking cessation counseling program for pregnant women and a diabetes and asthma self-management training program for beneficiaries. Take a peek inside to learn more about these important new initiatives.
We continually look for additional ways to keep you up to date and help make plan administration hassle-free. We value your feedback, please e-mail us at medicaidupdate@health.state.ny.us.
In this issue....

Policy and Billing Guidance
Medicaid to offer smoking cessation counseling for pregnant women
Reimbursement soon available to outpatient hospital clinics and diagnostic treatment centers
Diabetes and Asthma self-management training soon offered to Medicaid beneficiaries.
Important "Never Events" update
Enhanced payment for expanded "after hours" access
Reminder: CBIC card is valid statewide for Medicaid
PHARMACY NEWS
EPIC Update: New York's Prescription Program for Seniors
Medicaid drug rebate program overview
Ordered ambulatory providers billing 340B purchased drugs
Mandatory generic drug program update
Are you new to the Medicaid pharmacy prior authorization (PA) process?
DENTAL PROVIDERS
Dispensing validation system (DVS) updateNEWS FOR ALL PROVIDERS
Clinic Providers Reminder
Don't be silent about smoking
Medicaid training available
Provider Services
PLEASE NOTE: The phone number for the Recipient Name Search/Check Amount inquiry line changed on Tuesday, September 23. The new phone # is (518) 449-0400.
Do you suspect that a Medicaid provider or an enrollee has engaged in fraudulent activities?
Return to Table of Contents
Call: 1-877-87FRAUD
Your call will remain confidential.
You can also complete a Complaint Form online at:
www.omig.state.ny.us
Message from the Editor
Medicaid Update newsletter will move to electronic distribution
Return to Table of Contents
In an effort to distribute the Medicaid Update in a more efficient manner, reduce costs, and be more environmentally minded, beginning January 2009, the Office of Health Insurance Programs will no longer produce a printed version of the newsletter.
The Medicaid Update will ONLY be available electronically. This new delivery system will allow our providers to receive policy sensitive bulletins faster. The newsletter will be delivered monthly to your designated e-mail address in a Portable Document Format (PDF).
To receive the Medicaid Update electronically, please send your e-mail address with your provider ID# by Monday, November 10, 2008 to the following e-mail: medicaidupdate@health.state.ny.us.
Providers who are unsure about receiving an electronic-only version of the newsletter should bear in mind that the PDF newsletter can always be printed and read in hard copy.
Additionally, the current and archived newsletters are posted on the DOH Website at the following address: http://www.nyhealth.gov/health_care/medicaid/program/update/main.htm
You will receive your final printed newsletter by mail in December 2008 as we transition from print newsletters to electronic distribution.
The Office of Health Insurance Programs anticipates that most providers will take advantage of this new delivery system, however, those who cannot may send a written request, along with your provider ID#, to the following address by Monday, November 10, 2008 to:
NYS Department of Health
Office of Health Insurance Programs
Attention: Kelli Kudlack
Corning Tower, Room 2029
Albany, New York 12237
Don't be left out...send us your e-mail address and provider # today!
Forms available online
Return to Table of Contents
The Sterilization Consent form and the Acknowledgement of Hysterectomy Information form can be accessed on the Department of Health Website at the following link: http://www.health.state.ny.us/health_care/medicaid/publications/docs/ldss/ldss-3134.pdf
Questions? Call 518-473-2160.
Policy and Billing Guidance
Medicaid to offer smoking cessation counseling for pregnant women
Return to Table of Contents
In support of the United States Department of Health and Human Services Clinical Practice Guidelines 2008 Update "Treating Tobacco Use and Dependence," NYS Medicaid will soon cover smoking cessation counseling to pregnant women.

Effective January 1, 2009, Medicaid will reimburse office based providers and hospital outpatient departments for smoking cessation counseling. Reimbursement for these services will be available to free-standing diagnostic and treatment centers effective March 1, 2009. This counseling will complement existing Medicaid covered benefits for smoking cessation coverage, which include prescription and nonprescription smoking cessation products. Note: A Federally Qualified Health Center (FQHC) may bill for this service ONLY if it has elected to be reimbursed under Ambulatory Patient Groups (APGs).
Medicaid managed care and Family Health Plus plans will also be responsible for covering smoking cessation counseling services for pregnant women effective January 1, 2009. Coverage includes up to six counseling sessions within any 12 month period.
Reimbursement for smoking cessation counseling (SCC) must meet the following criteria:
- Services must be provided face-to-face.
- Services are ONLY available for Medicaid-eligible pregnant females who smoke. The claim must include a diagnosis of pregnancy (ICD-9-CM Diagnosis Codes: 630-677, V22, V23, V28).
- Smoking cessation counseling must be provided by a physician, registered physician's assistant, registered nurse practitioner, or licensed midwife during a medical visit (no group sessions).
- Physicians, nurse practitioners, licensed midwives, hospital outpatient departments, and freestanding diagnostic and treatment centers will be allowed to bill for SCC.
- Smoking cessation counseling is payable in a clinic setting with a diagnosis of pregnancy, an E&M code, and a SCC CPT procedure code.
- Smoking cessation counseling is payable in an office setting when billed with a diagnosis of pregnancy and the appropriate SCC CPT procedure code.
- Pregnant women will be allowed up to 6 counseling sessions within a continuous 12 month period.
- Office based providers will bill CPT procedure codes as follows:
- 99406 - Smoking cessation counseling 3 to 10 minutes.
- 99407 - Smoking cessation counseling greater than 10 minutes.
- Clinics will bill smoking cessation counseling utilizing these CPT codes which will group to APG 451.
- Practitioners will also bill smoking cessation counseling using the above referenced CPT codes. Payment amounts will be published shortly in updated practitioner fee schedules, which are available online at http://www.emedny.org
Questions? Please contact the Bureau of Policy Development and Coverage at (518) 473-2160
Policy and Billing Guidance

- LICENSED CLINICAL SOCIAL WORKERS (LCSWS)
- LICENSED MASTER SOCIAL WORKERS (LMSWS)
Reimbursement soon available to outpatient hospital clinics and free standing diagnostic and treatment centers
Return to Table of Contents
Effective January 1, 2009, reimbursement will be available to Article 28 outpatient hospital clinics and freestanding diagnostic and treatment centers for mental health counseling provided by Licensed Clinical Social Workers (LCSWs) and Licensed Master Social Workers (LMSWs).
Reimbursement will be available only for mental health counseling services provided to children and adolescents under the age of 19 and for pregnant women up to 60 days post-partum (based on the date of delivery or end of pregnancy). Mental health counseling by a psychiatrist or psychologist is still available to all Medicaid enrollees.
Clinics may bill Medicaid or a Medicaid managed care or Family Health Plus plan, as appropriate, for these services.
Reimbursement Requirements:
- A facility that is offering mental health counseling by LCSWs and LMSWs must have the appropriate certification listed on its operating certificate.
- All enrollees who are under age 19 are eligible for mental health services.
- Pregnant women are eligible for mental health services. They must have a primary or secondary diagnosis of pregnancy (ICD-9 codes: 630-677, V22, V23, and V28). Mental health services are also available up to 60 days postpartum with a primary or secondary diagnosis of postpartum depression (ICD-9 codes 648.40 - 648.44).
Three new rate codes have been established for billing mental health services in outpatient hospital clinics and free-standing diagnostic and treatment centers:
- 4257 Individual Brief Counseling (psychotherapy which is insight oriented, behavior modifying and/or supportive, approximately 20-30 minutes face-to-face with the patient).
- 4258 Individual Comprehensive Counseling (psychotherapy which is insight oriented, behavior modifying and/or supportive, approximately 45-50 minutes face-to-face with patient).
- 4259 Family Counseling (psychotherapy with or without patient).
The Profession Codes required for billing are:
- LCSW (Licensed Clinical Social Worker): Profession Code 073.
- LMSW (Licensed Master Social Worker): Profession Code 072.
In addition to the mental health counseling services described above, Article 28 certified free-standing diagnostic and treatment centers that billed and received Medicaid payment for individual psychotherapy services provided by licensed social workers in calendar year 2007 may continue to bill Medicaid for such services. Mental Health counseling provided by such clinics is available to all eligible Medicaid enrollees regardless of age or pregnancy status.
Questions? Please contact the Bureau of Policy Development and Coverage at (518) 473-2160
Policy and Billing Guidance
Diabetes and Asthma self-management training will soon be offered to Medicaid beneficiaries
Return to Table of Contents
NYS Medicaid will cover diabetes and asthma self management training services (DSMT and ASMT, respectively) for Medicaid beneficiaries diagnosed with diabetes or asthma when such services are ordered by a physician, registered physician's assistant (PA), registered nurse practitioner (RNP), or a licensed midwife (LM). This change will become effective in physicians' offices and hospital outpatient departments (OPDs) on January 1, 2009, and in free-standing diagnostic and treatment centers (D&TCs) on March 1, 2009. A Federally Qualified Health Center (FQHC) may bill for this service ONLY if it has elected to be reimbursed under Ambulatory Patient Groups (APGs).
Self-management training services are to be provided by a New York State licensed, registered, or certified health care professional, who is also certified as an educator by the National Asthma Educator Certification Board (CAE) or the National Certification Board for Diabetes Educators (CDE). Educators in this program are expected to practice within the scope of practice that is appropriate to their respective discipline, as defined by the Office of the Professions, NY State Education Department. Self-management training services will be billed by physicians, RNPs, LMs, OPDs, D&TCs and Federally Qualified Health Centers (FQHCs) who employ (or contract with) certified educators. Physicians and RNPs who are certified educators, themselves, can also bill for these services.
To enhance patient access, offices or clinics that do not directly offer ASMT or DSMT services may refer patients in need of educational services to Medicaid enrolled practitioner offices or clinics that do employ or contract with certified asthma and/or diabetes educators. A referral for ASMT or DSMT services must be written by the referring clinician (physician, PA, RNP or LM).
In the event that a Medicaid beneficiary is referred for ASMT or DSMT services, it is expected that appropriate documentation and feedback regarding the self management training will be communicated to the referring clinician.
A beneficiary with newly diagnosed asthma or diabetes, or a beneficiary with asthma or diabetes who has a medically complex condition - such as an exacerbation or poor control of the asthma or diabetes, a diagnosis of a complication, a diagnosis of a co-morbidity, a recent surgical procedure, a prescription for new asthma- or diabetes-related medications or equipment, a diagnosis of a mental health condition, a learning disability, and/or an unstable medical condition will be allowed up to 10 hours of self-management training for each condition during a continuous 6-month period.
The following professional entities (who are New York State licensed, registered, or certified, and are Certified Educators in their respective disciplines) may provide Medicaid self-management training services:
ASTHMA
- Registered Nurse
- Registered Nurse Practitioner
- Respiratory Therapist
- Physician (MD, DO)
- Pharmacist
- Physician Assistant
DIABETES
- Registered Nurse
- Registered Nurse Practitioner
- Registered Dietician
- Physician (MD, DO)
- Pharmacist
- Physician Assistant
- Physical Therapist
Enrollment and billing for ASMT and DSMT - How will it work?
CAEs and CDEs who cannot bill Medicaid directly will enroll as non-billing Medicaid providers and must be employed by or contracted with a billing Medicaid provider. At the time of enrollment, CAEs and CDEs must submit a copy of their professional license, certification, or registration from the New York State Education Department, and their national educator board certification to the Department of Health, Office of Health Insurance Programs, Division of Provider Relations and Utilization Management.
As part of the enrollment process, the entity with whom the educator is employed or contracted must provide proof of employment or a copy of the contract with the certified educator. Providers will be notified in a future edition of the Medicaid Update when enrollment forms and instructions become available.
When a practitioner does not directly offer ASMT or DSMT services, they may refer patients in need of educational services to Medicaid-enrolled practitioner offices or clinics that do employ or contract with CAEs and/or CDEs. Medicaid-enrolled clinics that employ or contract with CAEs and/or CDEs, and render educational services to a nonregistered clinic patient, will be reimbursed according to the ordered ambulatory fee schedule.
For a definition of 'ordered ambulatory services,' please refer to the online Clinical Provider Manual, policy section, page 8, or copy and paste the following link into your web browser: http://www.emedny.org/ProviderManuals/Clinic/PDFS/Clinic_Policy_Guidelines.pdf
Claims submitted for ASMT must have a diagnosis of Asthma (ICD-9 493.XX), and claims submitted for DSMT must have a diagnosis of Diabetes (ICD-9250.XX, 648.0x, 648.8x, 775.0, or 775.1).
If the beneficiary with diabetes or asthma is a child under 18 years of age, the parent(s) or legal guardian(s) may attend the education session and the claim will be submitted under the child's Medicaid number.
In an office setting, when billing for ASMT or DSMT, the provider must submit an individual claim for educational services, and the National Provider Identifier (NPI) of the CAE/CDE must be reported in the service provider field on the claim form.
In a clinic setting, since only one claim can be submitted per day, if multiple services are provided by different providers on a given day (e.g., an E&M service followed by diabetes self-management training), then only the NPI of the major service provider for that day should be entered on the claim form.
Asthma Self-Management Training (ASMT)
- A beneficiary with newly diagnosed asthma or a beneficiary with asthma who has a medically complex condition (such as: an exacerbation of asthma, poor asthma control, diagnosis of a complication, etc.) will be allowed up to 10 hours of ASMT during a continuous 6-month period.
- Beneficiaries with asthma who are medically stable may receive up to 1 hour of ASMT in a continuous 6-month period.
- Self-management training services may be provided in individual sessions, or in group sessions of no more than eight patients.

Asthma Self-Management Training CPT Codes
- 98960 - Individual education for 30 minutes.
- 98961 - Group education, for a 30 minute session, 2-4 patients
- 98962 - Group education, for a 30 minute session, 5-8 patients
Diabetes Self-Management Training (DSMT)
- A beneficiary with newly diagnosed diabetes or a beneficiary with diabetes who has a medically complex condition (such as: poor diabetes control [A1c>8], diagnosis of a complication, diagnosis of a co-morbidity, post-surgery, prescription for new equipment such as an insulin pump, etc.) will be allowed up to 10 hours of DSMT during a continuous 6-month period.
- Beneficiaries with diabetes who are medically stable may receive up to 1 hour of DSMT in a continuous 6-month period.
- Self-management training services can be provided in individual sessions, or in group sessions of no more than eight patients.
Diabetes Self-Management Training HCPCS Codes
- G0108 - Diabetes outpatient self-management training services, individual, per 30 minutes.
- G0109 - Diabetes outpatient self management training services, group (2-8 patients), per 30 minutes
Fee schedules for these services will be published in January 2009.
Please note that physicians and RNPs may also provide diabetes and asthma education in the context of an E&M service, regardless of whether or not the clinician has a CDE or CAE. In this instance, the educational service can be reflected in the calculation of the level of the E&M code.
However, a physician or RNP who accounts for the educational service in the E&M code is not permitted to additionally bill one of the specific codes noted above for the same education service.
Billing Examples:
| ICD-9 Diagnosis Code | 493.XX Asthma |
| CPT Procedure Code | 98960 ASMT |
| Billable Units | (one unit = a 30 minute session) (Can bill multiple units per day, based on medical necessity). |
| Service Provider | NPI number of the CAE |
| Please note: Providers billing on paper claim forms must submit an individual claim for educational services and include the above billing parameters. Providers that bill electronically can enter all services rendered on a single transaction, with the service provider data indicated at the service line level. | |
| ICD-9 Diagnosis | 250.XX Diabetes |
| HCPCS Procedure | G0108 DSMT (Can bill multiple units per day, based on medical necessity). |
| Service Provider | NPI number of the CDE |
| ICD-9 Diagnosis | 493.XX Asthma |
| Procedures | 99213 E&M |
| 98960 ASMT (Can bill multiple units per day, based on medical necessity). | |
| Service Provider | NPI number of the major service provider. |
NOTES:
Facilities with APG reimbursement will be able to bill the same self-management training procedure code multiple times, depending on how many 30 minute sessions are provided for a given beneficiary on a given date of service. Reimbursement will be at 100% for the first procedure code, and at 50% for subsequent procedure codes.
Federally Qualified Health Centers (FQHCs) who opt to keep their threshold PPS rate will be reimbursed at that rate regardless of how many self-management sessions are provided on a given date of service.
Policy and Billing Guidance
Important 'Never Events' Update:
Return to Table of Contents

Please Note: A letter was recently mailed out to Administrators from the NYS Department of Health alerting them of a modification to the implementation timeline for Medicaid's payment policy of 14 (fourteen) 'Never Events' (including hospital acquired complications).
Please read important information concerning this new reimbursement policy below:
Effective October 1, 2008, Medicaid will deny or reduce payment for three (3) 'Never Events' (object left in after surgery, air embolism, and blood incompatibility).
This new reimbursement policy applies to discharges on or after October 1, 2008. The New York State Department of Health will suppress the ICD-9 codes relating to these events and make use of the 'Present on Admission' indicator to adjust reimbursement accordingly.
To prevent billing Medicaid for charges that may result from the suppression of these diagnosis codes, hospitals are instructed not to bill for day or high cost outlier payments which are a result of, or significantly associated with, the three (3) events mentioned above. Implementation of payment reductions for the additional eleven (11) events will be deferred until the Department has established one or more specific rate codes, which will be applied by hospitals to all claims (including day or cost outliers) in which one of these eleven events occurred. The Department will then "pend" claims and review for appropriate payment modifications or adjustments.
The Department will provide hospitals with specifics regarding application of the rate code or codes and reimbursement guidelines well in advance of implementation. It is expected that implementation for the eleven (11) events will take place in early 2009.
Questions? Please contact John Franklin at (518) 473-8822 or Dr. Foster Gesten at (518) 486-6865.
Policy and Billing Guidance
Enhanced payment for expanded 'after hours' access
Return to Table of Contents
A supplemental payment amount will be made for ambulatory care scheduled to occur on evenings, weekends and holidays as defined by the Department of Health.
This change will become effective for patient visits in physician offices and hospital outpatient clinics for services provided on or after January 1, 2009.
Patient visits in diagnostic and treatment centers will be eligible for this additional reimbursement for services provided on or after March 1, 2009. This payment will be added to the otherwise applicable payment amount for each such visit. NOTE: A Federally Qualified Health Center (FQHC) may bill for this service ONLY if it has elected to be reimbursed under Ambulatory Patient Groups (APGs).
Payment amounts will be published shortly in updated practitioner fee schedules, which are available online at http://www.emedny.org
Clinic reimbursement for expanded hours access will be incorporated into the facility's APG payment.
For purposes of receiving the enhanced fee, evenings, weekends, and holidays are defined as follows:
- An evening visit is one which is scheduled for and occurs after 6:00 p.m.
- A weekend visit is one which is scheduled for and occurs on Saturday or Sunday.
- A holiday visit is one which is scheduled for and occurs on a designated national holiday.
Providers should use the following CPT codes as appropriate when billing for the expanded 'after hours' supplemental APG payment:
- CPT 99050, Services provided in the office at times other than regularly scheduled office hours, or days when the office is normally closed (e.g., holidays, Saturday or Sunday), in addition to basic service.
- CPT 99051, Services provided in the office during regularly scheduled evening, weekend, or holiday office hours, in addition to basic service.
PLEASE NOTE:
- The CPT codes listed above are not payable if they are the only CPT procedure(s) listed on the claim.
- The CPT codes listed above can be billed only when accompanied by a valid CPT code that represents a medical service/procedure.
Questions? Please contact the Bureau of Policy Development and Coverage at (518) 473-2160.
CBIC card is valid statewide for Medicaid
Reminder for Upstate and New York City health care providers
Return to Table of Contents
Since Medicaid is a statewide program, the Common Benefit Identification Card (CBIC) can be used by a Medicaid eligible individual in any county in New York State. Providers are reminded that a CBIC card must be accepted regardless of whether the Client Identification Number (CIN) appearing on it is an upstate or New York City CIN.
This reminder supports the Department's efforts to ensure that New York State Medicaid recipients who relocate intrastate have access to services. This includes formerly incarcerated individuals whose Medicaid is reinstated following suspension.
Pharmacy News
EPIC UPDATE
New York's Prescription Program For Seniors
Return to Table of Contents

Mandatory Generic Program
Effective October 1, 2008, EPIC requires the substitution of brand-name multi-source drugs with the generic equivalent on prescriptions where EPIC is the primary payer. A brand-name multi-source drug will only be covered if the prescriber obtains a prior authorization from EPIC.
Pharmacists may obtain a prior authorization when a generic is unavailable in the marketplace or when a 72-hour emergency supply is necessary because the prescriber cannot be reached.
To obtain a prior authorization, prescribers and pharmacists must call the EPIC Prior Authorization Call Line at (800) 256-2082.
Coordination with Medicare Part D
Before billing EPIC for a drug not covered by a Part D plan, pharmacists must consult with the prescriber about a possible substitute on the primary plan formulary. If the prescriber does not authorize an alternative, the pharmacy should document the consultation in their records and bill EPIC for the drug.
When billing EPIC, the pharmacy must certify that the prescriber was consulted by including a Submission Clarification Code (SCC) of 7 (prescriber determined medically necessary). If the prescriber could not be reached, EPIC can be billed with a SCC of 99 (other) to certify a consultation was attempted; however, the prescriber needs to be consulted before the next refill.
Exceptions: Drugs that are excluded from Medicare Part D (e.g. Benzodiazepines and Barbiturates) will not be subjected to this new requirement.
Part D Appeals
When cost effective, EPIC will submit appeals to Part D plans on behalf of enrollees for drugs not covered. Prescribers will be asked to complete the clinical portion of the required form, which EPIC will then submit to the Part D plan for consideration.
Please note: Prescriber and pharmacist cooperation is greatly appreciated, as these initiatives are important measures that will enable New York State to continue to help EPIC seniors afford the medications they need.
If you know a senior who needs help paying for out-of-pocket drug costs (deductibles, co-payments, non-covered drug costs or during the Medicare coverage gap) please refer them to EPIC.
EPIC HELPLINE (800)332-3742
Pharmacy News
Medicaid drug rebate program
Physicians, Nurse Practitioners, Licensed Midwives, and Ordered Ambulatory Providers
Return to Table of Contents

The 2005 Federal Deficit Reduction Act (DRA) requires Medicaid providers to report the National Drug Code (NDC) when billing for physician administered (J-code) drugs in addition to using the HCPCS code. The NDC quantity and NDC unit of measure must also be included on the claim.
The Federal Rebate Program also requires that Medicaid reimbursement be limited to drugs for which drug manufacturers have a signed rebate agreement with the Centers for Medicare and Medicaid Services (CMS). Approximately 520 pharmaceutical companies participate in the drug rebate program.
To assure compliance with this requirement, effective November 2, 2008, Medicaid providers must verify that the manufacturer has a signed rebate agreement prior to billing Medicaid by following these steps:
- Locate the drug's NDC information, which can be obtained from the drug invoice and/or drug packaging information. Note the first five digits of the NDC, which represents the manufacturer/labeler code.
- Check this five-digit code against the labeler code contained on the list of drug manufacturers/labelers that currently participate in the drug rebate program, found at the following link: http://www.cms.hhs.gov/MedicaidDrugRebateProgram/10_DrugComContactInfo.asp
- The labeler code is the five digit number at the beginning of the list, and precedes the name of the company.
- If the five-digit labeler code from the drug's NDC is a match for any of the labeler codes on the list from the Website, then the manufacturer has a signed rebate agreement with Medicaid, and the drug can be billed.
- If a drug is billed to Medicaid when the manufacturer is not a rebate signer, the claim will be denied.
Questions can be directed to the Bureau of Pharmacy Policy and Operations at (518) 486-3209.
Ordered ambulatory providers billing 340B purchased drugs
Return to Table of Contents
Effective November 2, 2008, ordered ambulatory providers billing Medicaid for drugs purchased through the 340B program will be able to identify their drug claims as a 340B priced claim as follows:
- Use the product service qualifier-loop 2400, SV2 segment, data element SV202-3 through SV202-6 on the 837I electronic format and enter the value of UD in this field.
When using this option, the drug must have been purchased through the 340B program and billed to Medicaid at the 340B price. When billing in this manner, it is not necessary to enter the NDC code or NDC units on the claim.
For pharmacy billing questions, please call (800) 343-9000
For Medicaid pharmacy policy questions, please call (518) 486-3209
Pharmacy News
Mandatory generic drug program update
Return to Table of Contents
The New York State Medicaid Mandatory Generic Drug Program requires prior authorization for brand-name prescriptions with an A-rated generic equivalent.
Effective November 1, 2008, new prescriptions for the brand-name drugs listed below will require prior authorization.
| Anestacon 2% Jel | Mononessa 28 Tablet |
| Beta-Val 0.1% Cream | Naprelan 500MG SA Tablet |
| Brevicon 28 Tablet | Necon 7-7-7 28 Tablet |
| Camptosar 20MG/ML Vial | Nora-Be Tablet |
| Cipro I.V. 10 MG/ML Vial | Nor-QD Tablet |
| Cipro I.V. 200 MG & 400 MG/100ML D5W | Omnipred 1% Eye Drop |
| Claforan 2 GM Injection | Reglan 5MG/5ML Vial |
| Climara 0.0375 & 0.06 MG/Day Patch | Serophene 50 MG Tablet |
| Diprivan 10MG/ML Vial | Solia Tablet |
| Emla Cream | SSD 1% Cream |
| Jolivette Tablet | Trinessa Tablet |
| Kytril 1MG/ML Vial | Thermazene 1% Cream |
| Maxipime 1 & 2 Gram Vial | Unasyn 15 Gram Vial |
| Metro I.V. 500MG/100ML | Zithromax I.V. 500 MG Vial |
Prescriptions written prior to November 1, 2008, but filled on or after that date, including refills, will not require prior authorization. However, when the current prescription expires, a prior authorization will be required for the patient to continue to receive the brand-name drug.
PLEASE NOTE: Brand-name drugs that are on the Medicaid Preferred Drug List do not require prior authorization and are not subject to the Medicaid Mandatory Generic Program prior authorization requirements.

Are you new to the Medicaid Pharmacy Prior Authorization (PA) process or just looking for more information?
Return to Table of Contents
If so, we have developed materials just for you. Our Medicaid Pharmacy Prior Authorization Process Flowchart (PA Flowchart) walks you step by step through the process of obtaining a prior authorization. To access the PA Flowchart go to: https://newyork.fhsc.com/downloads/providers/NYRx_PA_process_flowchart.pdf or follow these easy steps:
- Visit our Website at https://newyork.fhsc.com
- Click on "Providers"
- Click on "Prior Authorization Programs" then "Forms and Worksheets"
- Click on the link for "Medicaid Pharmacy Prior Authorization Process"
Don't forget to print the most current Preferred Drug List (PDL) at the following Website address https://newyork.fhsc.com/downloads/providers/NYRx_PDP_PDL.pdf or you can save time by sending a request to NYPDPNotices@firsthealth.com and you will automatically receive a PDL when updates are made to the program!
Provider News
Dental Providers
Dispensing validation system (DVS) update
Return to Table of Contents

Implementation of the "Dispensing Validation System (DVS)" for Dental Sealants (D1351) and Full Dentures (D5110 and D5120) began August 1, 2008. The implementation has proven successful and many providers find it to be a very useful and time saving feature.
DVS HELPFUL TIPS:
- If a request is submitted through DVS and rejected, it does NOT mean that the requested procedure has been denied. A prior approval request can still be submitted either on an eMedNY prior approval request form 361401 or by a HIPAA compliant 278 transaction (e.g. ePACES), for professional review and determination. Charting, x-rays and documentation of necessity should be submitted as appropriate for the procedure(s) being requested. X-rays are not required for sealants if there is no other procedure being requested which would require x-rays.
- DVS authorization or prior approval does NOT guarantee payment. The same conditions apply when claims are submitted for payment regardless of prior authorization / approval:
- The client must be eligible on the date that the service is provided or on the date of the "decisive appointment;"
- Sealants (D1351) are only permitted on permanent first and second molars between the ages of 5 and 15 (inclusive);
- Any conflicting claims payment history will "pend" or "deny" the claim;
- If there is a claims payment history for sealant (D1351) to the same provider or group within the allowed service frequency (3 years), payment will automatically be denied.
DVS submission is the fastest and easiest way to submit requests and is highly recommended.
For DVS technical assistance or to obtain eMedNY prior approval request form 361401, please contact Computer Sciences Corporation (CSC) at (800) 343-9000.
Questions? Please contact the Division of Provider Relations and Utilization Management, Dental Bureau at (800) 342-3005 menu option #2.
Clinic Providers
REMINDER
Return to Table of Contents
Medicaid does not pay for outpatient and ambulatory services while a patient is hospitalized.
Effective October 30, 2008, clinic claims submitted for a period when a patient is hospitalized will be denied when the clinic services are covered under the inpatient rate. Providers will receive an error message for Edit 00760 (Suspect Duplicate, covered by Inpatient Claim). Clinic providers should contact the eMedNY Call Center with any questions at (800) 343-9000.
Provider News
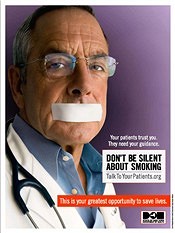
Smoking Cessation Medication Coverage Policy for Medicaid
Return to Table of Contents
- Smoking cessation therapy consists of prescription and non-prescription agents. Covered agents include nasal sprays, inhalers, Zyban (bupropion), Chantix (varenicline), over-the-counter nicotine patches and gum.
- Two courses of smoking cessation therapy per enrollee, per year are allowed. A course of therapy is defined as no more than a 90-day supply (an original order and two refills, even if less than a 30 day supply is dispensed in any fill).
- For all smoking cessation products, the enrollee must have an order. A prescription is the terminology for an order of a prescription product. A fiscal order refers to an order, which looks just like a prescription-written on a prescription blank, for an over-the-counter product.
Questions? Contact the Medicaid Pharmacy Policy and Operations staff at (518) 486-3209
By providing counseling, pharmacotherapy, and referrals, you can double your patients' chances of successfully quitting.
For more information, visit http://www.talktoyourpatients.org or call the NY State Smokers' Quitline at 1-866-NY-QUITS (1-866-697-8487).
Provider News
Computer Sciences Corporation offers Medicaid seminars
Return to Table of Contents

- Do you have billing questions?
- Are you new to Medicaid billing?
- Would you like to learn more about ePACES?
If you answered YES to any of these questions, please consider registering for a Medicaid seminar. Computer Sciences Corporation (CSC) offers various seminars to providers and their billing staff. Many of the seminars planned for the upcoming months offer detailed information and instruction about Medicaid's web-based billing and transaction program - ePACES.
ePACES is the electronic Provider Assisted Claim Entry System which allows enrolled providers to submit the following type of transactions:
- Claims
- Eligibility Verifications
- Utilization Threshold Service Authorizations
- Claim Status Requests
- Prior Approval Requests
Professional providers such as physicians, nurse practitioners and private duty nurses can even submit claims in "REAL-TIME" via ePACES. Real-time means that the claim is processed within seconds and professional providers can get the status of a real-time claim, including the paid amount without waiting for the remittance advice.
Fast and easy seminar registration, locations and dates are available online at http://www.emedny.org/training/index.aspx.
Review the seminar descriptions carefully to identify the seminar appropriate for you. Registration confirmation will be instantly sent to your e-mail address.
If you are unable to access the Internet to register, you may request a list of seminars and registration information be faxed to you through CSC's Fax on Demand at (800) 370-5809. Please request document 1003 for October-December seminar dates.
CSC Regional Representatives look forward to meeting with you at upcoming seminars!
Questions about registration? Please contact the eMedNY Call Center at (800) 343-9000.

PROVIDER SERVICES
Return to Table of Contents
Missing Issues?
The Medicaid Update, indexed by subject area, can be accessed online at:
http://www.nyhealth.gov/health_care/medicaid/program/update/main.htm
Office of the Medicaid Inspector General: http://www.omig.state.ny.us (518) 473-3782
Questions about an Article?
Each article contains a contact number for further information, questions or comments.
Questions about billing and performing EMEVS transactions?
Please contact eMedNY Call Center at: (800) 343-9000.
Provider Training
To sign up for a provider seminar in your area, please enroll online at:
http://www.emedny.org/training/index.aspx
For individual training requests, call (800) 343-9000 or email: emednyproviderrelations@csc.com
Enrollee Eligibility
Call the Touchtone Telephone Verification System at any of the numbers below:
(800) 997-1111 (800) 225-3040 (800) 394-1234.
Address Change?
Questions should be directed to the eMedNY Call Center at: (800) 343-9000.
Fee-for-Service Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Rate-Based/Institutional Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Comments and Suggestions Regarding This Publication?
Please contact the editor, Kelli Kudlack, at:
medicaidupdate@health.state.ny.us
Medicaid Update is a monthly publication of the New York State Department of Health containing information regarding the care of those enrolled in the Medicaid Program.