New York State
June 2007
Volume 23, Number 6
Medicaid Update
The official newsletter of the New York Medicaid Program
Eliot Spitzer, Governor
State of New York
Richard F. Daines, M.D. Commissioner
New York State Department of Health
Deborah Bachrach, Deputy Commissioner
Office of Health Insurance Programs
News for All Providers
Restricted Recipient Program Information
Identifies medical and non-medical reasons why an enrollee may be restricted under the NYS Medicaid Program.
Disqualified Provider List
If you want to know if a potential employee has ever been disqualified from the Medicaid Program, then read this article!
Are You Receiving Medicaid Correspondence at the Appropriate Address?
Providers must notify the Medicaid Program of any change of address in order to receive important Medicaid information.
Seminar Schedule and Registration
If you have billing questions or want to learn more about ePACES, read this article to find out where to sign up for training seminars!
Individual Provider Training is Available
Computer Sciences Corporation offers billing training to individual providers. Here's how to sign up!
Claims Pended for Review by the Office of the State Comptroller
Clarifies a new edit that some providers may see on denied or pended claims.
Submission of Medicaid Claims Over Two Years Old
Reminds providers of when it is appropriate to submit a claim over two years from the date of service.
Accessing the Medicaid Eligibility Verification System
ePACES provides quick responses for certain requests, such as eligibility and utilization thresholds. Sign up today!
Policy and Billing Guidance
Preferred Drug Program
Is your patient subject to the Preferred Drug Program? Is the drug you are prescribing preferred or non-preferred? This article contains the answer to these questions and more!
Reimbursement Changes for Pharmacy Claims.
Effective July 1, 2007, there will be changes to the estimated acquisition cost for drugs.
Pharmacists Must Bill Medicare First
A reminder to pharmacy providers to bill Medicare first when an enrollee has dual coverage.
Physicians Billing for Critical Care
What is critical care and how is it billed to the Medicaid Program?
National Drug Code Required on Medicaid Claims
A notice to Physicians, Nurse Practitioners, Licensed Midwives and Article 28-Based Hospitals and Clinics that the Medicaid Program will collect this information on claims.
Reviewing Your Transportation Rosters
Practitioners who order transportation services are reminded to review their Ordering Practitioner Roster for errors.
Medicaid Reimbursement for Implanon
Introducing coding instructions for the billing of the Medicaid Program for the contraceptive Implanon.
Durable Medical Equipment Fee Schedule Changes
Effective for dates of service on or after May 1, 2007, fees for certain items of Durable Medical Equipment have changed.
General Information
Antibiotic Resistance and the Judicious Use of Antibiotics
Prescribers are asked to use antibiotics judiciously to prevent the spread of resistance!
Tick-Tock: Information About Deer Ticks
Information for Medicaid enrollees! It's that time of year when ticks come alive! Learn how to identify and remove a deer tick.
Using the eMedNY 361501 Prior Approval Request Form
Clarification on a form used by Pharmacy, Durable Medical Equipment, Nursing, Eye Care and Physician Services providers.
Managing the Costs of Arthritis and Other Chronic Diseases
The Department's Arthritis Program discusses the costs of the leading cause of disability in the United States.
Save the Date: "Planning Today for Tomorrow"
Announcing a symposium offered on June 21, 2007 where attendees can discuss Long Term Care restructuring activities and discuss plans for the future of Long Term Care in New York State.
Restricted Recipient Program Information
Return to Table of Contents
The Restricted Recipient Program (RRP) identifies Medicaid enrollees that have abused or misused medical services. Medical reviews are performed by the State Medical Review Team (SMRT), which include pharmacists, nurses, and a physician consultant. There are also non-medical reasons to restrict enrollees that may include:
- forged prescriptions,
- card loaning,
- possession of multiple identification cards,
- selling of drugs obtained through Medicaid.
The program is administered by both the State and local departments of social services. The local departments work directly with enrollees and providers to establish primary care assignments, develop a case management plan, resolve program issues, and maintain the RRP data system. The objectives of the program are to establish enrollees with primary care providers to coordinate medical services, improve quality of care and to reduce overall health care costs.
Facts and Information
- The main primary care provider restrictions are physician/clinic, pharmacy, and inpatient hospital. Enrollees may also be restricted to dentists and durable medical equipment dealers. In the near future, enrollees may also be restricted to physician groups, nurse practitioners, dental clinics, and alternative pharmacies.
- Physician/clinic primary care providers provide all care within their scope of practice.
- Physician/clinic primary care providers are responsible for referring enrollees to all specialty medical services.
- All non-emergency Medicaid transportation services must be ordered by the primary care physician/clinic.
- A primary pharmacy is the sole provider of all prescriptions for RRP enrollees. Primary care physician/clinic providers, as well as specialty medical providers, may write prescriptions. The primary pharmacy must include the primary physician/clinic providers Medicaid Provider Identification Number in the Referring Provider field (NCPDP 421-DL) for all pharmacy claim submissions written by specialty providers. If the prescription is written by a physician in a clinic setting, the physician's license number or Medicaid Provider Identification Number must be entered in the Ordering Provider field (NCPDP 411-DB).
- When there is a non-emergency admission to an inpatient hospital, nursing home, adult home or drug/alcohol rehabilitation service facility, it is the responsibility of the facility where the enrollee is admitted to inform the enrollee's primary physician/clinic and the local district RRP Coordinator of the admission. After a review of the admission by the local district, it may be necessary to change the enrollee's primary medical providers. This is especially important for pharmacy services since many facilities contract with local pharmacies or pharmacy benefit managers. Claims for primary services will be denied if appropriate changes are not made by the local district.
For inquiries regarding NYC RRP enrollees, please call one of the numbers listed below:
(212) 630-1081
(212) 630-1087
(212) 630-1089
For inquiries regarding Upstate RRP enrollees, please call the Local Department of Social Services where the enrollee's Medicaid case is established.
For State RRP policy questions please call:
(518) 474-6866.
Disqualified Provider List
Do Not Hire!
Return to Table of Contents

It is important for all employers and individuals conducting business with the New York State Medicaid program to examine the list of Providers Not Allowed To Order before hiring an individual.
The New York State Department of Health's Providers Not Allowed To Order list includes:
- previously enrolled Medicaid providers who have been disqualified from the Medicaid program for various reasons; and
- individual providers who have never been enrolled in the Medicaid Program, but have been disqualified from the Medicare Program and therefore are not allowed to enroll in the New York State Medicaid Program.
The Providers Not Allowed to Order list can be found online at:
http://nyhealth.gov/health_care/medicaid/fraud/index.htm
The Department of Health encourages those doing business with the Medicaid program to examine this list to ensure compliance and avoid potential administrative sanctions and denied claims.
Are You Receiving Medicaid Correspondence At The Appropriate Address?
Return to Table of Contents
Providers are responsible for notifying Medicaid of any change of address, telephone number or other pertinent information within 15 days of a change.
New York State Medicaid and the eMedNY fiscal agent, Computer Sciences Corporation (CSC), distribute provider checks and paper remittances using the Pay-To Address on file. Other correspondence is directed to the Correspondence Address on file for a provider.
Often, direct mail notifications about important information are directed to the correspondence address. You may be missing out on such notifications if your address on file is outdated. From time to time, CSC Provider Services representatives will need to contact a provider by telephone with important information that may impact claims processing and payment.
First Verify
To verify the address and telephone information on file with CSC, please contact the Call Center at:
(800) 343-9000.
Then Update
To update address and telephone number information, follow the instructions below for printing the appropriate form. If you do not have internet access, the Call Center can provide you with a copy of the form.
The Change of Address form must contain the original signature of the provider listed on the form. The use of white out, red ink or double-sided forms is unacceptable and will cause rejection of the form.
Fee-for-Service providers can obtain more information on where to direct address change requests by going to:
Rate-based providers can obtain more information on where to direct address change requests by going to:
Seminar Schedule and Registration
Return to Table of Contents
- Do you have billing questions?
- Are you new to Medicaid billing?
- Would you like to learn more about ePACES?
If you answered YES to any of these questions, please consider registering for a Medicaid seminar. Computer Sciences Corporation (CSC) offers various types of seminars to providers and their billing staff. Many of the seminars planned for the upcoming months offer detailed information and instruction about Medicaid's web-based billing and transaction program - ePACES. ePACES seminars are designed for specific provider types.
ePACES is the electronic Provider Assisted Claim Entry System that allows enrolled providers to submit the following types of transactions:
- Claims
- Eligibility Verifications
- Utilization Threshold Service Authorizations
- Claim Status Requests
- Prior Approval Requests
Professional providers such as physicians, nurse practitioners and private duty nurses can even submit claims in "REAL-TIME" via ePACES. Real-time means that the claim is processed within seconds and professional providers can get the status of a real-time claim, including the associated paid amount, without waiting for the remittance advice to be delivered.
Seminar locations and dates are available at the eMedNY website. Seminar registration is fast and easy. Seminars are free to enrolled Medicaid providers.
Go to http://www.emedny.org/training/index.aspx to find and register for the eMedNY Training Seminar appropriate for your provider category and location. Review the seminar descriptions carefully to identify the seminar appropriate to meet your training needs. Registration confirmation will be instantly sent to your email address.
If you are unable to access the internet to register, you may also request seminar schedule and registration information by contacting CSC's Fax on Demand at 800-370-5809, request document number 1001 for a list of seminars and registration information to be faxed to you.
Please contact the eMedNY Call Center at (800) 343-9000 if you have questions about registration.
CSC Regional Representatives look forward to meeting with you at upcoming seminars!
Individual Provider Training Is Available
How to Make the Request
Return to Table of Contents
Computer Sciences Corporation (CSC) has Regional Representatives available to assist individual providers and resolve a variety of Medicaid claiming difficulties they may be experiencing.
CSC Regional Representatives can help providers with issues/problems such as:
- Billing problems (paper or electronic).
- ePACES usage.
- Prior Approval completion issues.
- Eligibility verification or service authorization response issues.
- Remittance interpretation (review solutions for pending and denied claims).
Providers may request to be contacted by a Regional Representative to request an individual training session by calling the Call Center at:
(800) 343-9000
or via email at the following address:
emednyproviderrelations@csc.com
If using the email method to request a call from a representative, please include your provider identification number, the nature of your request, and contact information. A CSC Regional Representative will contact you either via email or telephone to discuss your needs.
Claims Pended For Review By The Office of the State Comptroller
Return to Table of Contents
The New York State Constitution requires the Office of the State Comptroller (OSC) to audit all vouchers before payment. This requirement includes claims that are submitted to the Medicaid Program.
Effective immediately, OSC, as part of its audit process, will suspend certain claims from the Medicaid payment procedure in order to conduct a more thorough review of those claims.
Some providers will see a new basis for claims pending or denied. The eMedNY edit code and reason associated with the OSC Edit is 02014 - Claim Under Review by the Office of the State Comptroller. If a provider is receiving the HIPAA-compliant error codes, then the OSC edit will be mapped to Claim Adjustment Reason Code 95 - Benefits Adjusted. Plan Procedures Not Followed.
If a provider has claims pending or denied for this reason, a representative from OSC will contact the provider to discuss the provider's claims. This may include scheduling an appointment to visit the provider's facility to inspect medical records and other documentation supporting the claims being reviewed.
Under the Code of Federal Regulations (45 CFR § 164.512(d)(1) (HIPAA)), medical providers are permitted to disclose protected health information to an oversight agency, for oversight activities which are authorized by law, such as audits. For purposes of HIPAA, OSC is an oversight agency.
Although no specific information about OSC pending and/or denied claims can be obtained by calling the eMedNY Call Center, other billing questions should be directed there at:
(800) 343-9000.
Submission of Medicaid Claims Over Two Years Old
Voiding and Adjusting of Paid Claims
Return to Table of Contents
This is to reaffirm the Department policy with regard to the submission of claims over two years old. Acceptable reasons for a claim to be submitted after two years are:
- if the provider can produce documentation verifying the two-year delay was caused by the Department, the local social services district, or other agents of the Department; or
- if a court has ordered the Department to make payment.
When a provider voids a previously paid claim and now wishes to resubmit, the resubmission is treated as a new claim and will be subjected to the criteria above for the submission of claim(s) over two years old. All timely submission rules will apply. The new claim will not be considered as an agency error and, therefore, will not qualify for a waiver of the two-year regulation.
Adjustments, rather than voids, should always be billed to correct a paid claim(s).
Information regarding this policy is located in the General Billing subsection, Information for All Providers section of your provider manual at:
and a previous article related to timely submission of claims published in the November 2006 Medicaid Update.
For questions regarding claims over two years old, please call:
(800) 562-0856, option #3; or
(518) 473-4029.
Accessing the Medicaid Eligibility Verification System
Return to Table of Contents
Accessing the Medicaid Eligibility Verification System (MEVS) prior to providing services is essential to your claim payment.
HERE IS A FAST AND FREE METHOD TO ACCESS MEVS
Use ePACES
To obtain Real Time (FAST) responses for the following requests: ELIGIBILITY, SERVICE AUTHORIZATIONS (SA) and UTILIZATION THRESHOLD (UT's) or DISPENSING VALIDATION SYSTEM (DVS)
Sign up for ePACES and make it available to your staff at patient registration or reception sites. Providers who do not verify eligibility and conditions of coverage before rendering services to Medicaid patients run a risk of non-payment of claims.
ePACES is a free web-based application available to any provider with Internet access and an email address (for enrollment).
ePACES Eligibility Response Detail report will provide the following MEVS information:
- Eligibility details
- Service Authorization (and Utilization Threshold - UT) response (when SA is selected)
- Dispensing Validation System authorization number (when DVS is selected)
- Managed Care plan information and a listing of covered services
- Medicare and other insurance coverage information
- Spend-down (patient participation)
- Restricted patient alerts
- Patient exception codes
You can print the ePACES eligibility response and file it for future reference, or you can use ePACES' Search Criteria function to access stored responses, as needed.
For other methods of accessing MEVS, please consult the MEVS manual at:
http://www.emedny.org/ProviderManuals/AllProviders/MEVS/MEVS_Provider_Manual/1_0/mevs_manual.html
- ePACES is faster than the touch-tone telephone method
- ePACES is free, unlike the card-swipe terminal method or software needed to submit 270 eligibility transactions.
To sign up for ePACES contact the Call Center at (800) 343-9000.
Do it today!
Policy and Billing Guidance........
Preferred Drug Program
Return to Table of Contents
Provider Reminders:

- All enrollees who receive pharmacy services through the Medicaid fee-for-service program, including those in Medicaid and Managed Care plans, are subject to the Preferred Drug Program (PDP).
Those in Family Health Plus and Child Health Plus B (the non-Medicaid Program) receive medications through their managed care plan, and are not affected. - All prescriptions for Medicaid enrollees must include the prescriber's name, address, telephone number, and profession, and if applicable, the DEA (Drug Enforcement Agency) number. Providing accurate contact information ensures that the prescriber can be reached if there is a problem dispensing the prescription.
- When prescribing drugs in classes that are subject to the PDP, prescribers should first check whether the drug is preferred or non-preferred. Remember: preferred drugs can be prescribed without prior authorization!
Get the facts!
Providers should always look to trusted sources for information about changes to the Preferred Drug List. The Department of Health and First Health Services websites, as well as the monthly Medicaid Update publication, are such trusted sources.
For information on the Medicaid Preferred Drug Program visit one of the following websites:
http://www.emedny.org/, http://www.health.state.ny.us/, https://newyork.fhsc.com/.
Additional information is available by calling the pharmacy prior authorization clinical call center at
(877) 309-9493.
For clinical concerns or preferred drug program questions, call:
(877) 309-9493.
For billing questions, call:
(800) 343-9000.
For Medicaid Pharmacy Policy and Operations questions, call:
(518) 486-3209.
Reimbursement Changes for Pharmacy Claims
Effective July 1, 2007
Return to Table of Contents
Pharmacy reimbursement for prescription drugs under the New York State Medicaid program is limited to:
- The federal upper limit (FUL) for specific multiple source drugs; or
- The lower of the billing pharmacy's usual and customary price charged to the general public, or the estimated acquisition cost (EAC) established by the Department of Health.
The following changes have been made to the EAC definitions which will affect pharmacy reimbursement for drugs provided on or after July 1, 2007:
- Sole or Multi-source Brand Drugs
The average wholesale price (AWP) minus fourteen percent (14%). - Multi-source Generic Drugs
The lower of the average wholesale price (AWP) minus twenty-five percent (25%), or, the State based maximum acquisition cost (SMAC).
There will be no change to the current reimbursement rates for specialized HIV pharmacies which meet specific programmatic and operational criteria.
Questions may be directed to the Medicaid Pharmacy Policy and Operations staff at: (518) 486-3209.
Fraud impacts all taxpayers.
Return to Table of Contents
Do you suspect that an enrollee or a provider has engaged in fraudulent activities?
Please call:
1-877-87FRAUD
Your call will remain confidential.
Attention:
Pharmacy Providers
You Must Bill Medicare First!
Return to Table of Contents
Edit 152 message:
Recipient File Indicates Medicare/NoMedicare Present [i.e., while the enrollee has Medicare coverage, you have not entered any information on your claim regarding Medicare payment.]
For an enrollee with both Medicare and Medicaid coverage, all charges for Medicare covered drugs and supplies must be billed to Medicare first.
New Claim Edit for Pharmacies
Effective July 2, 2007, Medicaid will implement claims processing Edit 152 f or supplies, to ensure that Medicaid is billed as a last resort when an enrollee is both Medicare/Medicaid dually eligible (dual eligibles) and the drug or supply is covered by Medicare.
Drugs will be added in the near future; providers will be notified through the Medicaid Update.
Billing for Medicare/Medicaid Dual Eligibles
Pharmacies must be enrolled in Medicare in order to bill Medicaid for drugs or supplies provided to dually eligible enrollees. Pharmacies must indicate the Medicare paid amount on the submitted Medicaid claim or payment will be denied.
Pharmacies not enrolled in Medicare and attempting to bill Medicaid for drugs and supplies for dual eligibles will not be paid.
Medicare Quantity Limits
Medicare currently covers 100 strips and 100 lancets every 3 months for non-insulin dependent diabetics. Additionally, Medicare currently covers 100 strips and 100 lancets every month for insulin dependent diabetics without additional documentation.
Information on coverage of larger quantities can be found under Local Coverage Determinations for A4253 and A4259 at:
Physicians Billing for Critical Care
Clarification on Procedure Codes
Return to Table of Contents
The Medicaid Program allows physicians to bill two distinct procedure codes when critical care is rendered to a Medicaid enrollee:
Critical Care Definition:
Extraordinary care by the attending physician in personal attendance in the care of a medical emergency, both directing and personally administering specific corrective measures after initial examination had determined the nature of the ailment.
- Procedure code 99291: Critical care, evaluation and management of the critically ill or critically injured patient, requiring the constant attendance of the physician; first hour.
- Procedure code 99292: each additional 30 minutes (Listed separately, in addition to code 99291 for primary service).
If you bill the critical care procedure code(s) above, the services listed below are included. Thus, when billing for Critical Care procedure codes, the following services (with procedure codes in parentheses) should not be billed in addition to the Critical Care procedure codes:
- the interpretation of cardiac output measurements (93561, 93562),
- chest X-rays (71010, 71015, 71020),
- pulse oximetry (94760, 94761, 94762),
- blood gases, and information data stored in computers (e.g., ECGs, blood pressures, hematologic data (99090));
- gastric intubation (43752, 91105);
- temporary transcutaneous pacing (92953),
- ventilatory management (94656, 94657, 94660, 94662); and
- vascular access procedures (36000, 36410, 36415, 36540, 36600).
Any services performed which are not listed above should be reported separately.
Additionally, when critical care is provided by a physician during transport, the critical care codes 99291 and 99292 should be reported for the physician's attendance.
For additional and more detailed information on Critical Care, please consult the Procedure Codes & Fee Schedule section of the Physicians Provider Manual, available on line at:
Attention:
Physicians
Nurse Practitioners
Licensed Midwives
Article 28 Hospital Based and Freestanding Clinics
National Drug Code
Required on Medicaid Claims
Return to Table of Contents
The federal Deficit Reduction Act (DRA) of 2005 (at Section 6002) added provisions requiring ambulatory care providers to collect and submit National Drug Code (NDC) numbers on Medicaid claims.
While the implementation date is yet to be determined, this provision will require all claims for physician-administered drugs to include the 11-digit NDC code (which identifies the drug and manufacturer).
To ensure federal funding for drugs under the Medicaid Program, the New York State Medicaid Program will be collecting rebates based on the information provided on these claims.
Following implementation, claims for physician-administered drugs without valid 11-digit NDC numbers will be rejected.
Drugs subject to this provision include drugs commonly administered and billed in the ambulatory setting (e.g., chemotherapeutics, immune globulins, etc.).
Additional information will be provided in future Medicaid Update articles, as more details become available.
Questions may be directed to the Medicaid Pharmacy Policy and Operations staff at: (518) 486-3209.
Attention:
Practitioners Who Order Transportation Services
Reviewing Your Transportation Rosters
Return to Table of Contents
For a transportation provider to receive prior authorization to render non-emergency ambulance, ambulette, and New York City livery transportation services, the identity of the practitioner ordering the transportation must be furnished to Medicaid.
When the Prior Authorization request is approved, a copy of the roster containing the prior authorization information is sent to the ordering provider. Upon receipt of the roster, the practitioner should review the information to ensure that the patient(s) on the roster were referred by the physician receiving the roster.
If any of the patient(s) on the roster were not referred for transportation services, then a copy of the roster should be sent to Computer Sciences Corporation, with a cover letter explaining that the services for the indicated patient(s) were not referred by the practitioner identified on the roster. Both the roster and cover letter should be sent to:
Computer Sciences Corporation
Attn: eMedNY FRAUD
1 CSC Way
Rensselaer, New York 12144
Questions? Please contact the eMedNY Call Center at (800) 343-9000.
Medicaid Reimbursement for Implanon
Return to Table of Contents
Effective for dates of service on or after May 1, 2007, Medicaid is reimbursing for the Food and Drug Administration approved contraceptive Implanon.
- Implanon is a non-biodegradable, etonogestrel containing single rod implant for subdermal use.
- This is a practitioner administered contraceptive drug, and is indicated for women for the prevention of pregnancy for up to three years.
Coding Instructions
Reimbursement for Implanon is limited to the provider's actual acquisition cost from the manufacturer. Procedure code S0180 should be used to bill Medicaid for the acquisition cost.
The CPT-4 insertion/removal codes and associated fees are:
| 11975 | - Insertion, implantable contraceptive capsules ($81.00) |
| 11976 | - Removal, implantable contraceptive capsules ($57.00) |
| 11977 | - Removal with reinsertion, implantable contraceptive capsules ($109.50) |
Implanon Administered in a Private Practitioner Office - Physician, Nurse Practitioner, Licensed Midwife
- Practitioners should bill actual acquisition cost for Implanon under procedure code S0180. Professional component (insertion/removal of the capsule) should be billed under CPT-4 codes 11975, 11976, or 11977 as appropriate.
Implanon Administered in an Article 28 Certified Diagnostic and Treatment Center to a Registered Clinic Patient
- The all-inclusive clinic threshold rate should be billed to Medicaid. Cost of materials and professional fees are included in the threshold rate.
Implanon Administered in an Article 28 Certified Hospital Outpatient Department to a Registered Clinic Patient
- The all-inclusive clinic threshold rate should be billed to Medicaid. Cost of materials is included in the clinic threshold rate.
- The professional fee is included in the threshold rate if the practitioner is salaried.
- The professional fee may be billed to Medicaid fee-for-service for non-salaried practitioners.
Ordered Ambulatory - Implanon Administered in an Article 28 Certified Diagnostic and Treatment Center or Hospital-Based Outpatient Department as an Ordered Service (Not a Registered Clinic Patient):
- An ordered/referred ambulatory service is one that is performed by a hospital or diagnostic and treatment center on an ambulatory basis. The service is ordered by a qualified physician, physician's assistant, nurse practitioner, licensed midwife, or the appropriate staff of a clinic not affiliated with the hospital or diagnostic and treatment center which is providing the ordered ambulatory service.
Facilities should bill cost of materials at actual acquisition cost. The physician should bill the professional fee for the insertion/removal procedure code. In addition, a clinic must be enrolled in the Medicaid program with the designated category of service of 0163 (ordered ambulatory diagnostic and treatment center) or 0282 (hospital based ordered ambulatory).
Medicaid managed care and Family Health Plus enrollees
Medicaid managed care plans that cover family planning services must cover Implanon. The cost of the device is never considered a pharmacy item and must always be included in the cost of the practitioner or clinic services.
- Clinics and practitioners who have contracts with a patient's Medicaid Managed Care plan to provide family planning services may not bill Medicaid fee for service for Implanon.
- Clinics and practitioners who do NOT have contracts with a patient's Medicaid managed care plan to provide family planning services may see patients that request Implanon on a self referral basis only. A self referred managed care enrolled patient can not be considered a recipient of ordered ambulatory services, but is considered a registered clinic patient.
Family Health Plus (FHPlus) plans that cover family planning services must cover at least one type of implantable contraceptive. Enrollees in FHPlus plans that do not cover family planning services can obtain implantable contraceptives from Medicaid clinics and practitioners.
Questions for enrollees not in a managed care plan may be directed to the Division of Financial Planning and Policy, Bureau of Policy Development and Agency Relations at:
(518) 473-2160.
Questions for enrollees in a managed care plan may be directed to the Division of Managed Care and Program Evaluation, Bureau of Managed Care Program Planning at:
(518) 473-7467.
Durable Medical Equipment Fee Schedule Changes
Effective for dates of service on or after May 1, 2007
Return to Table of Contents
The following Durable Medical Equipment codes have been updated:
| HCPCS CODE | LONG DESCRIPTION | FEE |
| E2366 | Power wheelchair accessory, battery charger, single mode, for use with only one battery type, sealed or non-sealed, each. | $246.60 |
| E2603 | #Skin protection wheelchair seat cushion, width less than 22 inches, any depth. | $148.38 |
| E2604 | #Skin protection wheelchair seat cushion, width 22 inches or greater, any depth | $177.09 |
- Bolded codes indicate that prior approval is required.
- When the code description is preceded by a "#," Dispensing Validation System (DVS) prior authorization is required.
Questions can be referred to the Pre-Payment Review Group at (518) 474-8161.
Missing Issues?

The Medicaid Update, indexed by subject area, can be accessed online at the New York State Department of Health website:
http://www.health.state.ny.us/health_care/medicaid/program/update/main.htm
Hard copies can be obtained upon request by emailing:
General Information........
Attention:
Prescribers
Antibiotic Resistance and the Judicious Use of Antibiotics
Return to Table of Contents
To help reduce the appearance and spread of antibiotic resistance, prescribers are encouraged to:
- be familiar with local data on resistance,
- prescribe antibiotics that target only a narrow range of bacteria, and
- reserve broad spectrum antibiotics as second line therapy.
For more information on antibiotic use and resistance, please refer to the Centers for Disease Control and Prevention website at:
http://www.cdc.gov/drugresistance
LYME DISEASE ALERT
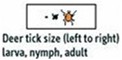

DO A THROUGH BODY CHECK FOR TICKS AFTER BEING OUTDOORS.
How To Remove A Tick
- - Using tweezers, grasp tick near the mouth parts, as close to skin as possible.
- - Pull tick in a steady, upward motion away from skin.
- - DO NOT use kerosene, matches, or petroleum jelly to remove tick.
- - Disinfect site with soap and water, rubbing alcohol or hydrogen peroxide
- - Record date and location of tick bite. If rash or flu-like symptoms appear contact your health care provider immediately.
DISEASE RISK IS REDUCED IF TICK IS REMOVED WITHIN 36 HOURS
New York State Department of Health
For more information about ticks and Lyme Disease, go online to: http://www.nyhealth.gov/nysdoh/environ/lyme/home.htm
Attention:
Pharmacy/DME
Nursing
Eye Care
Physicians
Using the eMedNY 361501 - Prior Approval Request Form
Return to Table of Contents
When filling out this form, please refer to your Provider Manual, Prior Approval Guidelines, Section III for Field by Field Instructions for the correct way to complete the 'ID/License Number' in Field 3 of this form, (if this field is incorrectly completed, the processing of your prior approval number may be delayed).
Provider Manuals are available online at:
http://www.emedny.org/ProviderManuals/index.html
Medicaid ID Number
Enter the Ordering Provider's Medicaid ID Number as in the example below. Right justify the information in this field.
Example:
ID/LICENSE NUMBER
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
License Number
If the Ordering Provider is not enrolled with the Medicaid Program, enter his/her license number and 3-digit profession code.
If entering a New York State license number, the license number must be preceded by two zeros (and be 8 digits) as in the example below.
Example:
ID/LICENSE NUMBER
| 0 | 0 | 2 | 3 | 4 | 5 | 6 | 7 |
If entering an out-of-state license number, the two-digit United States Post Office state abbreviation should be entered in place of the two zeros, as in the example below.
Example:
ID/LICENSE NUMBER
| N | J | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
If you have any questions, please contact the eMedNY Call Center at:
(800) 343-9000.
Managing the Costs of Arthritis and Other Chronic Diseases
Arthritis is currently the leading cause of disability in the United States.
Return to Table of Contents
The Centers for Disease Control and Prevention (CDC) reports that in 2003 the total cost of arthritis and other rheumatic conditions (AORC) in the United States was $127.8 billion. In New York State:
- The total cost of AORC for 2003 was approximately $8.7 billion.
- Sixty-four percent ($5.6 billion) of this total cost goes to direct cost or medical care expenditures; and
- 36% ($3.2 billion) of the total cost is indirect costs or costs related to lost earnings (due to illness or disability).
- New York State has the second highest total AORC costs in the U.S. (just after California).
These costs for both New York State and the entire U.S. have been increasing and are predicted to continue to increase as the population ages. 1
Individuals with doctor-diagnosed arthritis are often dealing with additional chronic conditions or risk factors for chronic conditions that can increase healthcare costs and disability. In New York State:
- 52% of adults with cardiovascular disease have arthritis.
- Approximately 47% of adults with hypertension have arthritis, and 42% of adults with high cholesterol (both of which are risk factors for cardiovascular disease) have arthritis.
- In addition, 39% of New York State adults who are obese and 35% of adults who are inactive have arthritis.
- The disease also affects adults with diabetes. 50% of adults with diabetes also have arthritis. 2
Increasing costs point to the need for expanding efforts to reduce AORC costs and reduce disability caused by AORC and other chronic diseases. There are several evidence-based programs that have been developed for individuals with arthritis or other chronic conditions that provide opportunities for physical activity or teach disease self-management skills. Certain physical activity programs and disease-self-management programs have proven to be effective in reducing health care costs and disability. The New York State Department of Health Arthritis Program assists in implementing five suchevidence-based programs: two Self-Management and Education programs (the Arthritis Foundation Self Help Course and the Chronic Disease Self-Management Program) and three Physical Activity Programs (the Arthritis Foundation Exercise Program, the Arthritis Foundation Aquatic Program, and EnhanceFitness).
Self-management education programs teach people with arthritis how to manage arthritis on a day-to-day basis. For example, the Chronic Disease Self-Management Program is a course designed for individuals with any chronic disease. This course teaches appropriate exercise and use of medications, communicating effectively with family, friends, and health professionals, nutrition, making informed treatment decisions, problem solving, and planning for the future. This program has been shown to reduce health distress, fatigue, and disability, as well as health care costs through fewer hospitalizations and fewer physician visits for program participants.3,4 Despite the effectiveness of this and other courses like it, only 9.5% of New York State adults with arthritis report ever taking a disease self-management course.2
Physical Activity Programs provide opportunities for learning and doing physical activity that is designed for individuals with arthritis and in the case of EnhanceFitness designed for all older adults. Research has shown that appropriate physical activity offers substantial benefits to people with arthritis and can decrease pain and disability.5,6 Physical activity is also integral to the management of other chronic diseases such as cardiovascular disease.
Reducing the cost of AORC in personal health and economic terms requires that greater effort be taken to support evidence-based programs like those listed above that help adults manage the affects of arthritis and lead healthier lives. To work toward this goal the Arthritis Program has enlisted a broad base of partners, including Area Agencies on Aging, rural health networks, the State University of New York, and independent living centers to implement the evidence-based programs throughout the state. An ever growing network of partnerships is needed to reach even more people and sustain these programs and the benefits of these programs long-term.
1 CDC. National and State Medical Expenditures and Lost Earnings Attributable to Arthritis and other Rheumatic Conditions - United States, 2003. MMWR 2007, 56; 4-7.
2 New York State Behavioral Risk Factor Surveillance System. 2005.
3 Lorig K.R., Sobel D.S., Stewart A.L., Brown Jr B.W., Ritter P.L., González V.M., Laurent D.D., & Holman H.R. Evidence suggesting that a chronic disease self-management program can improve health status while reducing utilization and costs: A randomized trial. Medical Care. 1999; 37(1):5-14.
4 Lorig K.R., Ritter P., Stewart A.L., Sobel D.S., Brown B.W., Bandura A., González V.M., Laurent D.D., & Holman H.R. Chronic Disease Self-Management Program: 2-Year Health Status and Health Care Utilization Outcomes. Medical Care. 2001; 39(11), 1217-1223.
5 Doyle M.A., Farrar V., Ryan S., & Sisola S. An evaluation of PACE. Arthritis Care Res. 1990; 3(2): S7.
6 Suomi R. & Lindauer S. Effectiveness of the Arthritis Foundation Aquatic Program on strength and range of motion in women with arthritis. J Aging Phys Activ. 1997; 5: 341-351.
Save the Date
Return to Table of Contents
The New York State Department of Health
Is pleased to announce
"Planning Today for Tomorrow"
A statewide symposium on Long Term Care Restructuring
June 21, 2007
Please join us at the Empire State Plaza Convention Center in Albany, New York on Thursday, June 21, 2007.
"Planning Today for Tomorrow" participants will be updated on current New York State restructuring activities, examine the special needs of those requiring long term care, review the best practices and innovations of New York State counties and other states, and plan for future activities.
Numerous workshops on topics such as Care Coordination; Affordable Senior Housing; Workforce Development; Children in Long Term Care; and Informal supports, will be offered during this daylong event.
Listed below are two keynote speakers who will also present during the day:
- Joshua Weiner, Senior Fellow and Program Director of aging, disability, and long-term care from RTI International; and
- Tom Nerney, Director and Co-founder of the Center for Self-Determination.
The registration brochure can be obtained at the following website:
http://www.nyhealth.gov/events/planning_today_for_tomorrow/
We look forward to seeing you then!

PROVIDER SERVICES
Return to Table of Contents
Missing Issues?
The Medicaid Update, now indexed by subject area, can be accessed online at the New York State Department of Health website:
http://www.nyhealth.gov/medicaid/program/update/main.htm
Hard copies can be obtained upon request by emailing: MedicaidUpdate@health.state.ny.us
Questions About an Article?
For your convenience each article contains a contact number for further information, questions or comments.
Questions about billing and performing MEVS transactions?
Please contact CSC Provider Services at: (800) 343-9000.
Provider Training
To sign up for a provider seminar in your area, please enroll online at: http://www.emedny.org/training/index.aspx
Patient Eligibility
Call the Touchtone Telephone Verification System (800) 997-1111, (800) 225-3040 or (800) 394-1234.
Address Change?
Questions should be directed to CSC at (800) 343-9000, option 5.
Fee-for-service Provider Enrollment
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/Provider Maintenance Forms/6101-Address Change Form.pdf.
Rate-based/Institutional Provider Enrollment
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/Provider Maintenance Forms/6106-Rate Based Change of Address Form.pdf
Comments and Suggestions Regarding This Publication?
Please contact the editor, Timothy Perry-Coon at MedicaidUpdate@health.state.ny.us or via telephone at (518) 474-9219 with your concerns.
The Medicaid Update is a monthly publication of the New York State Department of Health containing information regarding the care of those enrolled in the Medicaid Program.