MMC Guidance - Process for Expedited Request for Assessment and the New York Independent Assessor
- Guidance is also available in Portable Document Format (PDF)
To: Medicaid Managed Care Plans, HIV Special Needs Plans (HIV SNPs), and Health and Recovery Plans (HARPs)
From: Office of Health Insurance Programs, Division of Health Plan Contracting and Oversight
Re: Process for Expedited Request for Assessment and the New York Independent Assessor (NYIA)
Issue Date: November 17, 2022
This guidance provides instructions for an expedited request for an initial assessment for Personal Care Services (PCS) and/or Consumer Directed Personal Assistance Services (CDPAS). This change impacts enrollees in all Medicaid Managed Care (MMC) plans. This notification applies to MMC plans, including Mainstream Medicaid Managed Care plans, HIV Special Needs Plans (HIV SNPs), and Health and Recovery Plans (HARPs). Authorization for expedited PCS and/or CDPAS will now be made based on the MMC plans review of the New York Independent Assessor (NYIA) assessment.
As of December 1, 2022, an MMC plan enrollee with an expedited assessment request for PCS and/or CDPAS must have their Community Health Assessment (CHA) and Independent Practitioner Panel (IPP) Practitioner Order (PO) clinical appointment conducted by the New York Independent Assessor (NYIA). NYIA will conduct all expedited initial assessments and clinical appointments for PCS and/or CDPAS for adult enrollees (18 and over) in an MMC plan. The CHA and clinical appointment completed by the NYIA will assess for PCS and/or CDPAS service needs. The MMC plan will no longer conduct the CHA for expedited requests but will remain responsible for care planning and authorizing these services in accordance with 18 NYCRR sections 505.14 and 505.28.
Step 1:
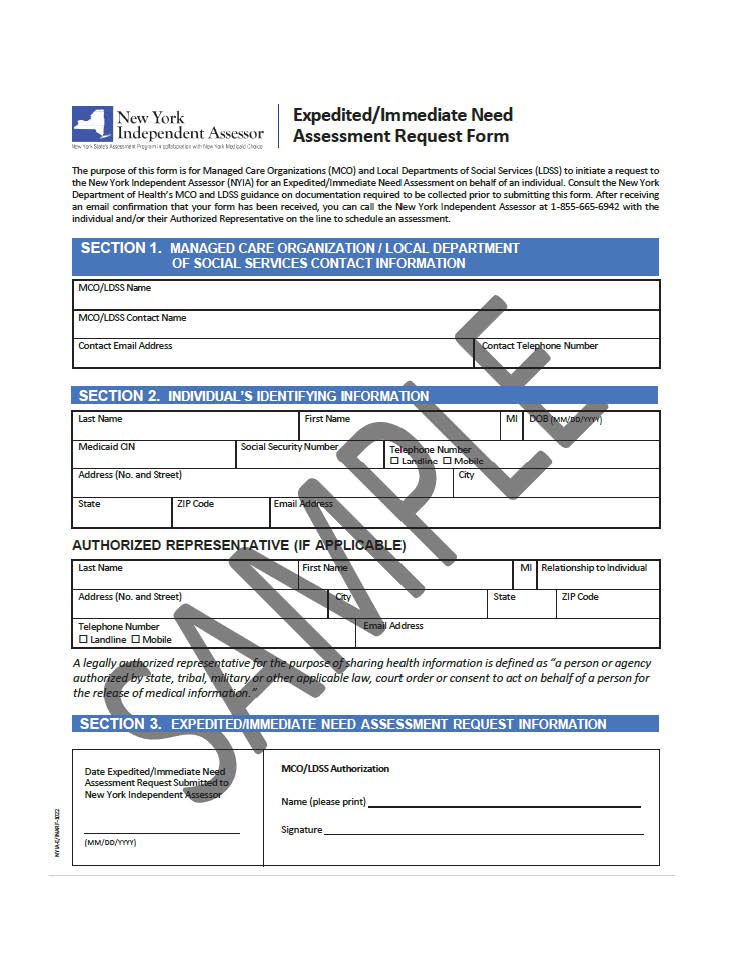
To schedule an expedited initial assessment by NYIA, the MMC plan must use the Expedited/Immediate Need Form. This is a web-based form to be completed electronically through a secure URL. A sample of the form is attached to this guidance document. Plans must request the dedicated URL by emailing NYIAHPA@maximus.com and NYIA will reply providing the MMC plan with the dedicated URL. Once the form is submitted electronically, the plan will receive an auto-generated email confirmation the form has been received.
Note:If an enrollee seeking an initial assessment for PCS and/or CDPAS on an expedited basis self-refers to NYIA or is directed to NYIA by a discharge planner or other referral source, the NYIA Customer Service Representative (CSR) will direct the individual to call back with a MMC plan representative.
Step 2:
After the MMC plan transmits the expedited review request through submission of the Expedited/Immediate Need Form, the MMC plan initiates a three-way call with the NYIA Operations Support Unit (OSU) and the enrollee and/or their representative after the form has been submitted. The NYIA OSU number is 1-855-665-6942. During the three-way call, the NYIA CSR will schedule a CHA and clinical appointment to be completed within six (6) calendar days of the call. All other aspects of the CHA and clinical appointment are the same as the initial assessment process described in the MMC plan guidance issued on April 28, 2022.
Step 3:
Once the CHA and clinical appointments are complete, NYIA will send the MMC plan a report. This will be sent daily and include expedited request information including the CHA and PO outcomes. This will allow the MMC plan to track assessment progress.
In addition, the MMC plan will receive a daily report that is triggered when one of the statuses listed below changes within a 24-hour period:
- Expedited CHA/Clinical Appointment no show;
- Expedited CHA/Clinical Appointment cancelation; or
- Expedited CHA/Clinical Appointment interruption.
Step 4:
Once a case on the daily report has a completed CHA and PO the MMC plan is considered in receipt of the expedited request and must prepare the Plan of Care (POC) and process the services authorization request as outlined in the Medicaid Managed Care Model Contract and 42 CFR § 438.210(d)(2).
Step 5:
(As needed) If, during the development of the POC, the MMC plan finds the enrollee in need of a high needs review, i.e., the POC includes 12 or more hours per day, on average, of PCS/CDPAS, the MMC plan must refer the case to NYIA’s Independent Review Panel (IRP) for an additional independent medical review and must consider the recommendation of the IRP when finalizing the POC. See 18 NYCRR §§ 505.14(b)(2)(v) and 505.28(d)(5).
When the requirement to perform an IRP review is triggered, the MMC plan must submit the web-based IRP Request Form electronically via the designated, secure URL for the MMC plan and include in the referral to the IRP all records and documents used to develop the POC.
Timeframes for authorizing services are not pended for high-needs cases that are forwarded to the IRP. In the event the IRP review would impact the MMC plan’s ability to authorize services pursuant to an expedited review of PCS and/or CDPAS, the MMC plan must authorize a proposed Plan of Care (POC) on a temporary basis pending review of the IRP recommendation. See 18 NYCRR §§ 505.14(b)(4)(vi) and 505.28(e)(4). Services of more than 12 hours per day on average may be provided under a temporary plan of care due to the expedited need. Upon receipt of the IRP recommendation, the MMC plan will finalize the POC and issue an initial determination notice.
General questions may be submitted to: omcmail@health.ny.gov.
NYIA specific questions may be submitted to: independent.assessor@health.ny.gov.