Value Based Payment Quality Improvement Program (VBP QIP)
Update Webinar
- Webinar also available in Portable Document Format (PDF)
- VBP Bootcamp Meeting One recorded webinar
October 2016
Today´s Agenda
- VBP QIP Governance Documents
- VBP QIP Timeline Update
- VBP QIP Facility Plans
- VBP QIP Financing Update
- Moving Towards VBP
- The VBP Landscape
- Contracting for VBP
- VBP – Final Notes
- Next Steps and Q&A
- Open Forum
VBP QIP Updates
VBP QIP Governance Documents
- Group 1 MCO Governance Documents were submitted to DOH on Friday, September 16th, 2016.
- DOH provided MCOs with feedback on the Governance Documents on Tuesday, October 11th, 2016.
- Group 2 MCO Governance Documents are due on Friday, December 9th, 2016.
- Group 2 MCO's has the option to submit their governance documents by Friday, October 7th, 2016 if they wanted to obtain DOH's feedback.
- A blank Governance Document Scorecard can be found on the DOH VBP QIP website.
- The Scorecard outlines the areas DOH reviews, which the MCO´s can use to establish a solid approach for overseeing their programs. This will reinforce the integrity of each program and will foster the parameters that will assist the MCO's paired Facilities with achieving their VBP QIP objectives.
VBP QIP Timeline Update
Group 1 Key Upcoming Dates
| Milestone | Due Date |
|---|---|
| MCO Quarterly Reporting to DOH (April 2016 – Ongoing) – MMCOR Submissions | November 15, 2016 |
| First steps towards VBP undertaken with PPS & MCO oversight in accordance with approved Facility Plan | Ongoing |
Group 2 Key Upcoming Dates
| Milestone | Due Date |
|---|---|
| PPSs review Facility Plan and return them to facilities for revision | October 28, 2016 |
| Baseline metrics for future measurement are co–developed by facility, PPS, & MCO (submitted as part of the Facility Plan) | October 28, 2016 |
| MCO Quarterly Reporting to DOH (April 2016 – Ongoing) – MMCOR Submissions | October 31, 2016 |
| MCOs submit a revised VBP QIP Governance Document to DOH for review | December 9, 2016 |
| Final Facility Plans approved by MCO in collaboration with PPS (final copies should be sent to DOH) | December 9, 2016 |
Note: Although deliverables can be completed at any time before the red dates noted on the VBP QIP Timeline, the Department encourages participants to complete them as soon as possible, as the majority of VBP QIP in DY2 focuses on setting up VBP contracts, which must be in place between Facilities and MCOs by April 1st, 2017.
|top of page|VBP QIP Facility Plans
- The Facility Plan Template provides guidance to participants on the information each party should consider when putting together their VBP transformation plan.
- The Facility Plan Template can be found on the DOH VBP QIP website.
- Group 1 Facility Plans were were submitted to DOH on Friday, September 16th, 2016.
- Finalized Facility Plans should have been approved by partnered MCOs and PPS.
- DOH will not be providing official scores for the Facility Plans, but will be reviewing the submitted documents, and will provide feedback that partners can choose to act upon..
- Group 2 Facility Plans are due to DOH by Friday, December 9th, 2016.
VBP QIP Financing
- Finalization of VBP QIP DSRIP Year (DY) 2 – April 2016 Rate Package
- DOH´s submission of the DY2 Rate Package to CMS & DOB is delayed
- Additional time was provided to the MCOs to review and comment on the rate package.
- DOH worked with DOB to gain approval for a state–funded advance for the 3rdQuarter (October 2016 – December 2016) to get VBP QIP funds to the MCO´s (until April 2016 rate is approved by CMS & DOB).
- DOH´s submission of the DY2 Rate Package to CMS & DOB is delayed
Moving Towards VBP
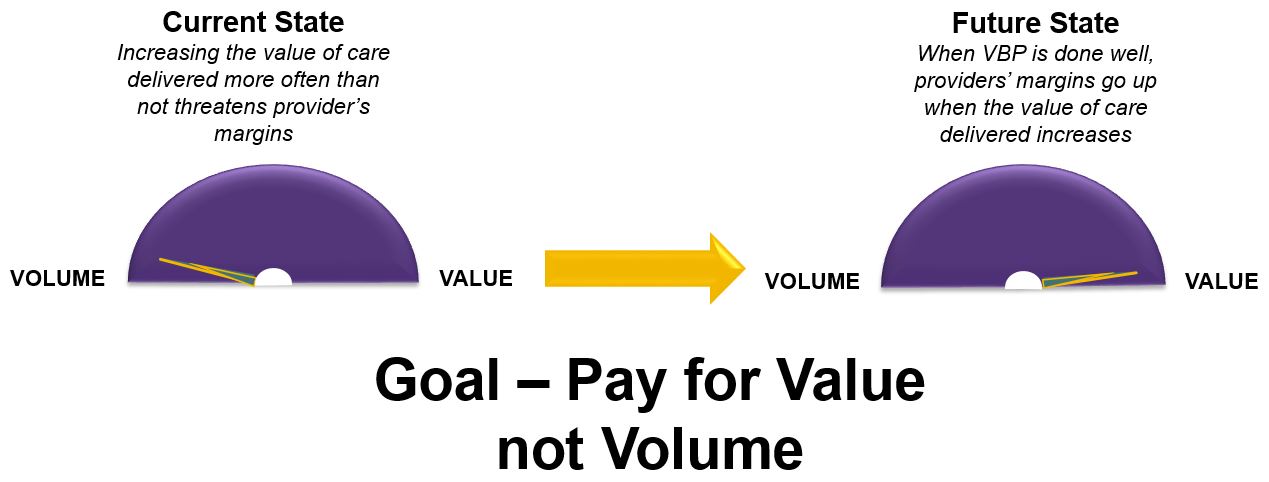
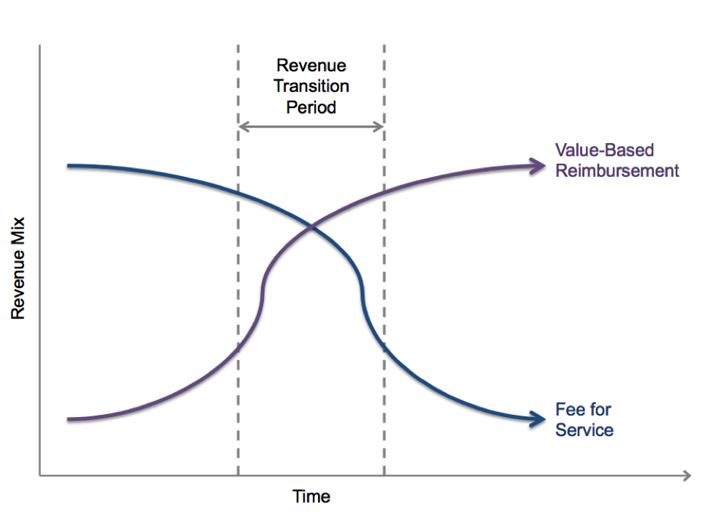
Payment Reform: Moving Toward VBP
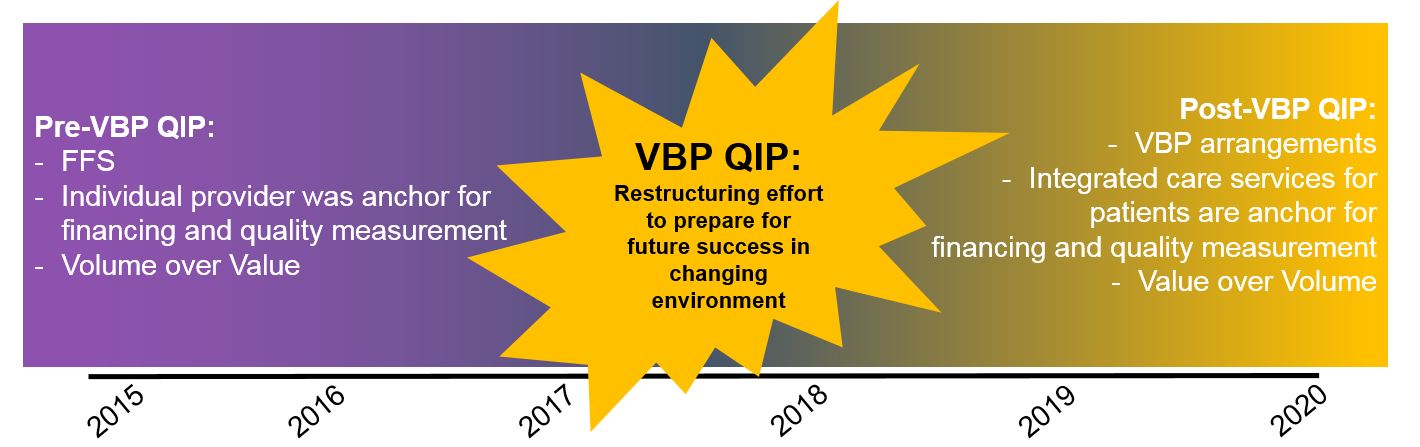
- A Five-Year Roadmap outlining NYS´ plan for Medicaid Payment Reform was required by the MRT Waiver.
- By DSRIP Year 5 (2019), all MCO´s must employ non fee–for–service payment systems that reward value over volume for at least 80–90% of their provider payments (outlined in the Special Terms and Conditions of the waiver).
- The State and CMS are committed to the VBP Roadmap, which core stakeholders (providers, MCO´s, unions, patient organizations) have actively collaborated in creating and updating.
- If Roadmap goals are not met, overall DSRIP dollars from CMS to NYS will be significantly reduced.
Payment Reform: VBP Arrangements
VBP arrangements are not intended primarily to save money for the State, but to allow providers to increase their margins by realizing value.
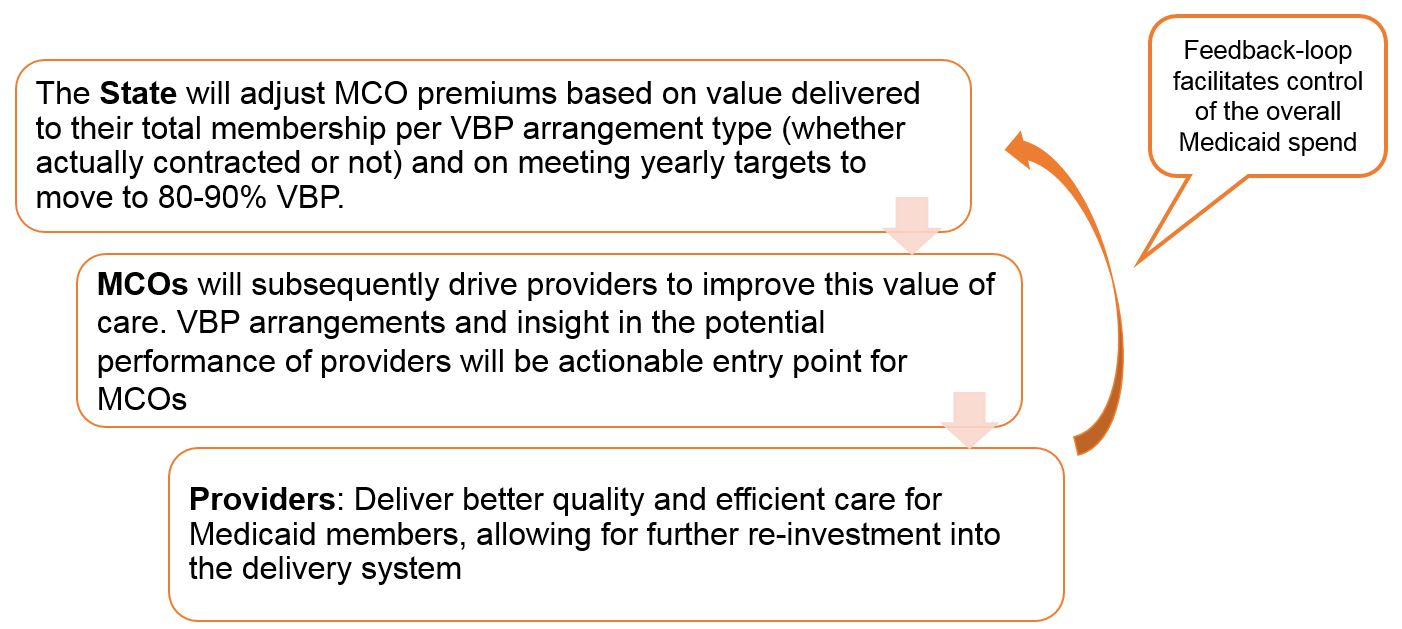
How VBP and VBP QIP Work Together
The VBP Landscape
VBP Goals
By April 2020, 80-90%* of Medicaid Managed Care Spend (Plan to Provider Payments) Will Be in VBP Level 1 and Higher
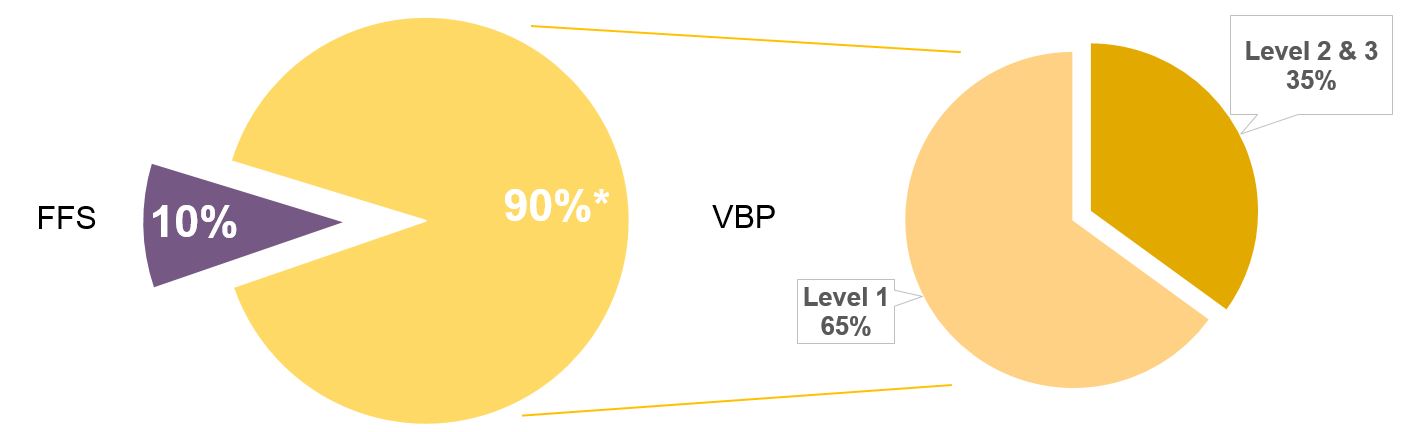
*Minimum of 80%; includes Managed Long–Term Care and (depending on move to Managed Care) care for the Intellectually/Developmentally Disabled
Aligning the Incentives is Key
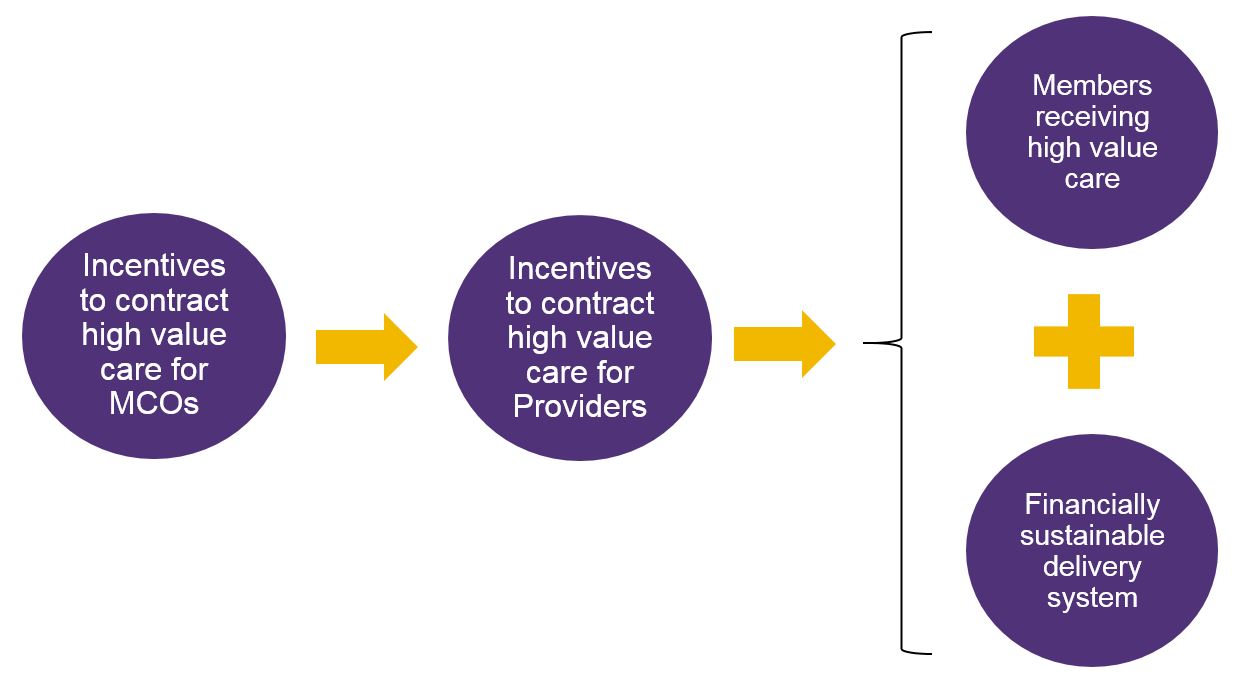
Alignment Will Be Implemented From 2017 Onwards
Financial Incentives for VBP Contractors and Other Providers: Shared Savings and More
- Potential for shared savings: incentives for a reduction in
net spending for a defined patient population/bundle, and
reinvestment of those savings back into the provider system - Performance adjustments for those VBP contractors that are
high value performers before the contract year starts - Stimulus adjustments for those VBP contractors moving to
Level 2 or higher - All these incentives have their opposites: shared losses,
downward performance adjustments, penalties for providers
that could but are not moving to VBP
Contracting for VBP
Who Can Contract VBP?
A VBP contractor is the entity that contracts the VBP arrangement with the MCO. This can be:
- Accountable Care Organization (ACO)
- Independent Physician Association (IPA)
- Individual provider (either assuming all responsibility and upside/downside risk or subcontracting with other providers)
- Individual providers brought together by an MCO to create a VBP arrangement through individual contracts with these providers
Notes:
1 – A PPS is not a legal entity and therefore cannot be a VBP contractor. However, a PPS can form one of the entities above to be considered a VBP contractor.
2 – Facilities participating in VBP QIP can be a VBP contractor.
Components of a VBP Contract
- Measurement Period
- Targeted Medical Budget
- Services Included
- Calculations
- Savings and Losses
- Reporting
- Financial Protections
- Quality Measures
__________________________________________________________
- Measurement Period
- Annual
- Targeted Medical Budget
- Percentage of Premium
- Set dollar amount
- Medical Loss Ratio
- Risk Adjustment
- Services Included
- Calculation Determination
- Savings and Losses
- How much will the MCO and Contracting Provider share in savings and losses?
- Risk and Savings is typically shared proportionally
- Reporting
- How often will reports be generated?
- Final determination is typically 18 months after the measurement period
- What reports will be generated so the VBP Contractor can ascertain its status and have time to make adjustments in service delivery patterns?
- Will the Contracted Provider have an opportunity to object?
- How often will reports be generated?
- Financial Protections
- Letter of Credit
- Reserve Fund
- Stop Loss
- Certified Financials
- Quality Measures
- Reports
- Submission of data
- Payment
MCOs and Contractors Can Choose Different Levels of Value Based Payments
In addition to choosing which integrated services to focus on, the MCOs and contractors can choose different levels of Value Based Payments:
| Level 0 VBP | Level 1 VBP* | Level 2 VBP | Level 3 VBP (feasible after experience with Level 2; requires mature contractors) |
|---|---|---|---|
| FFS with bonus and/or withhold based on quality scores | FFS with upside-only shared savings available when outcome scores are sufficient (For PCMH/IPC, FFS may be complemented with PMPM subsidy) | FFS with risk sharing (upside available when outcome scores are sufficient) | Prospective capitation PMPM or Bundle (with outcome-based component) |
| FFS Payments | FFS Payments | FFS Payments | Prospective total budget payments |
| No Risk Sharing | ↑ Upside Risk Only | ↑↓ Upside & Downside Risk | ↑↓ Upside & Downside Risk |
*As part of their participation in VBP QIP, Facilities must reach Level 1 VBP Contracting by April 1, 2017.
|top of page|There are Numerous Options for VBP Contracting
- There is not a single path towards Value Based Payments. Rather, there are a variety of options that MCOs and providers can jointly choose from.
- Total Care for General Population (TCGP)
- Total Care for Special Needs Population
- Per integrated service for specific condition: Maternity Care bundle
- For Integrated Primary Care (IPC): includes Chronic Care bundle
- These VBP arrangements are limited to Medicaid-only members.
- Duals will be integrated in the VBP arrangements from 2017 on.
Different Types of VBP Arrangements
| Types | Total Care for General Population (TCGP) | Integrated Primary Care (IPC) | Care Bundles | Special Need Populations |
|---|---|---|---|---|
| Definition | Party(ies) contracted with the MCO assumes responsibility for the total care of its attributed population | Patient Centered Medical Home or Advanced Primary Care, includes:
|
Episodes in which all costs related to the episode across the care continuum are measured
|
Total Care for the Total Subpopulation
|
| Contracting Parties | IPA/ACO, Large Health Systems, FQHCs, and Physician Groups | IPA/ACO, Large Health Systems, FQHCs, and Physician Groups | IPA/ACO, FQHCs, Physician Groups and Hospitals | IPA/ACO, FQHCs and Physician Groups |
Contracting VBP: Top 4 Steps for Beginners
| 1 | Assess your readiness; address issues to be able to start at Level 1 |
| 2 | Understand what types of contracts you want to engage in based on the services you provide, the attributed population and outcome measures that impact savings, and the potential for realizing savings |
| 3 | Choose the partners that will help you succeed and that are adequate for the contracts you chose – build your partnerships |
| 4 | Familiarize yourself with and utilize available resources (data from the State, technical assistance from potential partnering contractors, etc.) |
- The first step towards VBP is a Level 1 VBP arrangement:
- No risk
- Only upsides: nothing to lose
- ...but MCO will likely retain 50% or more of the savings
- The second step towards VBP is a Level 2 VBP arrangement:
- Assuming risk
- Up– and downsides: potentially significant losses
- ...but VBP contractor receives majority of the savings
- Only in Level 2 can MCOs stop doing Utilization Review & ask for Pre-Authorizations
- Only if you commit to going to Level 2 after maximally one year after the start can you be a NYS VBP Pilot
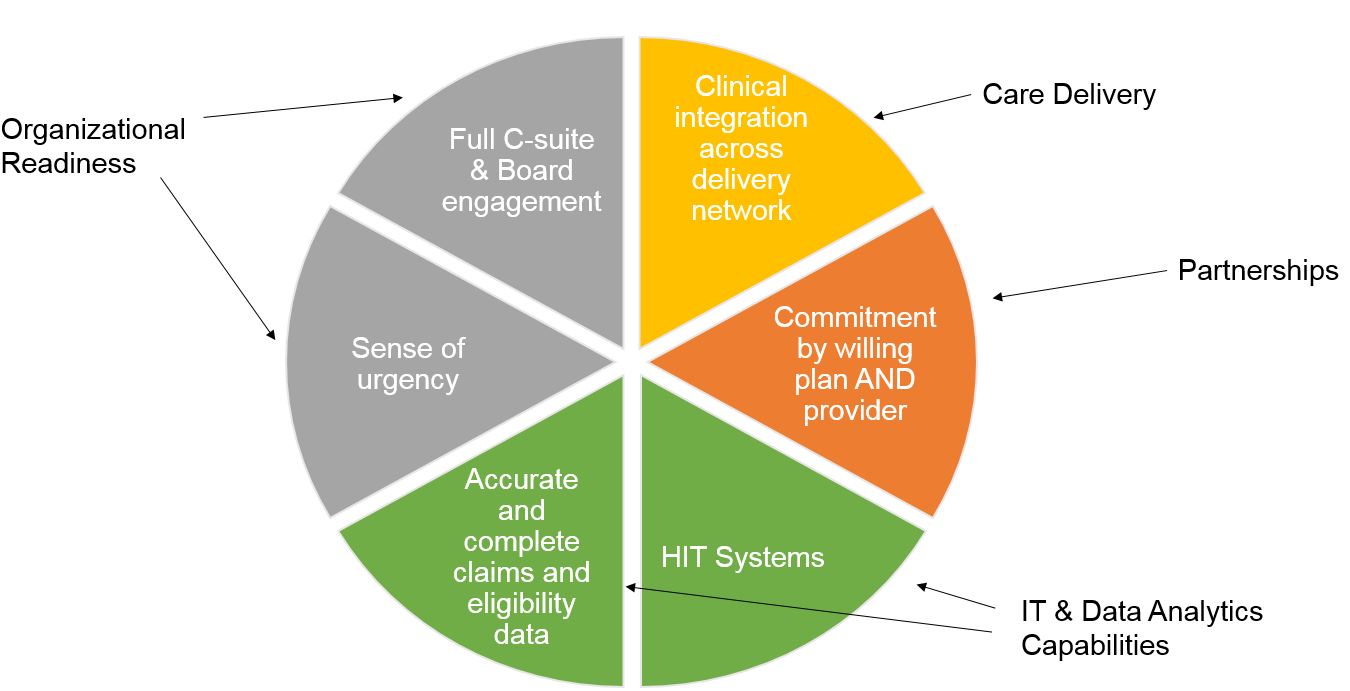
VBP Readiness Assessment

Am I ready to assume risk?
A readiness assessment is
recommended to evaluate current
state and capabilities, identify
and prioritize financial and
operational gaps. Suggested
assessment areas include but are
not limited to:
|top of page|
Care Delivery
Before entering a VBP agreement, ask:
- Especially for IPC and TCGP arrangements: are existing population health efforts adequate?
- Is clinical staffing adequate?
- Is the organization ready to engage patients?
Recommended ideal/perfect state is when you:
- Have experience managing care for groups of members and/or populations with various conditions
- Have experience managing high–utilizer/high cost members
- Have experience providing robust care coordination
- Have linguistic and cultural competency at all levels of the organization
- Have care standardization processes in place
- Demonstrate excellent chronic care management and post–discharge follow-up
- Offer integrated behavioral health and primary care services
- Have engagement, activation, and outreach strategies in place to connect with attributed population
The delivery of care model must change to satisfy requirements of payment reform
|top of page|Financial Sustainability
Before entering a VBP agreement, ask:
- Do you recognize your data; do they seem accurate and complete?
- Do you understand your part of the total cost of care / episode of care?
- Do you see ways to improve patient outcomes that would realize savings? Or realize savings while keeping care quality at the same level?
- Based on your own insights and the data, do you see opportunities to increase revenue for you and your partners through realizing shared savings, either through:
- Increasing your own efficiency
- Realizing savings downstream (i.e., outside of the group of partners you´re working with)
- What is your current financial situation?
- Would you see yourself taking risk for a specific VBP arrangement? As a lead, as a partner? Or perhaps joining a Level 2 arrangement while yourself taking minimal risk?
- Are you able to draw your own administrative and clinical data to monitor progress and outcomes of the VBP arrangement you are interested in?
VBP QIP was created to assist financially distressed organizations not only maintain operations, but move towards VBP contracting.
Recommended ideal/perfect state is when you:
- Have a clear understanding of up-front costs you will incur with implementation and an estimated return on investment
- When considering Level 2, have cash reserves on–hand appropriate to manage the relative risk of your VBP arrangement
- Have considered / included innovative ways to realize upfront investment (DSRIP, MCOs, other health care providers, banks, investors, etc.)
- Have (a clear growth path to) the ability to track and report on system–level utilization and cost data (coding accuracy is very important)
- Have a clear strategy in place for transforming your business model towards paying for value across business lines
- Have a strategy in place to coordinate the inevitably varying approaches towards VBP across payers?
- Demonstrate an understanding of the quality metrics that drive patient outcomes rather than volume
- When considering Level 2, have the ability to engage in risk–based contracts, supported by legal and compliance expertise
Organizational Readiness
Before entering a VBP agreement, ask:
- Before entering a VBP agreement, ask:
- Is the board of directors knowledgeable about payment reform efforts and their implications for the organization´s mission and services? Are they supporting the transition?
- Does the organization have the experience with and capacity to implement the organizational changes required?
Recommended ideal/perfect state is when you:
- Have a shared organizational vision for and commitment to involvement in payment reform amongst administrative and clinical leadership (from staff to C–suite level)
- Promote an overall organizational culture that prizes value and patient outcomes
- Have leadership tools and processes in place to monitor performance (robust technical infrastructure)
- Have identified specific opportunities in relation to the existing mission, service area, and scope of services
- Have change management practices in place to aid the transition
Significant organizational change must take place to accommodate payment reform. Everyone in the organization must understand what is changing and why to ensure a smooth transition
|top of page|IT & Data Analytics Capabilities
Before entering a VBP agreement, ask:
- Does the organization have an IT strategy for the transition to payment reform?
- Has a current systems hardware and software analysis been performed to ensure the organization´s IT capabilities are sufficient to participate successfully in VBP?
Recommended ideal/perfect state is when you:
- Staffed IT departments adequately and have the capacity to support payment reform efforts
- Have appropriate hardware and software systems in place with trained staff
- Demonstrate and utilize interoperability and real–time data access
- Have your Health Information Technology (HIT) reliably achieving performance targets and allowing for the continuous quality improvement (CQI), management of population/members through provider alerts, decision tools/dashboards, registries, enhanced access to data, etc.
Organizations must be able to collect and analyze large amounts of clinical and claims data to inform decisions related to VBP
|top of page|Partnerships
Before entering a VBP agreement, ask:
- Has the organization developed partnerships to address service area needs and take advantage of opportunities in the local healthcare marketplace?
- Is data sharing among partners sufficient?
- Are all contracting entities ready to participate in payment reform?
- Which providers do you want to contract with – and which not, or perhaps, later?
- How can you engage CBOs – and not because the State asks you to?
Recommended ideal/perfect state is when you:
- Have established appropriate partnerships with other providers in order to execute and meet the goals of your arrangements
- Have established relationships with social services and/or other organizations in the community in order to develop community-level systems of care
- Have begun developing new products and services in order to meet target population needs
- Have a clear understanding of the cost effectiveness and outcomes of partnership efforts
Smart partnerships between plans and providers are vital to the success of VBP
|top of page|VBP – Final Notes
We Are All in This Together
Keys to Achieving Level 1 by April 2017
Important Information
VBP Support Materials
VBP Resource Library:
- Path: DSRIP Homepage → Value Based Payment Reform → VBP Resource Library
- Link: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_library
VBP Bootcamps Website:
- Path: DSRIP Homepage → Value Based Payment Reform → VBP Bootcamps
- Link: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_bootcamp
VBP Website:
- Path: DSRIP Homepage → Value Based Payment Reform
- Link: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_reform
Final Thoughts
Next Steps and Q&A
- Group 1
- MCOs should begin planning and preparing their quarterly report, which is to be submitted in MMCOR by Tuesday, November 15th, 2016.
- Group 2
- Facilities should continue developing their VBP QIP Facility Plans for submission to their paired PPS for review.
- MCOs should continue to develop and prepare to submit their MCO Governance Documents to DOH for review.
- DOH encourages all participants to continue reviewing the NYS VBP Roadmap!
Upcoming VBP Bootcamps
| Date | Region | Session Name | Location | Time |
|---|---|---|---|---|
| Wednesday, October 19 | 5 – Long Island, Queens | Session 2: Contracting and Risk Management | Hofstra University | 9:00 am – 4:00 pm |
| Wednesday, October 26 | 5 – Long Island, Queens | Session 3: Performance Measurement | SUNY at Stony Brook | 10:30 am – 4:30 pm |
Thank you for your continued support with VBP QIP!
- The next VBP QIP Update Webinar is scheduled for Wednesday, November 16th from 2:00 pm – 3:00 pm.
- Please let DOH of any topics that you would like discussed during next month´s webinar by submitting your requested topics to the VBP QIP inbox (vbp_qip@health.ny.gov).
- The remainder of this webinar is reserved for an open forum session.
Follow Us