A Plan to Transform the Empire State's Medicaid Program
Better Care, Better Health, Lower Costs
- Final Report is also available in Portable Document Format (PDF, 2.2MB)
MULTI-YEAR ACTION PLAN
INTRODUCTION
Ever rising health care costs are a national challenge. The United States currently spends 16 percent of its GDP on health care which is nearly twice as much as any other nation. At the same time, key health indicators suggest that we are not getting our money´s worth.
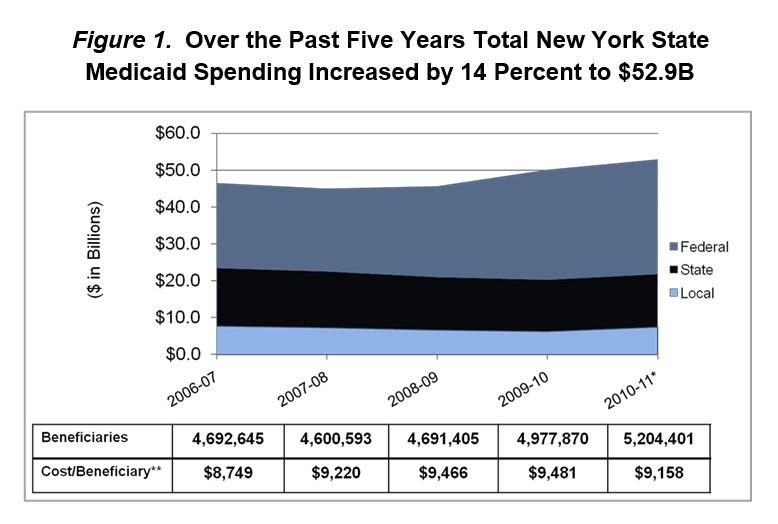
New York is a microcosm of the nation. New York´s Medicaid program, the nation´s largest, spends nearly $53 billion to serve 5 million people, which is twice the national average when compared on a per recipient basis. At best, New York is in the middle of the pack when it comes to health care quality. Similar to the nation as a whole, New York taxpayers are not getting their money´s worth when it comes to its Medicaid program.
In addition to a high spending "base", New York´s Medicaid program has seen significant growth in recent years. Some of this growth has been driven by the recession; however, other cost drivers have played a key role in program-wide spending which has risen from $46 billion in April 2007 to the current 2011 Medicaid budget of $53 billion. Upon taking office, Governor Andrew M. Cuomo identified the problem. Buried within the complexity of the Medicaid program lie numerous policies (sometimes taking the form of formulas) that have led to runaway cost growth. The Governor quickly determined that unless these underlying issues are addressed, and spending growth is contained, New York´s Medicaid program will no longer be sustainable.
In addition to a cost problem, New York has some significant quality issues. As mentioned, while national rankings tend to show New York in the middle of the pack when it comes to overall health care quality, those overall statistics mask major problems in areas such as avoidable hospital use, where New York ranks 50th in the country. Major disparities exist in health status among racial, ethnic, and socioeconomic groups in New York State. These quality issues are not limited to Medicaid but are reflected in the entirety of the health care system.
To address these underlying health care cost and quality issues, Governor Cuomo pursued a unique approach to reform. He invited key Medicaid stakeholders to the table in a spirit of collaboration to see what could be achieved collectively to change course and rein in Medicaid spending, while at the same time improving quality.
Governor Cuomo´s vision for collaboration was effectuated through Executive Order #5 which created the New York Medicaid Redesign Team (MRT). The MRT, made up initially of 27 stakeholders representing virtually every sector of the health care delivery system, including patient advocates, worked for nearly two months and developed a series of recommendations that not only lowered immediate spending - state share savings of $2.2 billion in SFY 11-12 - but also proposed important reforms that will lead to improved health outcomes, as well as further savings in years to come. The MRT continued its innovative work in a second phase, breaking into work groups to address more complex issues, as well as monitoring the implementation of key recommendations enacted from their initial work.
Perhaps the most important element of the MRT´s Phase 1 plan was to enact a global Medicaid spending cap. This cap, which applies to the state share of Medicaid spending and is under the control of the Commissioner of Health, has fundamentally changed how state officials and stakeholders view the program. Every policy change must now be viewed in terms of what, if any, impact it will have on the allocation of finite Medicaid resources. Expenditures are tracked monthly and the figures are posted to the Department of Health web site so the public can observe how the program is performing relative to the spending cap. If spending appears on path to exceed the cap, the Commissioner of Health now has "super powers" to change reimbursement rates and implement utilization controls to rein in spending.
To survive and thrive within the Medicaid budget cap, significant reform and innovation is required. New York embraces the Centers for Medicare and Medicaid Services (CMS) "triple aim" approach (as delineated herein) to health system redesign. All of the strategies identified in New York´s Medicaid redesign effort are consistent with the triple aim, and the state has developed a comprehensive set of performance measures that will allow the state to track its progress toward achieving these important goals.
New York is also well positioned to ensure that Medicaid reform also means more comprehensive health system reform. Medicaid has a large footprint in New York, especially in New York City. Changes in Medicaid payment policies have proven that they can drive broader system-wide innovations such as the statewide expansion of Patient Centered Medical Homes. New York is committed to working with other payers to drive innovation. The implementation of the health insurance exchange is just one opportunity to align health care payers to drive system-wide reform, and the state is willing to explore how best to use all the tools at its disposal to bend the overall health care cost curve, as well as improve the health of the state´s population.
Thanks to Governor Cuomo´s leadership, New York is well on its way to ensuring that the state´s Medicaid program is both successful and sustainable. However, New York needs the federal government´s help if it is to be truly successful in achieving meaningful reform. To be successful, a renewed partnership with the federal government is needed.
That´s why New York will seek to establish a new Medicaid 1115 waiver that will allow the full depth and breadth of the MRT´s recommendations to be implemented. The goals of this waiver include:
- Allowing New York to lower health care costs, improve patient outcomes and reduce health disparities by successfully implementing and maintaining the wide array of critical reforms approved by the MRT;
- Ending the state´s Medicaid fee-for-service system and replacing it with a comprehensive, high-quality and integrated care management system that will lower costs and improve health outcomes, and
- Implementing the program changes called for in the Affordable Care Act (ACA) quickly and efficiently.
While this action plan is not intended to fully capture the Medicaid Redesign Team´s in-depth discussions, the work group reports included in the companion document to this report highlight the work group´s intentions and recommended guidelines for the work going forward.
The staff of the Department of Health has worked to draw the work group recommendations together in this report, to detail an action plan that is truly comprehensive and consistent with the MRT work group recommendations. This multi-year action plan combines Phase 1 and Phase 2 recommendations and translates those into a path for the future of Medicaid in New York.
The state recognizes that as sweeping as these Medicaid program changes are, we maintain an obligation to make certain that individuals enrolled in the Medicaid program do not fall through the cracks. Community education will be paramount in assisting members understand how these programmatic changes will affect them.
New York is poised to fundamentally transform its Medicaid program into a national model for cost- effective health care delivery. Thanks to the work of the Medicaid Redesign Team the State of New York now has a multi-year road map that points the way toward a program and system that are affordable and produce good outcomes for all New Yorkers. Now it is up to the state, stakeholders and the broader New York community to continue to work together to successfully implement this multi- year action plan.
______________________________________________
Figure 1: Notes: *Reflects estimates that are awaiting final closeout by Division of Budget. ** Calculation does not reflect UPL and DSH Payments, which are included in 5-Year Medicaid spending totals. Source: Medicaid Spending Data - Division of Budget Final Enacted Financial Plan; Beneficiary Data - DOH /OHIP Datamart Database.
______________________________________________
Note: The work group recommendations are included in their final reports, as outlined in the companion document of this report, and all were approved by the MRT and are adopted by reference into this Action Plan.
|top of section| |table of contents|HEALTH SYSTEM REDESIGN IN NEW YORK: TRIPLE AIM
New York embraces the Centers for Medicare and Medicaid Services (CMS) vision for health care system redesign which provides a three-part aim for delivery reform:
- Improving the quality of care by focusing on safety, effectiveness, patient-centeredness, timeliness, efficiency and equity.
- Improving health by addressing root causes of poor health e.g., poor nutrition, physical inactivity, and substance use disorders.
- Reducing per capita costs.
In order for New York to ultimately control health care costs, it must ensure that better care is provided, including proven-effective prevention initiatives resulting in improvements in overall health status and reductions in health disparities. In particular, the biggest problem with the state´s health care system is that it is not successful in ensuring that complex, high-cost populations obtain the coordinated care they require.
In New York, this failure to deliver is not due to a lack of access to vital services. New York maintains one of the nation´s most comprehensive Medicaid programs and health care safety net systems. The problem, however, is that for far too many people, care is not effectively managed. Moreover, health disparities persist in New York as in other states throughout the nation. Providing Medicaid coverage to persons of color and residents of urban and rural areas contributes to reducing racial/ethnic and rural/urban health disparities. While coverage helps, additional efforts are needed if persistent disparities are to be eliminated.
This new MRT action plan will lead to reforms consistent with the triple-aim that will not only benefit the Medicaid program, but also the state´s overall health care delivery system. In New York, Medicaid reform has the potential to translate into meaningful health care reform, due to the size of the state´s Medicaid program and New York´s progressive political tradition, which can facilitate the successful replication of Medicaid initiatives in other key state-administered health care programs. In particular, a key component of New York´s vision for the health insurance exchange is to utilize the collective purchasing power of the state (Medicaid, exchange and state employees) to drive delivery system reform.
New York´s vision is to implement Medicaid system redesign and then drive successful reforms into these other programs. New York also wants to work closely with Medicare, an effort already underway from a data-sharing and planning perspective, which will further strengthen the state´s ability to drive change and will ensure that the triple-aim is achieved in a measurable way.
|top of section| |table of contents|KEY REFORM ELEMENTS: NEW YORK ACHIEVING THE TRIPLE AIM
New York´s path to achieving the triple-aim began with the work of the Medicaid Redesign Team. MRT Phase 1 led to the development of 78 distinct initiatives which are now being implemented. These initiatives were a mix of traditional cost containment ideas (rate reductions, utilization controls), systemic reforms and traditional public health interventions.
MRT Phase 2 generated additional proposals that both transcend the earlier work by addressing complex topics set aside in Phase 1, and help provide clarity to certain key Phase 1 reforms. This MRT action plan is built upon these recommendations and "connects the dots" to ensure that the state´s plan is a comprehensive approach to redesign and will collectively achieve the triple-aim.
Outlined in this report are the key initiatives in the plan. It should be noted that these initiatives are not necessarily mutually exclusive. There is overlap relative to their potential for enhancing quality, improving beneficiary outcomes and increasing the value of care. Some initiatives will require new investments while others will require the waiving of certain federal requirements in order to be fully enacted. The Department of Health will continue to revise the strategies identified in the plan over time to ensure effectiveness.
The reform proposals are arranged by the specific aim they best help New York achieve. While over time strategies may change New York´s commitment to improving care, improving health and controlling costs will remain. The reform proposals identified in this plan make significant strides toward these important goals, however, the state remains open to other strategies that will bolster its efforts.
|top of section| |table of contents|AIM #1: IMPROVING CARE
New York´s path to achieving the triple-aim began with the work of the Medicaid Redesign Team. MRT Phase 1 led to the development of 78 distinct initiatives which are now being implemented. These initiatives were a mix of traditional cost containment ideas (rate reductions, utilization controls), systemic reforms and traditional public health interventions.
MRT Phase 2 generated additional proposals that both transcend the earlier work by addressing complex topics set aside in Phase 1, and help provide clarity to certain key Phase 1 reforms. This MRT action plan is built upon these recommendations and "connects the dots" to ensure that the state´s plan is a comprehensive approach to redesign and will collectively achieve the triple-aim.
Outlined in this report are the key initiatives in the plan. It should be noted that these initiatives are not necessarily mutually exclusive. There is overlap relative to their potential for enhancing quality, improving beneficiary outcomes and increasing the value of care. Some initiatives will require new investments while others will require the waiving of certain federal requirements in order to be fully enacted. The Department of Health will continue to revise the strategies identified in the plan over time to ensure effectiveness.
The reform proposals are arranged by the specific aim they best help New York achieve. While over time strategies may change New York´s commitment to improving care, improving health and controlling costs will remain. The reform proposals identified in this plan make significant strides toward these important goals, however, the state remains open to other strategies that will bolster its efforts.
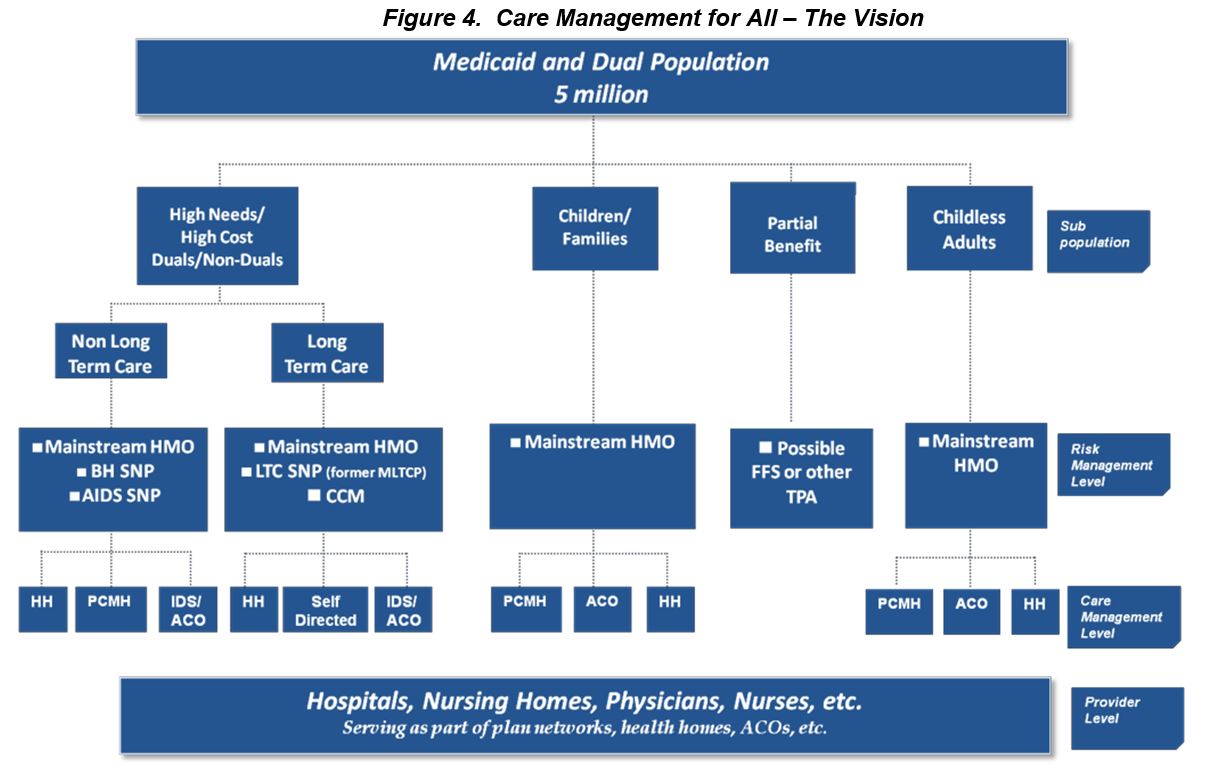
New York is committed to ensuring that every Medicaid member has access to high quality, cost-effective health care that is effectively managed. Care management for all was a key component of the MRT´s recommendations and the state is now on a path to eliminate the uncoordinated fee-for-service (FFS) payment system within three years. Replacing FFS with high-quality care management is New York´s primary strategy to achieve Aim #1.
New York has a number of care management strategies currently in place and has plans to enact even more. The state´s challenge will be to weave together these various strategies into an effective care management plan that covers the entire state and all appropriate populations. New York´s care management approach is not "one-size-fits-all" and "big insurance company for all." New York´s vision is that care management services will be delivered in a coordinated fashion by both providers and health plans. A key element of New York´s approach will be to integrate patient centered medical homes, health plans (including Special Needs Plans), and the latest innovation -- health homes, into a single system of effective care management.
New York´s long term goal is to ensure that every Medicaid member has access to fully-integrated care management. This means that health plans and their network partners will need to manage the complete health, long term care, behavioral health and social needs of the populations they serve. It may take up to five years for plan partners to evolve and develop comprehensive, high-quality networks that are sufficient to meet the unique needs of all members.
Care Management for All
Figure 2: Care Management for All Evolution Cycle
| Step 1 | Move all member and services into care management | Years 1-3 |
| Step 2 | Expandfully-integrated options | Years 1-3 |
| Step 3 | Enroll all members into fully-integrated plans | Years 3-5 |
| GOAL All members enroll in high-quality, fully-integrated care management plans in five years |
||
The MRT has set New York on a multi- year path to "care management for all." Care management for all is not simply traditional mandatory managed care in which states rely solely on insurance companies. New York´s vision is that virtually every member of the program will be enrolled in some kind of care management organization. Some care management organizations will be traditional insurance companies, while others will be provider-based plans uniquely designed to meet the needs of special populations.
New York sees full capitation as its preferred financial arrangement, but is open to other financing systems, especially for special populations. New York also acknowledges that a period of transition is necessary to achieve its ultimate goal of fully-integrated care management for virtually the entire Medicaid population.
Fully-integrated means that a single care management organization would be responsible for managing the complete needs of a member (acute, long term and behavioral care). It may take time to reach this final destination (more than three years) and existing care management organizations will need to evolve while new organizations will need to be created. In the interim, New York will use a wide range of care management tools including behavioral health organizations, existing health plans, managed long term care plans and special needs plans to ensure it reaches its initial goal of ending FFS Medicaid in three years.
Care management for all is especially important for high needs/high cost populations, including those who suffer from mental illness and substance use disorders. Systems of care for these populations must be provided that promote health through an integrated and coordinated approach that is both effective and efficient. Currently, New York spends 56 percent of its Medicaid budget providing services to this important population (see Appendix A).
Historically, New York has relied on an often disparate network of service providers to meet the needs of the program´s most complex patients. These providers must be supported in a process of transformation to become a true coordinated "system" which provides evidence-based interventions that are proven to be effective. A number of MRT initiatives are specifically designed to assist in this transformation.
The proper alignment of Medicare and Medicaid is essential if care management for all is to be successful. Currently, there is little effective coordination between the state´s two largest health care purchasers. New York is currently working with the federal Medicare-Medicaid Coordination Office to blend Medicaid and Medicare financing streams to promote efficiency and eliminate cost-shifting, while bending the cost curve for both programs.
The dual-eligible population includes the state´s most chronically ill and costliest patients, accounting for approximately 45 percent of the state´s annual Medicaid spending (2009) and 41 percent of Medicare. Yet, many of the state´s more than 700,000 dual eligibles lack effective care coordination. The move to full integration for duals will likely begin in 2014 but the exact pace and scale of transition will be subject to federal approval and stakeholder feedback.
An important interim care management strategy is the move to mandatory managed long term care for duals. In MRT Phase 2 a work group focused on developing a list of "guiding principles" for successful implementation of this important initiative. Non-institutional FFS long term care has been a major cost driver in Medicaid. Over the last five years these program costs have doubled while the number of people served has declined. At the same time per member, per month costs for managed long term care have been flat. Reform is clearly needed.
While mandatory managed long term care is now the law in New York, the Department of Health was charged with developing specific guidance for what types of "care coordination models" would meet the state´s standards. The MRT work group´s guiding principles have served as the basis for the development of the Care Coordination Models (CCM) guidance, which has been released. Figure 3 summarizes the guiding principles which will provide the state with clear direction on how to effectively implement this important part of care management for all.
A remaining challenge facing New York in its quest for full-integration will be how to ensure behavioral health services are effectively provided. While Special Needs Plans for individuals with significant behavioral health challenges will be one strategy, New York will also look at options that integrate behavioral health organizations with other care management organizations that ensure continuity, as well as prevent the "medical model" of care from displacing community-based behavioral health service delivery. Fully-integrated care management for all must mean expanded access to evidence-based behavioral health services.
Effective care management is essential to health care reform. New York stands ready to implement both short- and long-term strategies with the eventual goal of full integration, which if successful, could be a national model for how to lower costs for both of America´s major health care entitlement programs.
Figure 3: The Guiding Principles
| Principle #1 A CCM must provide or contract for all Medicaid long term care services in the benefit package. CCM will be at risk for the services in the benefit package and rates will be risk adjusted to reflect the population served. |
| Principle #2 A CCM must include a person-centered care management function that is targeted to the needs of the enrolled population. |
| Principle #3 A CCM must be involved in care coordination of other services for which it is not at risk. |
| Principle #4 The member and his/her informal supports must drive the development and execution of the care plan. |
| Principle #5 Care coordination is a core CCM function. For benefit package services, CCM members will have a choice of providers. |
| Principle #6 A CCM will use a standardized assessment tool to drive care plan development. |
| Principle #7 A CCM will provide services in the most integrated setting appropriate to the needs of qualified members with disabilities. |
| Principle #8 A CCM will be evaluated to determine the extent to which it has achieved anticipated goals and outcomes and to drive quality improvement and payment. |
| Principle #9 Existing member rights and protections will be preserved. |
| Principle #10 A CCM with demonstrated expertise will be able to serve specified population(s). |
| Principle #11 Mandatory enrollment into CCMs in any county will not begin until and unless there is adequate capacity and choice for consumers and opportunity for appropriate transition of the existing service system in the county. |
| Principle #12 Members shall have continuity of care as they transition from other programs. |
| Principle #13 Prospective members will receive sufficient objective information and counseling about their choices before enrolling. |
Ensure Universal Access to High Quality Primary Care
New York envisions a health care delivery system in which every Medicaid recipient has access to, and appropriately utilizes, high-quality patient-centered primary care. To achieve the triple-aim, New York needs to move individuals, services and resources from avoidable institutional care to community and outpatient-based care. High quality primary care is essential if New York is going to effectively rebalance its health care delivery system.
In New York, an important component to creating high quality primary care is achieved by promoting advanced Patient-Centered Medical Homes (PCMHs). Currently, 1.4 million Medicaid recipients utilize primary care from a National Committee for Quality Assurance (NCQA) recognized medical home, most of them at Level 2 or 3 (the highest level). This achievement was made possible since the state invested money in care management payments for those primary care clinicians and practices that met the standard. New York will further expand its efforts as a result of the MRT. The current plan is to expand access to PCMHs to all Medicaid recipients over the next several years.
New York is clearly a national leader in PCMHs. Despite that fact, New York needs assistance from the federal government to achieve its vision of every Medicaid member having access to, and fully taking advantage of, a Level 3 PCMH. To attain this goal, New York must accomplish four things:
- Maintain and expand the current Medicaid incentive payment for achieving PCMH recognition, while promoting transformation to Level 3 along with highest levels of care integration and health information exchange.
- Eliminate barriers to Level 3 recognition for all types of eligible providers through technical assistance and grants, so they can implement systems/processes necessary to reach Level 3; have tools and support to continue to improve the delivery of care and be able to meaningfully participate in care integration activities with other providers, in other settings across the community including, but not limited to, health homes and accountable care organizations.
- Recruit and retain more primary care physicians and nurse practitioners, especially access challenged regions of New York including but not limited to rural areas.
- Expand the "physical plant" of primary care providers such as Federally Qualified Health Centers (FQHCs) and rural clinics.
Together these strategies will not only expand access to high quality primary care within Medicaid, but there will be an additive impact across the entire health care delivery system. New York envisions a world in which state employee plans, exchange plans and other commercial plans also adopt Medicaid reimbursement strategies for PCMHs and as a result virtually all primary care providers are Level 3 PCMHs within five to seven years.
|top of section| |table of contents|Health Homes
The Affordable Care Act (ACA) has created new opportunities for states to effectively manage the health, behavioral health and long term care needs of complex, high-cost populations. New York views one new ACA tool "health homes" as the care coordination vehicle for many of the state´s most challenging populations including dually eligible members.
New York´s vision for health homes relies on a wide array of current providers forming new partnerships and stretching their list of services in ways that ensure recipients with complex health issues are effectively managed. New York has significant experience and infrastructure upon which to draw for this broad initiative. It includes a large number of PCMHs, lessons from demonstrations in chronic illness management within FFS Medicaid, large investments in Health Information Technology (HIT) and Health Information Exchange (HIE) and the experience from our HIV Special Needs Plans.
Health homes will be led by providers, health plans and even community-based organizations. Health homes will be integrated into current managed care provider networks and will be a permanent fixture of the state´s care management for all strategy. Health home networks will always include community- based organizations because they are uniquely positioned to meet the social needs of patients that often transcend health care needs.
The challenge to health homes will be to break down traditional "silos" and create partnerships that ensure that New York´s rigorous health home standards are met and that care is coordinated for New York´s most vulnerable populations.
| ISSUE SPOTLIGHT #1 FITTING THE PIECES TOGETHER: Care Management, PCMH and Health Homes |
|---|
| New York envisions a health care delivery system in which incentives align to reward quality and cost-effectiveness over volume and poor patient outcomes. No longer can New York continue to support a system in which a doctor, hospital or nursing home is financially "punished" when a patient gets well and needs less care. To align incentives to reward quality and lower costs, the state is focused on creating "integrated care" in which providers and health plans are rewarded for better patient outcomes. Integration must occur at the "risk level, "care management level," and the "provider level." New York hopes to enroll all Medicaid patients in fully-integrated health plans within five years. While an important step, this alone will not align the incentives to reward quality. Integration must also occur at the care management and provider level. Providers must be rewarded to work together to meet the complete needs of patients, especially for those patients with significant needs that cut across health care silos. Care management integration will be achieved by health homes, PCMH´s and, in some cases, health plans and ACOs. Health Homes and PCMH´s will continue to be vital state strategies even when all members are enrolled in fully-integrated care management plan. New York needs integration and incentive alignment at both the plan and provider levels in order to be successful. |
______________________________________________
1 A November 2009 report prepared by the Lewin Group found that using this model dramatically lowered inpatient costs by as much as 52 percent. The rate of hospital admissions for SNP members also decreased by 22-27 percent and the average length of stay per admission was lowered by 11 - 16 percent. Report available here. Evaluation of New York´s HIV Special Needs Plan Program: Cost and Usage Impacts. Prepared by The Lewin Group in collaboration with the AIDS Institute, NYSDOH. Authors include Franklin Laufer (New York State Department of Health AIDS Institute) and Joel Menges, Maik Schutze and David Zhang (The Lewin Group).
Another key challenge to health homes will be the implementation of Health Information Technology (HIT) and Health Information Exchange (HIE). New York plans to support health homes so they can build their capacity to communicate electronically. New York currently has a statewide network of functioning Regional Health Information Organizations (RHIOs) upon which to begin this work.
The goal is that every health home will eventually have a method to electronically share vital information (including care plans) among contracted providers, in real time. To achieve this vision, New York will likely need resources from the federal government. While the ACA provides enhanced federal funding to begin health homes, this funding is time limited. New York will look to the waiver to provide additional funding for this new initiative.
As mentioned, New York sees health homes as an essential part of the care management for all strategy. Health homes will act as providers administering a benefit within a care management network. Care management organizations will be required by contract to connect challenged populations with health homes that are certified by the state (unless the health plan serves as the health home.)
Thanks to Health Homes, New York is poised to redesign the manner in which Medicaid´s most challenged patients´ access health care services. This redesign will lead to both better patient outcomes and lower costs.
|top of section| |table of contents|Health Care Workforce for the 21st Century
The ACA will add hundreds of thousands of new beneficiaries to the New York Medicaid program, and many more to the ranks of the privately insured. This will require delivery system restructuring and expansion, including training additional providers and workers and retraining clinical and non-clinical workers to focus on chronic disease management and care coordination.
To help address the health care workforce challenges of the 21st Century, a special MRT work group was established. This group, comprised of a wide array of stakeholders, met multiple times and attempted to achieve consensus on challenging issues such as scope of practice. MRT Phase 1 initially included scope of practice changes but those changes were not approved by the legislature.
The Workforce MRT work group overwhelmingly approved a series of sweeping recommendations which, if adopted, could substantially recalibrate the health care workforce and lead to more cost-effective care. A key theme resulting from the work group recommendations was the need to ensure that mid-level providers were allowed to work "at the top of their licenses." In particular, the work group made a series of important recommendations to expand the scope of practice for certified nurse practitioners, dental hygienists, home care aides and advanced aides.
The work group also recommended the creation of a new Advisory Committee, which would assist the Office of the Professions within State Department of Education with assessments of proposals designed to improve health workforce flexibility in New York. The hope is this group will allow New York to break-out of the traditional professional silos, and utilize medical evidence and independent research to inform scope of practice decision-making.
While some stakeholders remain concerned about certain provisions, the state will work with the broader health care community, legislature and the State Department of Education to implement them in cost-effective ways.
|top of section| |table of contents|HIT - Interoperable EHR for All New Yorkers
In order for Medicaid redesign to be successful, New York must find a better way to coordinate and manage care for high needs/high cost patients. To effectively coordinate care, a wide array of providers and plans must be able to effectively communicate. Universal provider-to-provider communication is only possible if we can develop an interoperable HIT system, through which providers can share vital information about patients in ways that protect patient confidentiality and do not add extra burdens to providers. While the MRT did not have a specific work group dedicated to HIT, many of the MRT initiatives are dependent upon a high functioning HIT system in New York.
Strategic investments, coordinated with existing state and federal initiatives targeted at HIT adoption and use, will help lead to a statewide HIT infrastructure that will allow patient records to be shared. This will reduce redundant tests and help contain costs by enabling providers to better track the care given to patients. New York envisions a health care delivery system in which every provider has access to the vital patient information they need to effectively provide and manage care. New York has made progress in this area, but additional investments will help ensure that by the end of the decade every New Yorker will benefit from a statewide, interoperable EHR system.
New York State has already made an unprecedented commitment to advance broad HIT adoption and use. Since 2006, the state has invested more than $400 million in combined state and federal dollars to establish policies and technical services to facilitate health information exchange, as well as increase the number and success of physicians utilizing EHRs. Additional federal support for these objectives has come through three initiatives: EHR incentive payments for eligible professionals and hospitals serving a significant volume of Medicare and/or Medicaid beneficiaries; the award of contracts to the New York eHealth Collaborative to administer the State HIE Cooperative Grant Program and the statewide Regional Extension Center (REC) program (outside New York City); as well as the REC contract award to NYC Regional Electronic Adoption Center for Health (REACH).
The combined NYC REACH goal is to implement EHRs and support 10,000 physicians to achieve meaningful use and qualify for the incentive payments.
Despite these investments, we recognize that there are significant gaps in health IT capabilities which will be necessary to achieve the ambitious Medicaid reforms New York envisions. The need for additional resources and assistance can be broken into four categories: (1) eligible professionals (EPs) and hospitals that may qualify for Medicaid utilization but are not served by the REC program because of limited resources or categorical restrictions; (2) professionals and hospitals that would otherwise meet the definition of EPs and hospitals, and serve large numbers of Medicaid beneficiaries, but do not hit the 30 percent patient volume threshold; (3) additional health care providers - mental health, long term care and substance use disorders, for example - who were not included in the Meaningful Use (MU) incentive program and are actively involved in Health Homes; and (4) other categories of providers (e.g., Health Home Case Managers) who need to access information through HIE but may not have or need full EHR capabilities.
Additional work is needed to quantify the implementation gap and define specific priorities to advance the state´s health reform goals. At this time, the state does not have a reliable estimate of the total number of Medicaid providers who lack EHRs. The state will need to develop criteria to prioritize these needs in the context of broader MRT programmatic objectives, including the implementation of Health Homes. Fortunately, the state has an extensive tool kit for implementation support and local and statewide organizations that are experienced in managing and providing these services.
New York commits to completing this analysis and developing a specific proposal for the number of providers, the package of technical assistance services and the dollars necessary to advance broad HIT adoption and use in support of Medicaid redesign and broader health care transformation.
|top of section| |table of contents|Improving Behavioral Health
New York´s behavioral health system (which provides specialty care and treatment for mental health and substance use disorders) is large and fragmented. The publicly funded mental health system alone serves over 600,000 people and accounts for about $7 billion in annual expenditures. Approximately 50 percent of this spending goes to inpatient care. The publicly funded substance use disorder treatment system serves over 250,000 individuals and accounts for about $1.7 billion in expenditures annually. Despite the significant spending on behavioral health care, the system offers little comprehensive care coordination even to the highest-need individuals, and there is little accountability for the provision of quality care and for improved outcomes for patients/consumers. This fragmentation problem is compounded since mental health and substance use care and treatment systems are separated, with discrete regulations and funding streams, though there are substantial rates of people with co-occurring serious mental illness and substance use disorders.
Behavioral health also is not well integrated or effectively coordinated with physical health care at the clinical level or at the regulatory and financing levels. The behavioral health system is currently funded primarily through fee-for-service Medicaid, while a substantial portion of physical health care for people with mental illness or substance use disorders is financed and arranged through Medicaid managed care plans. This also contributes to fragmentation and lack of accountability. This lack of coordination extends well beyond physical health care into the education, child welfare, and juvenile justice systems for those under the age of twenty-one.
The fragmented and uncoordinated payment and delivery systems have contributed to poor outcomes, including:
- People with serious mental illness die 15-25 years earlier on average than the rest of the population. The leading contributors to this disparity are chronic, co-occurring physical illnesses, which are not prevented and are treated inadequately. (Congruencies in Increased Mortality Rates, Years of Potential Life Lost, and Causes of Death among Public Mental Health Clients in Eight States http://www.cdc.gov/pcd/issues/2006/apr/05_0180.htm).
- The majority of preventable admissions paid for by fee-for-service Medicaid to Article 28 inpatient beds are for people with behavioral health conditions, yet the majority of expenditures for these people are for chronic physical health conditions.
- There is an over-reliance on State psychiatric hospitals, adult homes and nursing homes, partly due to the system´s inability to assign responsibility for integrated community care.
- In New York State, under the current Medicaid fee-for-service system, 20% of patients discharged from psychiatric inpatient units are readmitted within 30 days. (http://www.omh.ny.gov/omhweb/rfp/2011/bho/databook_tables.xlsx)
To address the problems in New York´s behavioral health system, a specific MRT work group was established. This work group, which brought together a wide array of stakeholders, developed comprehensive recommendations, and a reform agenda that is a key part of the overall MRT action plan.
First and foremost, the work group embraced the concept of effective care management for patients with serious mental illness and substance use disorders. The work group went beyond simply advocating for care management, and actually identified a number of key elements of design and practice needed for a managed and coordinated behavioral health care system in New York relevant across the age span. Savings on behavioral and physical healthcare attributable to improved care coordination should be focused on high priority areas including housing, employment services, peer services and family support. The work group reached consensus on key principles and identified critical metrics and indicators that should be measured to determine the extent to which the principles are met. The guiding principles can be found in Appendix B of this document.
One of the key recommendations of the work group is to establish Special Needs Plans and Integrated Delivery System models for providing fully-integrated care management for patients with significant behavioral health needs. These organizations would be risk-bearing and manage the comprehensive needs of the patients they serve. In addition this work group strongly supported the MRT recommendation of a Behavioral Health Organization option which would be a carved-out service that works in tandem with a health plan to achieve service integration. This recommendation is entirely consistent with the overall MRT theme of care management for all and creates a new model of integration that is highly specialized to an important sub-population.
The work group also provided specific recommendation for how to effectively implement Behavioral Health Organizations as an initial step to effective care management, as more comprehensive care management models are allowed to develop. BHOs were a key MRT Phase 1 initiative and are already being implemented. BHOs have proven effective at managing behavioral health services in other states, and will begin by managing high cost FFS behavioral health services through a concurrent review process for FFS inpatient care and a focus on high-quality engagement post discharge. Eventually BHOs will bear risk, and the work group provided very specific recommendations for how to ensure they are effective.
This work group also discussed the need for integration of behavioral health into primary care settings covered under mainstream plans. Collaborative care and a more robust set of behavioral performance measures were recommended for mainstream plans. A mechanism for funding an appropriate level of services to the uninsured and underinsured needs to be maintained as the system moves into managed Medicaid for all clients with mental health and substance use disorders, and previous funding streams (such as disproportionate share hospital (DSH) payments) are reduced or no longer available.
The work group also created a special team that focused on the behavioral health needs of children. The team provided recommendations on how the state should step up enforcement of health plans to ensure children with behavioral health needs get the services they need, as well as specific outcome measures the state should track to ensure that children are appropriately served.
Finally, the work group also provided recommendations on how to expand access to peer services, and provided the state with further guidance on how to effectively implement health homes. The work group´s full recommendations, which can be found in the companion document of this report, are perhaps the most comprehensive roadmap New York has ever had for creating an effective behavioral system that is efficiently integrated with other health sectors in order to ensure that the complete needs of complex patients are addressed.
|top of section||top of section - Aim #1| |table of contents|
AIM #2: IMPROVING HEALTH
Medicaid reform in New York State must be about improving population health. Historically, Medicaid reform has often focused on lowering costs for taxpayers or improving health care quality measures. New York wants to "break the mold" and look to use the Medicaid program to drive deeper and more lasting change. In addition, New York wants to bring a whole new group of social entrepreneurs to the table to assist the state in managing complex populations through a mix of services that transcend the traditional Medicaid offerings.
Medicaid, as the largest insurer in the State of New York, has a vested interest in addressing preventable conditions and promoting health to ensure a healthy and productive populace and to reduce expenditures. While Medicaid has traditionally been viewed solely as an insurer of low-income and vulnerable populations, the program´s coverage of essential public health services and financing of public hospitals and clinics improves the health status and outcomes of program beneficiaries and the population as a whole.
New York must implement powerful new health and public health strategies to eliminate health disparities, significantly expand access to supportive housing, and re-invent the Medicaid benefit to improve population health. New York´s approach to improving population health is built on its years of experience in other areas, such as the fight against AIDS. By utilizing lessons learned from other efforts, as well as bringing to scale successful pilot efforts, New York will be uniquely poised to lead the nation in improving overall population health.
| 2009 Commonwealth New York State Scorecard on Health System Performance | |
|---|---|
| Care Measure | National Ranking |
| Percentage of Uninsured Adults | 28th |
| Quality of Health Care | 22nd |
| Public Health Indicators | 17th |
| Avoidable Hospital Use and Cost | 50th |
Eliminating Health Disparities
Medicaid reform must be about more than health care system redesign and payment reform. Medicaid reform - and broader reform of the entire New York health system - must also be about improving overall population health. Throughout New York´s history, the state has been a national leader in advancing important public health causes. New York must reclaim its role as a national leader in population health management.
Perhaps the most pressing population health problem facing New York is the ever present reality that significant disparities in health outcomes exist in our state. To address these concerns an MRT work group was established to develop specific recommendations for how to reduce or eliminate disparities based on race, ethnicity, gender, age, physical or psychiatric disability, sexual orientation and gender expression.
This work group experienced some challenges when it came to defining its scope and focus. Disparities are caused by a wide array of complex factors and possible solutions cut across traditional health care silos. The work group reviewed a substantial amount of data and considered 69 specific proposals before agreeing on 14 priority recommendations which were included in their work group report. These recommendations are provided below:
- Data Collection/Metrics to Measure Disparities: New York should implement and expand on data collection standards required by Section 4302 of the Affordable Care Act by including detailed reporting on race and ethnicity, gender identity, the six disability questions used in the 2011 American Community Survey (ACS), and housing status. In addition, funding should be provided to support data analyses and research to the state´s work with internal and external partners to promote programs and policies that address health disparities, improve quality and promote appropriate and effective utilization of services including the integration and analysis of data to better identify, understand and address health disparities.
- Improve Language Access to Address Disparities: Medical Assistance rates of payment for hospital inpatient and outpatient departments, hospital emergency Departments, diagnostic & treatment centers, and federally-qualified health centers should provide reimbursement for the costs of interpretation services for patients with limited English proficiency (LEP) and communication services for people who are deaf and hard of hearing.
- Promote Language Accessible Prescriptions: Actions should be taken to require all chain pharmacies to provide translation and interpretation services for limited English proficient (LEP) patients, that standardized prescription labels be required to ensure understanding and comprehension especially by LEP individuals and that prescription pads be modified to allow prescribers to indicate if a patient is LEP, and if so, to note their preferred language.
- Promote Population Health through Medicaid Coverage of Primary and Secondary Community-Based Chronic Disease Preventive Services: Medicaid should be expanded to include coverage of Pre-Diabetes group and individual counseling services (fee-for-service and managed care); lead poisoning, asthma, home visits and automated home blood pressure monitors for patients with uncontrolled hypertension.
- Streamline and Improve Access to Emergency Medicaid: The state should take actions to increase awareness about emergency Medicaid among consumers, providers, and local Social Services districts, streamline the application process through prequalification and extend certification periods for certain medical conditions to enable providers to receive appropriate reimbursement from federal funds and reduce hospital and institutional reliance on state charity care dollars.
- Address Disparities in Treatment at Teaching Facilities: Actions should be taken to ensure that existing standards of care are enforced in teaching hospitals and training clinics to ensure that the care provided to persons who are uninsured, to people covered by Medicaid, and to the privately insured is consistent and is of the highest quality and equivalent to those services provided by the private faculty practices in the same institutions.
- Address Disparities Through Targeted Training for NYS´ Health Care Workforce: Cultural competency training should be required to promote care and reduce disparities for all individuals including but not limited to people with disabilities, Lesbian, Gay, Bisexual and Transgender persons, persons with mental illness, substance use disorders and persons at risk of suicide.
- Enhance Services to Promote Maternal and Child Health: The following Medicaid enhancements and expansions should be implemented to promote maternal and child health: Expanded access to contraception and other family planning services including inter- conceptional care following an adverse pregnancy; breastfeeding education and lactation counseling during pregnancy and in the postpartum period; and support of initiatives to demonstrate effective and efficient use of HIT technology between hospitals/health care systems and community-based health organizations to improve care delivery.
- Enhanced Services for Youth in Transition with Psychiatric Disabilities: Comprehensive programs to serve youth in transition with psychiatric disabilities should be developed across all systems of care including foster care, school populations that have youth with a serious emotional disorder diagnosis and the juvenile justice population to ensure that youth with psychiatric disabilities do not end up homeless or in the criminal justice system.
- Promote Effective Use of Indigent Care Funds: The charity care reimbursement system should be revised to ensure that indigent care funding is transparent, is used to pay for the care of the uninsured and that there is greater accountability for use of these funds.
- Promote Hepatitis C Care and Treatment through Service Integration: Efforts should be taken to promote the integration of hepatitis care, treatment and supportive services into primary care settings including community health centers, HIV primary care clinics and substance use treatment programs.
- Promote Full Access to Medicaid Mental Health Medications: Actions should be taken to ensure that all Medicaid recipients who are in managed care plans where the pharmacy benefit is no longer carved out continue to have full access to mental health medications.
- Medicaid Coverage of Water Fluoridation: To address disparities in access to dental services, Medicaid funding should be made available to support costs of fluoridation equipment, supplies and staff time for public water systems in population centers (population over 50,000) where the majority of Medicaid eligible children reside.
- Medicaid Coverage of Syringe Access and Harm Reduction Activities: Actions should be taken to promote and address health care needs of persons with chemical dependency including allowing medical providers to prescribe syringes to prevent disease transmission; and by authorizing NYS DOH AIDS Institute Syringe Exchange providers to be reimbursed by Medicaid for harm reduction/syringe exchange program services provided to Medicaid eligible individuals.
These recommendations cut across the entire health care delivery system and show just how broad a look the work group took at the causes of health disparities. Some of these initiatives were approved as part of the 2012-13 state budget, however, to fully implement these recommendations new funding sources will be necessary. One possible source of funding is the new MRT waiver which the state will pursue in 2012. The hope is that all of these recommendations will be implemented, within existing financial constraints, over the next three to five years.
______________________________________________
Note: All MRT initiatives were evaluated for their impact on health disparities, as recommended by the Health Disparities work group.
|top of section| |table of contents|Affordable and Supportive Housing
The Medicaid Redesign Team identified early on in its deliberations that increasing the availability of affordable and supportive housing for high-need Medicaid beneficiaries who are homeless, precariously housed or living in institutional settings is a significant opportunity for reducing Medicaid cost growth.
There is strong and growing evidence in New York and around the country that a lack of stable housing results in unnecessary Medicaid spending --on individuals in nursing homes and hospitals who cannot be discharged only because they lack a place to live, and on repeated emergency department visits and inpatient admissions for individuals whose chronic conditions cannot be adequately managed on the streets or in shelters. The lack of appropriate affordable housing, especially in New York´s urban areas, may be a major driver of unnecessary Medicaid spending.
In New York City, for example, among Medicaid beneficiaries with expected high future costs identified for participation in the Chronic Illness Demonstration Project, up to 30 percent were homeless and even more were precariously housed or living in transitional settings. New York has an impressive record of making investments in supportive housing, both in the mental hygiene system and for frail elders. These investments have helped stabilize thousands of high-risk New Yorkers with complicated medical, long term care, mental health and substance use disorder needs. Thanks to the MRT, the state is taking a new look at how housing can lead to a reduction in overall Medicaid spending. In fact, an ongoing annual appropriation of $75 million has been pledged in the NYS financial plan as part of MRT Phase I.
In addition, an MRT work group was established to see what more could be done to expand access to affordable/supportive housing for Medicaid members. This work group was made up of a diverse set of stakeholders, including some of the largest operators of supportive housing in New York. Their final report included seven proposals for investments in new affordable housing capacity, as well as five "collaboration/coordination" recommendations which are designed to ensure that various state and local agencies (both governmental and non-profit) are working together to maximize the value of all affordable housing programs.
Also, the work group provided a series of recommendations for how the state could expand access to the Assisted Living Program. Assisted living is often a lower cost and more appropriate living arrangement for individuals. Unfortunately, the regulations associated with the program have not kept up with changing events, which has restricted access. In addition, the program needs to modernize in order to prepare for care management for all.
New York is especially interested in using the 1115 Medicaid waiver as a funding source for a significant new investment in affordable/supportive housing specifically targeted at high needs/ high cost Medicaid members. New York hopes this investment could amount to millions of dollars per year and would allow the state to fully implement the work group recommendations.
The workgroup made numerous other recommendations about how to improve access to housing and healthcare. Examples include but are not limited to: co-locate behavioral and health services in housing, expand and improve independent senior housing, evaluate ways to create opportunities for diversion from hospitals, ensure coordination with Health Homes, streamline community siting processes, ensure the viability of existing housing resources, and design a Moving On initiative to help move individuals to more independent settings thereby freeing up needed resources for those most in need.
Affordable/supportive housing is a classic example of where the current Medicaid financing system deters states from making the kinds of investments that can truly reduce costs. New York is interested in working with the CMS to see how federal funds can help establish more supportive housing, so that Medicaid beneficiaries receive the care they need in the most cost-effective settings possible.
|top of section| |table of contents|Redesigning New York´s Medicaid Benefit
Medicaid benefits, covered services, as well as recipient cost-sharing, are rarely examined on a systematic basis. The only time such an examination occurs is during very difficult budget situations when savings are needed and the options most often considered are either benefit cuts or increases in cost-sharing.
As New York prepares for ACA implementation, the state wants to engage its stakeholder community as well as national experts in a comprehensive discussion about how the Medicaid benefit should be structured to ensure that all members have access to the clinically effective, efficiently delivered services they require. New York hopes to learn from the experiences of other states and commercial payers and implement reforms that are consistent with value-based benefit design.
To lead this comprehensive review, an MRT work group was established under the leadership of Health Commissioner, Dr. Nirav R. Shah. Dr. Shah is a nationally-recognized health sciences researcher, with substantial experience in comparative- effectiveness research. Dr. Shah co-chaired the group with Frank Branchini, a veteran health plan executive. The work group included providers and consumer advocates and proposed specific Medicaid benefit changes as well as a process for moving forward in value-based benefit design. Before launching into the consideration of specific recommendations the work group established guiding principles. These principles form the base upon which not only the work group functioned but how New York will seek to implement value-based benefit structures. The ten principles, which can be found in Appendix C, stress the importance of treating all Medicaid patients equitably while at the same time acknowledging that effective stewardship of finite public resources requires responsible use of empirical evidence regarding the benefits, harms and costs of benefits/services in making benefit design decisions.
The work group also provided a very detailed recommendation for how the Department of Health should review benefits in the future. Specifically, the work group recommended that the state create an expert advisory panel to provide guidance to the Medicaid program in regard to ongoing benefit design. This panel will include consumer/members representation to ensure that those important voices are heard.
The work group also provided clear direction on the types of analysis that should be used in making benefit decisions and the important advice that the panel focus on benefits or services that fall into the following categories:
- New technology with significant costs or utilization or health impact(s);
- Requests from outside stakeholders for changes in coverage;
- Proposed new codes for services (CPT and HCPCS);
- New federal or state statute/regulatory changes that mandate review.
In addition to the creation of a prospective review process and the establishment of an expert advisory committee, the work group also made a series of recommendations regarding specific benefit changes. These changes, which were approved in the FY 2012-13 state budget, are designed to both improve Medicaid´s cost effectiveness as well as demonstrate how medical evidence can improve benefit design. New York will seek to implement these recommendations in a cost-effective manner which ensures that they do not create any additional pressure on the state´s global spending cap.
|top of section||top of section - Aim #2| |table of contents|
AIM #3: REDUCING COSTS
Upon taking office, Governor Cuomo quickly determined that New York´s Medicaid program was no longer sustainable. New York taxpayers, while generous, had reached the point where they were no longer able to afford the ever-increasing burden the program placed on the state budget. It is for this reason that Governor Cuomo created the Medicaid Redesign Team (MRT). The MRT radically changed the Medicaid budget discussion by creating a new global Medicaid spending cap and by giving the Commissioner of Health the power to enforce that cap.
The global spending cap has changed the way the program is perceived by both state officials and stakeholders. All new expenditures must be analyzed to assess their impact on both cost and quality. This level of scrutiny is unprecedented in New York. The global spending cap means savings not only for state taxpayers, but also for the federal government. The cap represents the core of the state´s budget neutrality argument for a future 1115 Medicaid waiver.
While the implementation of the spending cap was an important first step, more needs to done if costs are to be controlled. In particular, New York must lead the nation in payment reform. While this action plan will get New York out of the Medicaid FFS business, the state must ensure that its care management partners also shift away from volume-based payments and adopt other payment systems that reward quality.
To truly lower costs and improve quality, New York must also improve the overall efficiency of its health care safety net system. New York relies on a variety of public and non-profit institutions to provide care. The safety net system must evolve and become more efficient, especially given the significant expansion in access that will come with the ACA.
Lastly, New York must obtain control over its ever-rising medical malpractice costs while at the same time balancing the needs of vulnerable patients and their families. These costs pose a significant financial challenge.
Global Medicaid Spending Cap
New York now has a statutory "global cap" on Department of Health controlled Medicaid expenditures. This cap is on the state´s share only. The cap is linked to the annual rate of growth in the 10-year rolling average in CPI-Medical. The cap can be adjusted by the state´s Division of Budget, but only under very limited circumstances. Enrollment growth due to macro-economic factors is not one of these circumstances; however, since the cap is set in state law, the Legislature could adjust the cap if New York were to face another economic crisis.
New York´s statutory cap will lead to significant federal savings. Current estimates are that over the next five years the federal government will save $18.3 billion. It is this savings which will ensure that a proposed 1115 waiver is budget neutral. In order to function within the statutory cap New York needs the other elements of its comprehensive plan to be implemented. Given New York´s size, a successful state spending cap could play a role in the nation´s overall deficit reduction efforts.
| ISSUE SPOTLIGHT #2 TRACKING SPENDING - NEW YORK´S NEW APPROACH |
|---|
| The Medicaid global spending cap has forced New York to track Medicaid expenditures more closely than ever before. Every month a global spending report is published so that the public can track performance relative to a spending target. Spending is tracked by sector and the report clarifies why spending is deviating from target. To effectively track Medicaid spending as well as to better understand what factors are driving the trend, the state has contracted with Salient, an innovative New York company. Salient provides New York with a state of the art visual data mining technology that allows analysts to drill down into data - even down to the individual patient or provider level - so as to understand what factors are driving spending. Information can be geo- mapped and outlier providers can be clearly identified for targeted interventions. Thanks to this new tool New York is well positioned to not only ensure that state taxpayers get their money´s worth when it comes to Medicaid, but to ensure that budget neutrality is maintained under a new waiver. |
Strengthening and Transforming the Health Care Safety Net
The financial performance of New York´s hospital sector remains well below the national average. In 2009, New York hospitals generated an average operating margin of 1.6 percent, significantly below the national average of 4.3 percent and the 3 percent level generally recognized as necessary to maintain infrastructure. The margin for New York´s safety net hospitals was far worse. Hospitals with Medicaid patient loads in the highest quartile ran an average operating margin of negative 1.3 percent. Maintaining a strong safety net system is absolutely critical to preserving services, including primary care services, for the Medicaid population.
In addition to providing critical inpatient acute and trauma services, New York hospitals are the major provider of primary care services to the Medicaid population, particularly in New York City. New York´s safety net institutions generally have very high Medicaid and Medicare volume and very little commercial volume. Recession-driven reductions in Medicaid reimbursement rates, along with flat Medicare reimbursement, have placed these institutions in increasingly precarious situations. Indeed, 11 hospitals have closed in New York since 2007. These institutions struggle from day-to-day to maintain basic services, and have no capacity to invest in the infrastructure necessary to implement delivery system reform.
Perhaps the most telling case study for the challenges facing New York´s health care safety net can be found in Brooklyn. A special MRT work group was established to examine the challenges facing the borough. Its specific mission was to "assess the strengths and weaknesses of Brooklyn hospitals and their future viability" and "make specific recommendations that will lead to a high-quality, financially secure and sustainable health system in Brooklyn." After months of work which included site visits, public hearings, expert testimony and extensive policy analysis, the work group determined that Brooklyn´s healthcare delivery system is at the brink of dramatic change. This change will either be characterized by a reconfiguration of services and organization to improve health and health care or by a major disruption in services as a result of the financial crises at three hospitals.
The Brooklyn work group recommended both the development and implementation of a series of "tools for change" as well as a series of hospital-specific recommendations that if implemented could effectively lead to a more stable delivery system in New York City´s largest borough.
The tools for change are provided below while the hospital specific recommendations can be found in Appendix D.
- Expand the State Health Commissioner´s Powers over Healthcare Facility Operators
- Appoint a Brooklyn Healthcare Improvement Board
- Provide Financial Support for Restructuring through an Application Process
- Rationalize the Distribution of DSH/Indigent Care Pool Funds2
- Provide funding for a Multi-Stakeholder Planning Collaborative in Brooklyn
- Support Involvement of Private Physician Practices in Integrated Health Systems
- Develop New Alternatives for Capital Support of Primary Care Providers.
While not all of these tools were approved in the most recent state budget, the Department of Health will work with Brooklyn hospitals and other community stakeholders to build off the recommendations of the MRT work group.3 The state stands ready to work with willing providers to transform the boroughs´ health care delivery system to ensure that it provides high- quality care in a cost-effective manner.
Brooklyn is not the only community facing significant health care delivery problems. New York will seek to build off the Brooklyn process to address the needs of other parts of the state. Some safety net provider funds are now available statewide, but more federal financial assistance will be necessary given the state´s limited resources. The obvious vehicle for this funding is the MRT 1115 waiver. In order to ensure that New York has a cost-effective health care safety net that is prepared to survive and thrive in a post-ACA world, additional investments will be necessary and New York believes an 1115 waiver is the tool to make those vital investments.
Finally, a major challenge facing safety net providers is the growing population of undocumented residents with significant health care needs. These individuals are not eligible for full Medicaid and are often limited to emergency room care to treat their chronic health care needs. One MRT work group, Health Disparities, recommended that Indigent Care Pool funds be re-directed to finance a primary care benefit for this population. The challenge associated with the undocumented population will be a challenge even after ACA is implemented. New York will look to work with the federal government and stakeholders to address this major cost driver.
______________________________________________
2. Three MRT work groups provided recommendations regarding possible changes to the allocation of DSH/Indigent Care Pool funds. The Department of Health is currently looking for CMS guidance on what options for changes in the programs will allow the state to more effectively protect these vital funds which are now at risk because of recent changes in federal law. 2
3. The Brooklyn work group did not report back to the full MRT but rather to the Commissioner of Health, Dr. Nirav Shah.3
Payment Reform
New York is committed to eliminating the Medicaid FFS payment system.
Specifically, New York wants to end the practice of paying for volume rather than for value. While care management for all is an important step, it does not guarantee true payment reform will occur. If the care management partners simply use FFS- like payment systems to pay providers, the misaligned incentives associated with the current system will remain.
To permanently break out of the current cycle, New York will aggressively pursue other payment models. New York currently has providers who work with health plans on a sub-capitation basis. This arrangement will be further encouraged, and the state will watch closely as Medicare and other payers pursue other innovative models.
The most commonly discussed payment reform initiative is Accountable Care Organizations (ACOs). New York and its provider community are very interested in this concept. New York has reviewed the final rules from Medicare on this topic and is prepared to work with interested providers to pursue this reform opportunity. Finally, true payment reform will only be possible if Medicare and Medicaid align their purchasing strategies. The MRT Payment Reform work group recommended that the state move forward with an innovative new partnership with the federal government under which true integration would be achieved for dual eligible members. This partnership must ensure that providers and payors realize financial savings while at the same time patient outcomes improve. New York is confident that the combined impact of payment reform, effective care management and a new state/federal partnership will lead to both lower costs and improved outcomes.
| ISSUE SPOTLIGHT #3 PAYMENT REFORM OPPORTUNITY: ADVANCED HEALTH HOME |
|---|
| New York is prepared to aggressively pursue innovative payment reform models. Additionally, New York wants to effectively coordinate its efforts with Medicare and other large payers to ensure that providers experience a consistent set of financial incentives and do not face barriers to reform and innovation. In particular, New York seeks to integrate the Health Home concept with other payment reform proposals such as Accountable Care Organizations. To this end, New York wants to work with the federal government and the provider community to pursue an "Advanced Health Home" concept that would merge the best features of the New York´s upcoming health home initiative with the accountable care concept to deliver fully coordinated health care to patients. A regional and sustainable Advanced Health Home would function as a coordinated network of providers, share a common care plan that is managed by a single case manager, and report results across diverse organizational entities. Significant investment in health information technology (HIT) infrastructure, workforce development and common policies and procedures would allow for the effective integration of medical and behavioral care key to achieving savings. The Advanced Health Home would also operate under a more robust shared savings model. Reimbursement for the health home would more closely track comparable Medicare efforts, for example under the Pioneer Accountable Care Organization (ACO) model. Aligning the two programs would make it easier for capable providers to participate in both initiatives. New York would look to start its Advanced Health Home model with provider networks that participate in Medicare´s Pioneer ACO program. |
Note: The Payment Reform work group´s guiding principles are included in their final report, as outlined in the companion document to this report.
|top of section| |table of contents|Medical Malpractice Reform
Medical malpractice costs are increasingly difficult for providers to sustain in New York. The MRT took the first step in addressing this problem by creating a new one-of-a-kind Medical Indemnity Fund (MIF) which will lower insurance premium costs by financing health care services for children affected by neurological impairment that have received either a court settlement or award. It is estimated that this new initiative will lower premiums by $320 million annually. MIF is now operational and the state will closely monitor its ability to both finance health care services for vulnerable children and lower malpractice insurance premiums.
More can be done to lower malpractice premiums, as well as ensure that the quality of care is improved. To this end, the MRT created the Hospital Quality Initiative, with a specific obstetrical work group which will look to improve the effectiveness of maternity care that could translate into reduced medical malpractice and insurance premiums. In addition, a MRT Medical Malpractice Reform workgroup was convened in 2011 and further explored areas for potential action. While no formal recommendations were made, the workgroup engaged in useful dialogue that will assist policy development in the future.
New York is looking to the federal government to help fund the MIF since Medicaid is a direct beneficiary. Other Medicaid malpractice reforms, including efforts to lower costs for physicians, may also need federal participation in order to be effective.
|top of section| |table of contents|Redefining the State/Local Relationship in Medicaid
One of the most contentious issues in New York State Medicaid is the manner in which the program is financed and administered. New York, unlike almost any other state, finances a portion of Medicaid with county property tax revenue. In addition, New York relies heavily on local districts to manage the day-to-day tasks associated with administering this large and complex program.
Not surprisingly, local officials are very concerned about Medicaid costs and the overall impact the program has on county budgets. MRT created a special work group to grapple with this complex topic. This topic has been made even more complex by two recent developments which have made the status quo no longer an option. These developments include:
- A new state law requiring a five-year plan to implement the state assumption of Medicaid administration.
- Adoption of the Accountable Care Act at the federal level which creates the need for a new health insurance exchange which must first determine Medicaid eligibility.
Despite the complexity of these issues, the work group was able to reach consensus on important recommendations. The work group focused on the most immediate issue at hand which was the need for the state to implement a health insurance exchange by January 1, 2014. The recommendations provide the state with a path for how to successfully implement the health insurance exchange while at the same time centralizing the Medicaid eligibility determination process for most program participants. These recommendations were approved in the most recent state budget and the state is currently beginning its work on implementation.
On the ever challenging issue of financing the program the work group reached consensus on a recommendation that directs the state to develop and implement a multi-year plan for a more sustainable Medicaid financing system that phases out reliance on local taxes. This recommendation was hotly debated by the full MRT. MRT members expressed serious concerns that benefits and provider payments not be sacrificed to phase out the local contribution. The work group recommendation was then amended to address this concern. The most recent state budget made a major step toward addressing this concern by phasing out growth in the local share. This step will provide important relief for county budgets.
Finally, the group also provided a series of eligibility streamlining proposals which will make the Medicaid program more cost-effective and customer-friendly. These reforms will be implemented in lock-step with the rest of the recommendations regarding state take-over of Medicaid administration.
|top of section||top of section - Aim #3| |table of contents|
MEASURING SUCCESS
Comprehensive health care reform must be built on a comprehensive system of performance measurement. The task at hand is to quantify the triple-aim in order to benchmark current performance and set clear goals for the future.
New York has a large set of performance measures for Medicaid managed care, commercial managed care and Child Health Plus (CHPlus), which have been in place for over 15 years. The Quality Assurance Reporting Requirements (QARR) are a measurement set collected annually from managed care plans measuring performance in quality, access and utilization. Performance on these process and outcome measures has improved over time, and most measures exceed national benchmarks. Recently, measures of preventable hospitalizations have been added to the Medicaid measurement set. Unfortunately, for many high-volume, high-cost services including mental health, substance use and long term care, there are few metrics in place to measure quality of care.
In response to the new initiatives related to the Medicaid Redesign Team, New York is creating an even more comprehensive system of performance measurement that will apply not only to the Medicaid program or health plans, but will measure performance across the state´s entire health care system. Two sets of performance measures have been developed. The first set are the Medicaid core measures which will build off existing health care measures (HEDIS, CAHPS, provider level and more), fill in the gaps in measurement for long term care and behavioral health, and align efficiency measures like preventable hospitalizations across all payers. These efficiency measures are key indicators for success of many MRT initiatives including Health Homes, Patient Centered Medical Homes and care management for all. The second set are the population core measures which will align with New York´s public health goals, as well as monitor quality across all payers not just public programs. With these two measurement sets, New York will, for the first time, have a robust system of measurement that clearly captures the triple-aim.
The Medicaid core set of performance measurement is based on the triple aim and ten priority areas. The measures align with many of the current measurement activities including: 1) state-level QARR, 2) national-level HEDIS, and 3) federal-level measure sets, which include CHIPRA 2009 (section 1139A) initial core set of measures for children, the Affordable Care Act (section 2701) initial core set of health quality measures recommended for Medicaid-eligible adults, the American Recovery and Reinvestment Act of 2009 (ARRA) measures of meaningful use and CMS´ proposed health home measurement set. The Medicaid core set is meant to be a comprehensive set of measures for Medicaid that the state can use to track improvement over time. The Medicaid core set can be found in Figure 5.
For each performance measure within each priority area, benchmarks were developed for short-term (1-2 years), mid-term (3-4 years) and long term (year 2020) improvement. Benchmarks were developed with Medicaid managed care data, based on the opportunity for improvement. For example measures where current performance is in the 85-90 percent range, modest improvement is expected, while measures in the 50-60 percent range, a higher rate of improvement is anticipated.
In addition to the core set of measures for Medicaid, New York is tracking a core set of population measures across all payers. Medicaid is the largest purchaser of health care in New York State, and has responsibility to not only improve the care being delivered to Medicaid enrollees, but also improve the overall health care delivery system. The population core set of measures can be found in Figure 6.
New York´s goal is that these measures will drive both policymaking and the focus of health care improvements in the state for many years to come. Before these measures become final, input from outside experts and stakeholders will be gathered. The United Hospital Fund (UHF), which recently published a paper on measuring quality for complex populations, has offered to assist the state in finalizing its measurement sets. With assistance from the UHF, the state expects to finalize the set of measures and release a comprehensive performance dashboard soon. The dashboard will be updated periodically and will need to evolve, as measures change, and new priorities arise.
Finally, New York currently has a Pay for Performance program in Medicaid managed care. The core set of measures that are finally adopted will be the basis for any quality incentives going forward. New York is committed to using its purchasing power to drive improvement in its core measures.
Figure 5. Proposed Medicaid Quality Measures - Across the Triple Aims
| Number | Health Care Priority Area |
Quality Measure | Current Performance 2010 |
2013 | 2015 | 2020 |
|---|---|---|---|---|---|---|
| AIM 1 Improving Care | ||||||
| 1 | Preventive Care | Chlamydia screening (Ages 16-24) | 68 | 70 | 71 | 74 |
| 2 | Preventive Care | Childhood immunizations (Combination 3 - 4312314) | 73 | 74 | 76 | 78 |
| 3 | Preventive Care | Annual dental visit for children (Ages 2-21) | 53 | 55 | 58 | 62 |
| 4 | Women´s Health | Cervical Cancer Screening | 72 | 73 | 75 | 78 |
| 5 | Women´s Health | Frequency of Ongoing Prenatal Care - 81 to 100% of visits | 74 | 75 | 77 | 79 |
| 6 | Women´s Health | Low Birth weight Deliveries (*A low rate is desirable) | 7 | 6.8 | 6.6 | 6.3 |
| 7 | Chronic Care | Follow up care for children prescribed ADHD medication - Initiation | 58 | 60 | 62 | 66 |
| 8 | Chronic Care | Follow up care for children prescribed ADHD medication - Continuation | 64 | 66 | 68 | 71 |
| 9 | Chronic Care | Medication Management for People with Asthma | TBD | TBD | TBD | TBD |
| 10 | Chronic Care | Comprehensive diabetes care - HbA1c control (<8.0) | 55 | 57 | 60 | 64 |
| 11 | Chronic Care | Comprehensive diabetes care - LDL-c control (<100mg/dL) | 44 | 47 | 50 | 55 |
| 12 | Chronic Care | Controlling high blood pressure for persons with hypertension | 67 | 69 | 70 | 74 |
| 13 | Chronic Care | Engaged in Care for People Living with HIV/AIDS | 80 | 82 | 84 | 88 |
| 14 | Mental Health | F/U after Hospitalization for MH - within 7 days | 70 | 72 | 73 | 76 |
| 15 | Mental Health | F/U after Hospitalization for MH - within 30 days | 85 | 86 | 87 | 88 |
| 16 | Mental Health | Proportion of Schizophrenia Patients With Long-Term Utilization of Antipsychotic Medications | TBD | TBD | TBD | TBD |
| 17 | Substance Abuse | Initiation and Engagement of Alcohol and Other Drug Dependence | TBD | TBD | TBD | TBD |
| 18 | Substance Abuse | F/U after Hospitalization for Substance Abuse | TBD | TBD | TBD | TBD |
| 19 | Long Term Care | No Falls | 85 | 86 | 87 | 88 |
| 20 | Long Term Care | Flu Shot | 83 | 84 | 85 | 86 |
| 21 | Primary Care | Percent of enrollees in PCMH | TBD | TBD | TBD | TBD |
| 22 | Health Care Reform | Percent of High Cost/High Need Cases in Health Homes | TBD | TBD | TBD | TBD |
| AIM 2 Improving Health | ||||||
| 1 | Preventive Care | Weight Assessment and Counseling for Children and Adolescents - BMI Percentile | 65 | 67 | 69 | 72 |
| 2 | Preventive Care | Weight Assessment and Counseling for Children and Adolescents - Nutrition | 71 | 72 | 74 | 77 |
| 3 | Preventive Care | Weight Assessment and Counseling for Children and Adolescents - Physical Activity | 58 | 60 | 62 | 66 |
| 4 | Chronic Care | Use of tobacco cessation products | TBD | TBD | TBD | TBD |
| 5 | Long Term Care | Depression (*A low rate is desirable) | 25 | 24 | 23 | 20 |
| 6 | Long Term Care | Disruptive/Intense Daily Pain (*A low rate is desirable) | 11 | 10 | 9 | 7 |
| 7 | Long Term Care | Urinary Incontinence (*A low rate is desirable) | 73 | 70 | 67 | 61 |
| 8 | Patient Perspective | Getting care quickly | 77 | TBD | TBD | TBD |
| 9 | Patient Perspective | Getting needed care | 74 | TBD | TBD | TBD |
| 10 | Patient Perspective | Care coordination | 74 | TBD | TBD | TBD |
| AIM 3 Reducing Costs | ||||||
| 1 | Preventable Events | Preventable Hospital Admissions (PQIs) (*a low rate is desirable) | TBD | TBD | TBD | TBD |
| 2 | Preventable Events | Potentially Preventable Preventable Readmissions(*a low rate Events is desirable) | TBD | TBD | TBD | TBD |
| 3 | Preventable Events | Preventable ER Visits (*a low rate is desirable) | TBD | TBD | TBD | TBD |
| 4 | Health Care Reform | Percent of Enrollees needing Long Term Care Services in Nursing Homes (*a low rate is desirable) | TBD | TBD | TBD | TBD |
| 5 | Health Care Reform | Medicaid Spending within Global Cap | TBD | TBD | TBD | TBD |
| 6 | Health Care Reform | Rate of Growth of Medical Malpractice Premiums | TBD | TBD | TBD | TBD |
| 7 | Health Care Reform | Percent Eligibility Determination done at State Level | TBD | TBD | TBD | TBD |
Figure 6. Population Quality Measures
| Number | Quality Measure | Current Performance 2010 |
2013 | 2015 | 2020 |
|---|---|---|---|---|---|
| Diabetes | |||||
| 1 | New cases diagnosed with diabetes (per 1,000) | 6.00 | 5.80 | 5.70 | 5.40 |
| 2 | Preventable Hospitalizations (PQIs) for short term complications of diabetes, age 6-17 (per 100,00) | 3.40 | 3.22 | 3.15 | 3.00 |
| 3 | Preventable Hospitalizations (PQIs) for short term complications of diabetes, age 18+ (per 100,000) | 5.60 | 5.46 | 5.32 | 5.04 |
| Obesity | |||||
| 1 | Percent of WIC children (ages 2-4) who are obese | 14.40 | 11.60 | 10.60 | 9.60 |
| 2 | Percent of WIC children (ages 6-11) who are obese | 17.00 | 16.67 | 16.35 | 15.70 |
| 3 | Percent of WIC children (ages 12-17) who are obese | 18.00 | 17.50 | 17.00 | 16.10 |
| 4 | Percent of WIC children (ages 2-4) who are obese | 24.50 | 23.89 | 23.28 | 22.05 |
| Asthma | |||||
| 1 | Preventable Hospitalizations (PQIs) Asthma - all ages (per 10,000) | 21.50 | 21.00 | 20.40 | 19.40 |
| 2 | Preventable Hospitalizations (PQIs) Asthma - ages 0-17 (per 10,000) | 31.30 | 30.40 | 29.56 | 28.27 |
| 3 | Preventable Emergency Department Visit - all ages (per 10,000) | 85.70 | 83.60 | 81.40 | 77.10 |
| 4 | Preventable Emergency Department Visit - ages 0-17 (per 10,000) | 147.00 | 143.30 | 139.70 | 132.30 |
| Lead | |||||
| 1 | Incidence of children <72 months old with confirmed blood levels >= 10ug/dl (per 1,000) | 11.10 | 10.80 | 10.50 | 9.90 |
| Tobacco | |||||
| 1 | Percent cigarette smoking in adolescents in past month | 12.60 | 10.00 | 9.00 | 6.00 |
| 2 | Percent cigarette smoking in adults | 15.50 | 12.00 | 12.00 | 10.00 |
| 3 | Percent of Medicaid using smoking cessation products | 13.00 | 25.00 | 40.00 | 50.00 |
| Birth Outcomes | |||||
| 1 | Percent early prenatal care (First Trimester) | 73.30 | 74.40 | 75.50 | 77.90 |
| 2 | Percent Low Birth weight Deliveries | 8.20 | 8.20 | 7.90 | 7.80 |
| 3 | Percent preterm births | 12.30 | 11.90 | 11.50 | 11.10 |
| 4 | Percent Unintended Pregnancy | 29.60 | 28.60 | 27.60 | 26.60 |
| Immunization | |||||
| 1 | Adult Flu Shot | 68.30 | 69.90 | 71.60 | 75.00 |
| 2 | Adults >= 65 Pneumococcal vaccine | 66.10 | 67.80 | 69.50 | 73.00 |
| HIV Prevention | |||||
| 1 | New Diagnosis of HIV (per 100,000) | 21.30 | 20.75 | 20.20 | 19.17 |
CONCLUSION
New York is well positioned to lead the nation in Medicaid reform. Governor Cuomo´s Medicaid Redesign Team helped develop a multi-year action plan that if fully implemented will not only bend the state´s Medicaid cost curve but also improve health outcomes for more than 5 million New Yorkers.
Medicaid reform also has the potential to mean broader health system reform in New York. The reforms identified in the action plan will lead to broad changes in health care delivery that will benefit the state´s 19 million residents. New York is willing to use all the tools at its disposal to drive innovation across the health care system, including aligning payment strategies with commercial insurers through the state´s health insurance exchange.
New York is also committed to establishing a new relationship with the state´s second largest payer, Medicare. A new state-federal compact is needed that will allow for true cooperation and alignment. This cooperation is especially important for the 700,000 New Yorkers who are enrolled in both programs. Billions of dollars in savings is possible as well as improved patient outcomes if the full action plan recommendations are implemented as they relate to dually-eligible members.
Finally, to fully implement the MRT action plan a ground-breaking new Medicaid 1115 waiver will be necessary. The waiver will both allow the state to reinvest in its health care infrastructure as well as give the state the freedom to innovate. The new waiver will allow the state to prepare for implementation of the national health care reform as well as effectively bend the cost curve for the state´s overall health care system.
New York is ready to lead. New York is prepared to work very hard to fundamentally re-shape how health care is delivered so as to improve patient outcomes and lower costs. New York is also united in its support for reform. Governor Cuomo´s innovative Medicaid Redesign Team ensured that the action plan outlined in this report has broad support among the health care stakeholder community. Now all is left is to implement. New York will work with the federal government as well as the state´s health care stakeholders to successfully implement this important action plan.
|top of section| |table of contents|Appendix A
New York State Medicaid - High Cost Populations vs. Total (CY2009) Includes duals and non-duals
| Developmental Disabilities |
Long Term Care | Behavioral Health | Other | Total | |
|---|---|---|---|---|---|
| High Cost Population | |||||
| Members Served | 52,118 | 209,622 | 408,529 | 306,087 | 976,356 |
| Expenditures | 6,467,486,840 | 10,688,288,537 | 6,328,160,789 | 2,418,882,194 | 25,902,818,360 |
| Total Population | |||||
| Members Served | 101,635 | 368,762 | 704,019 | 4,149,822 | 5,324,238 |
| Expenditures | 9,989,010,415 | 16,147,709,332 | 8,059,791,122 | 12,160,808,767 | 46,357,319,636 |
| High Cost Percent of Total | |||||
| Members Served | 51.3% | 56.8% | 58.0% | 7.4% | 18.3% |
| Expenditures | 64.7% | 66.2% | 78.5% | 19.9% | 55.9% |
Developmental Disabilities Population includes Inpatient, Waivers, ICF-DD, Managed Care and Other. Long Term Care includes persons with more than 120 days of LTC needs and includes persons enrolled in Managed Long Term Care (PACE, Partial and MAP). Behavioral Health and/or Substance Abuse classification is at any time during CY2009. The Other category includes all other Medicaid recipients. Managed care enrollees are included in all four groups. Recipient counts are unique, as classifications are mutually exclusive.
|top of section| |table of contents|Appendix B
Principles for Behavioral Health Services in a Managed Care Environment
As charged by the MRT, the Work Group identified a number of key elements of design and practice needed for a managed and coordinated behavioral health care system in New York State relevant across the age span. Beginning with the first meeting, the Work Group engaged in a goal-setting and prioritization process to reach group consensus on these key principles. The Work Group also identified critical types of metrics and indicators that should be measured to determine the extent to which these principles are met. The following are the principles established by the Work Group:
- There should be mechanisms at multiple levels for connecting and coordinating all of the different participants, including healthcare providers, payers, and care managers. The delivery of clinical care should be coordinated and efficient.
- Mental health, physical health, and substance use disorders should be addressed in an integrated manner.
- APG caps on physical health services provided in behavioral health settings and behavioral health services in physical health settings must be revisited.
- Patient/Consumer screening for mental illness and substance use disorders should be done across specialty and primary care settings and should use state-of-the-art techniques and technology.
- Providers should use electronic medical records and available mechanisms for health information exchange. They should have access to, and use, their patient/consumers´ Medicaid data.
- There should be a "no wrong door" approach so that no matter where patients/consumers enter the system, they are guided to the right provider. Standardized screening tools should be used.
- A system of empowered care coordination should be established, and be stratified by risk/need of patient/consumer. Payment models should incentivize coordination among physical and behavioral health providers.
- Duplication of services should be avoided.
- Co-location of services should be one available model to promote integrated care.
- There should be clarity around roles and accountability across service providers.
- Linkages to other systems, such as the criminal justice, juvenile justice, homeless, and child welfare systems, also should be developed.
- Payment for services should be tied to patient/consumer outcomes.
- Incentives should guide providers to the appropriate type and amount of care.
- The reimbursement rate structure should recognize the varying levels and capabilities of providers.
- There should be flexibility to finance wrap-around services.
- The fee-for-service "mentality" should be eliminated, although that does not preclude using fee-for-service payment mechanisms within a managed care arrangement.
- Patient/Consumer input and choice is critical.
- Whenever possible, consumer choice should be preserved.
- There should be in-person care coordination activities for high-need users.
- Peer programs should be used to help engage patient/consumers.
- Families should be integrated into care whenever possible.
- Treatment should be based on condition, and not on insurance status.
- There should be a person-directed focus on wellness and recovery.
- Consumer access should be considered as part of any data-sharing initiative.
- Attention should be paid to social factors that influence individual behavior and outcomes, such as employment and financial status.
- Available social services outside of health care should be utilized maximally.
- Housing resources need to be available directly for timely use to avoid lengthy or repeat admissions, and to provide stability for patient/consumers in the community.
- Money saved should be reinvested smartly to improve services for behavioral health populations.
- Savings from better managed behavioral and physical health care should be reinvested to the extent possible for improved outcomes and reduced health costs.
- Reinvestment should prioritize non-clinical support services, such as housing, peer, employment, and family services.
- Investment in preventive services that avoid the need for tertiary care should be incentivized.
- Savings might be shared with consumers to incentivize engagement.
- Distinction in design and operation must be made to address the unique needs of children and their families.
- The needs of older adults are unique and require special attention.
- For older adults, care coordination will require interface with home health services, adult day care, and a heightened sensitivity to physical health needs.
- Regulatory burden should be minimized.
- Unfunded mandates should be avoided.
- The paperwork required of providers by government and managed care organizations should be reduced, or, at the very least, not increased.
- The diversity of New York State´s communities should be taken into account.
- Varying levels of patient/consumer needs and provider capacities may dictate different approaches in different parts of the State, especially those which are predominately rural or urban.
- Key outcomes at the individual, provider, and system levels include:
- Sustainable medical-loss ratios and reasonable levels of reinvestment.
- Elimination of inappropriate financial barriers to care.
- Adequate and promptly paid reimbursement rates to ensure appropriate capacity.
- Appropriate risk-adjustment to incentivize treatment of the harder to serve.
- Payments that promote the delivery and use of the appropriate level of care.
- Good clinical outcomes for key chronic medical conditions.
- Cultural and linguistic competency and use of peer services.
- Reduced hospital admissions inpatient detoxification and SUD inpatient rehabilitation services.
- Reduced mortality and health disparities associated with mental illness and substance use.
- Reduced gap between prevalence of service engagement and prevalence of conditions in the population.
- Reduced criminal and juvenile justice involvement.
- Reduction in use of court-ordered outpatient treatment for mental health (excluding mental health courts).
- Improved care transitions (e.g., appointments after hospitalizations).
- Meaningful and useful communication across providers.
Appendix C
Medicaid Redesign Basic Benefit Review Work Group Guiding Principles
The guiding principles recommended by the Work Group are as follows:
- All Medicaid members will be treated equitably without discrimination so that they may attain the highest level of health.
- If Medicaid budgets are insufficient to support all potential services, then priorities must be set by the program among services to be provided based on evidence and effectiveness.
- Priorities in benefit design must maximize the health of the population served by the program and be based on an assessment of benefits, harms, and costs.
- When assessing benefits, harms and costs, empirical evidence (when available and of high quality) will be critically appraised to determine its appropriateness for policy application and will be given more weight than subjective or expert opinion. The hierarchy of evidence used for coverage decisions includes:
- Type I (highest): meta-analysis or systematic review of multiple well designed randomized controlled trials.
- Type II: one or more well designed randomized controlled trials.
- Type III: well designed studies which could include nonrandomized controlled, pre-post, cohort, case-control, cross-sectional, observational studies.
- Type IV: expert panel opinion/ high quality professional guidelines.
- Type V (lowest): single expert, case report.
- Criteria to be considered for evaluation of specific services and benefits follow those of evidence-based health care, and include:
- Evidence that it is better than receiving no service for the specific clinical condition(s) or populations.
- The added benefit per added cost compares favorably to other treatments for the same condition.
- Evidence that access to less expensive interventions does not create undue burden for individuals.
- Evidence that benefits outweigh harms in improving health.
- The burden of presenting evidence for the above criteria lies with those advocating the use of the service.
- Level of evidence will be specified in accord with typology described above and reassessed when sufficient new evidence would suggest a possible change in benefit coverage.
- Considering cost and value as well as cost control through benefit design are legitimate as they support the ability of the state to provide the maximum number of services that are effective in improving the health of the population. This approach will make the most efficient use possible of available resources and maximize the public good. Criteria for excluding or limiting benefits should focus on those services in which:
- Costs are high and evidence for clinical effectiveness is highly variable or low, or (the clinical intervention (product or service) is overused compared to evidence-based appropriateness criteria.
- Evidence of additional value (benefits to cost) compared to other treatments for the same condition is low.
- A highly limited number of benefit decisions may require an individualized approach including those pertaining to rare or emerging clinical conditions for which a high level of evidence is not realistic, certain experimental treatments where no ´standard of care´ exists, and/or complex emergency circumstances.
- In the evaluation of services and benefit design the outcomes of interest should include the preferences of patients, individual autonomy, and those outcomes generally of high value to patients such as survival, function, symptoms and quality of life.
- Evaluation of benefit decisions on utilization, costs, and health outcomes (where feasible) should follow any ´major´ benefit decisions in order to assess impact post- coverage decisions.
- Every attempt should be made to eliminate any conflict of interest in the use of clinical experts.
Appendix D
Medicaid Redesign Brooklyn Work Group Brooklyn Hospitals: Specific Recommendations
The Work Group focused its attention on the three most troubled hospitals in Brooklyn that require immediate intervention to avert financial collapse: Brookdale Hospital Medical Center, Interfaith Medical Center, and Wyckoff Heights Medical Center. The Work Group notes that Long Island College Hospital (LICH) also would also fall into this category, but for its recent affiliation with SUNY Downstate Medical Center which has created the potential for a turnaround. In addition, the Work Group considered the position of two other key hospitals, Brooklyn Hospital Center and Kingsbrook Jewish Medical Center, that do not exhibit the same level of financial distress as the others. However, they need to put in place plans for long-term sustainability and can play a leadership role in creating integrated systems to strengthen healthcare delivery in the communities served by all six hospitals. Specific recommendations are made for these six hospitals:
Brookdale Hospital Medical Center and Kingsbrook Jewish Medical Center: The Work Group recommends that Kingsbrook Jewish take the lead in establishing an integrated system with Brookdale, either under a common active parent or other accountable governance structure. The Work Group recommends new executive leadership at Brookdale and a separation from MediSys. A viable plan would require the creation of a new governance structure and a new board of directors for the integrated system.
The restructuring of Brookdale´s debt and other obligations is essential to the success of this proposal. Any reconfiguration would also require the implementation of a plan to strengthen primary care in the communities served by the two institutions and clinical integration among participating providers. The Kingsbrook/Brookdale system should also consider reducing its bed complement and investing in additional ambulatory care services. Development and implementation of this plan recommendation should take place under the guidance of the Brooklyn Healthcare Improvement Board, with input from the communities served.
Brooklyn Hospital Center, Interfaith Medical Center, and Wyckoff Heights Hospital: The Work Group recommends the integration of these three institutions into a single system under an active parent, or other accountable governance structure, led by Brooklyn Hospital Center. In light of the precarious financial positions of Interfaith and Wyckoff, the Work Group would like to ensure that Brooklyn Hospital, which has recently emerged from bankruptcy and is demonstrating sound financial practices, is not brought down by this plan. Indeed, we recommend that Brooklyn Hospital be given the support to lead the transformation and restructure the operations at Interfaith and Wyckoff.
This system should streamline inpatient and tertiary care in a manner that is sustainable and aligned with community needs. A critical element of the restructuring plan must be enhanced access to high quality primary care and outpatient services. Development and implementation of the plan should proceed under the guidance of the Brooklyn Healthcare Improvement Board, with input from the communities served.
SUNY Downstate Medical Center and Long Island College Hospital (LICH): In light of the recent acquisition of LICH, SUNY Downstate should consider consolidating inpatient services at the LICH campus, thereby eliminating excess capacity and permitting the medical center to focus its inpatient resources and expertise on one location. With the new campus and the expansion of services at the neighboring Kings County Hospital, SUNY Downstate should reconsider any planned expansion of beds at the former Victory Hospital site and any development of an ambulatory facility in the vicinity of University Hospital or at the former Victory Hospital site.
Any request by SUNY Downstate to open additional inpatient beds at the Victory Hospital site should be denied.
Kingsboro Psychiatric Center: The Office of Mental Health (OMH) should close the inpatient service of Kingsboro Psychiatric Center (KPC) and, working with the Department of Health, redirect resources to community-based behavioral health services that would function in collaboration with Brooklyn hospitals. Intermediate psychiatric hospital care for Brooklyn residents and court referrals should be provided primarily by South Beach Psychiatric Center, which currently serves a large section of Brooklyn. KPC´s existing array of community-based services should remain within the community.
Conversion of a majority of the high cost KPC inpatient beds into intensive community treatment and support services would be well-timed with the implementation of the Medicaid Health Home initiative in the borough. Improved coordination, coupled with expanded service availability, will significantly reduce the burden on Brooklyn´s emergency rooms and inpatient services.
Woodhull Hospital, Kings County Hospital and Coney Island Hospital: These hospitals are operated by the New York City Health and Hospitals Corporation (HHC). Although they have been linked principally with the other institutions in the HHC system, rather than with local facilities, it is now essential that they become more active partners in the Brooklyn delivery system.
|top of section| |table of contents|
Follow Us