December 2010 Volume 26, Number 14
New York State Medicaid Update
The official newsletter of the New York Medicaid Program
David A. Paterson, Governor
State of New York
Richard F. Daines, M.D. Commissioner
New York State DOH
Donna J. Frescatore, Medicaid Director & Deputy Commissioner
Office of Health Insurance Programs

In this issue....
POLICY AND BILLING GUIDANCE
Important Information about the IRS 1099 Form
Medicaid Expands Coverage for Diabetes Self-Management Training (DSMT)
Medicaid Coverage of Genetic Counseling
2011 Healthcare Common Procedure Coding System Update
Hospice Care for Children in Medicaid, Family Health Plus and Child Health Plus
Mandatory Certifications
Mandatory Compliance Program Certification of Effectiveness
Changes to Ambulette, Taxi and Livery Transportation Procedure Codes
Managed Care Covered Services
PHARMACY UDATES
Medicaid Coverage/Billing Requirements for Risperdal Consta, Invega Sustenna & Zyprexa Relprevv
Treatment for Recurrent Diaper Rash
New York Medicaid Provides In-Service Education
ALL PROVIDERS
X12 Version 5010 Mediciad Update Special Edition Soon Available
Smoking Cessation Advertisement
Provider Directory
Important Information about the IRS 1099 Form
Return to Table of Contents
Computer Sciences Corporation (CSC), the eMedNY contractor for the NYS Department of Health (NYSDOH), annually issues the Internal Revenue Service (IRS) Form 1099 to providers for the previous year's Medicaid payments. 1099 forms are issued with the individual provider's Social Security Number, or if a business, with the Federal Employer Identification Number (FEIN) registered with New York Medicaid. As with previous years, the IRS 1099 amount is not based on the date of the checks/EFTs; rather, it is based on the date the checks/EFTs were released to providers.
Since there is a two-week payment lag between the date of the checks/EFTs and the date the check/EFT is issued, the IRS 1099 amount will not correspond to the sum of all checks/EFTs issued for your provider identification number during the calendar year.
The IRS 1099 issued for 2010 will include the following:
- Check/EFT dated 12/21/09 (Cycle 1687) released on 01/06/2010 through,
- Check/EFT dated 12/13/10 (Cycle 1738) released 12/29/10.
Each year, CSC receives calls from individual providers who are issued 1099s for funds the practitioner is unaware of. This generally occurs because in order for group practice providers to direct Medicaid payments to a group NPI and corresponding IRS 1099 for the group, group practices must submit the group NPI in the appropriate field on the claim (paper or electronic). When claims are submitted without the group NPI listed it causes payment to go to the individual provider and his/her IRS 1099. Regardless of who deposits the funds, the 1099 will be issued to the individual provider when the funds had been paid to the individual provider's NPI.
NOTE: 1099s are not issued to providers whose yearly payments are less than $600.00. IRS 1099s for the year 2010 will be mailed no later than January 31, 2011.M
Questions? Please contact the eMedNY Call Center at (800) 343-9000.
Medicaid Expands Coverage for Diabetes Self-Management Training (DSMT)
Return to Table of Contents
Billing and claims submission:
eMedNY Call Center at (800)343-9000.
DSMT enrollment forms:
Division of Provider Relations and Utilization Management at (518) 474-8161.
DSMT coverage:
Division of Financial Planning and Policy at (518) 473-2160.
Effective January 1, 2011, Medicaid will reimburse for Diabetes Self-Management Training (DSMT) when provided by an Article 28 clinic (hospital outpatient department or free-standing diagnostic and treatment center) that is accredited by a CMS approved national accreditation organization (NAO). Currently, CMS recognizes the American Diabetes Association (ADA), American Association of Diabetes Educators (AADE) and Indian Health Services (IHS) as approved NAOs. Under this accreditation, DSMT can be performed by a New York State licensed, registered, or certified professional in one of the following professional disciplines:
- Registered Nurse
- Registered Nurse Practitioner
- Registered Dietician
- Physician (MD, DO)
- Pharmacist
- Physician Assistant
- Physical Therapist
DSMT services can be provided to beneficiaries who are newly diagnosed with diabetes, to beneficiaries with diabetes who are stable, or to beneficiaries with diabetes who have a medically complex condition such as poor control of diabetes or other complicating factor.
DSMT services can be provided in individual sessions, or in group sessions of no more than eight patients. Claims must include the appropriate ICD-9 code for diabetes mellitus: 250.XX, 648.0x, 648.8x, 775.0, or 775.1. DSMT services are billed in unit increments with one unit equaling 30 minutes of service using the following HCPCS codes:
- G0108 - Diabetes outpatient self-management training services, individual, per 30 minutes.
- G0109 - Diabetes outpatient self-management training services, group (2-8 patients), per 30 minutes.
No more than 10 hours or 20 units, of diabetes self-management training for a newly diagnosed beneficiary or beneficiary with a medically complex condition can be billed during a continuous six-month period. Beneficiaries who are medically stable can receive up to 1 hour, or 2 units, of diabetes self-management training in a continuous six-month period.
In order to bill for DSMT services, Article 28 clinics will need to request an enrollment form by contacting Medicaid's Rate Based Provider Enrollment Office at (518) 474-8161. To avoid reimbursement interruption providers are advised to notify Rate Based Provider Enrollment upon re-certification from the NAO.
The Medicaid program plans to expand provision of DSMT services to eligible physician office-based practices and pharmacies in the near future. Providers will be notified of this expansion in a future Medicaid Update. Medicaid will also continue to reimburse for DSMT services provided by Certified Diabetes Educators (CDEs) as previously described in the October 2008 Medicaid Update.
Medicaid Coverage of Genetic Counseling
Return to Table of Contents
Effective January 1, 2011, Medicaid will cover genetic counseling when provided by a certified or credentialed genetic counselor. Genetic counseling services may be provided in a practitioner's office or in an Article 28 hospital outpatient department (OPD) or free-standing diagnostic and treatment center (D&TC). Reimbursement will be made to physicians, nurse practitioners, licensed midwives and Article 28 clinics who employ or contract with the genetic counselors. Genetic counselors must be certified by the American Board of Genetic Counseling (ABGC), the American Board of Medical Genetics (ABMG) or be an advanced practice nurse in genetics (APNG), who is credentialed by the Genetic Nursing Credentialing Commission (GNCC). A written order is required.
New York Medicaid also covers genetic counseling services provided by physicians.
Genetic testing for inherited genetic variants is generally performed for one of several purposes:
- predictive testing of asymptomatic individuals to identify future disease risks, given increased risk as determined by an assessment of family history and risk factor profiles;
- diagnostic testing of individuals with symptoms to confirm a specific diagnosis or rule-out a suspected diagnosis;
- determination of genetic risks for offspring (prenatal diagnosis), family planning, and carrier testing;
- guidance of medical treatment (for example, pharmacogenetic testing);
- newborn screening follow-up and confirmatory testing as a result of a positive newborn screening test.
Except for routine newborn screening conducted by public health agencies, genetic counseling is appropriate prior to considering a genetic test, and after completion of the test. However, please note that a preimplantation genetic diagnosis associated with in vitro fertilization services is not covered by New York Medicaid.
Genetic counseling provided by a genetic counselor is billed under CPT code 96040 (Genetic Counseling). When genetic counseling is provided by a physician, the appropriate Evaluation and Management code should be used instead of CPT code 96040. Claims should include the diagnosis code that most closely describes the reason for the counseling.
Medicaid will pay for up to 2 hours of pre-genetic test counseling, and up to 2 hours of post-genetic test counseling per diagnosis based on "units of service" with one unit equaling 30-minutes of counseling. The maximum allowable session length is two hours (4 units).
Reimbursement to office-based practitioners is $32/unit. Clinic payment will be approximately $32/unit on a statewide average basis, but may vary somewhat by region and clinic type (i.e., freestanding or hospital).
To increase patient access to genetic counseling services in areas of the State without qualified genetic counselors, Article 28 OPDs may utilize telemedicine consultations with Article 28 OPDs that either employ or contract with credentialed or certified genetic counselors. To conduct a telemedicine consultation, the Article 28 OPD must have an interactive audio and video telecommunications system that permits a "real time" interactive consultation between a genetic counselor and patient. The Article 28 OPD that provides the genetic counseling (the hub) must include the modifier "GT" on the claim. The Article 28 OPD where the patient and their physician are located (the spoke) will bill a regular OPD visit. Both Article 28 OPD claims must include CPT code 96040.
For details on providing telemedicine consultations please see the September 2006 and the July 2010 issues of the Medicaid Update. These publications can be accessed respectively at:
- http://health.ny.gov/health_care/medicaid/program/update/2010/2010-07.htm#exp
- http://health.ny.gov/health_care/medicaid/program/update/2006/sep2006.htm
Questions? Please contact the following:
Billing and claims submission, eMedNY Call Center at (800) 343-9000.
Medicaid genetic counseling and telemedicine policy, Division of Financial Planning and Policy at (518)473-2160.
Funding for rural hospitals for purchasing of telemedicine equipment, Office of Rural Health at (518)402-0102.
Credentialing and privileging requirements, Office of Health Systems Management at (518) 402-1003.
2011 Healthcare Common Procedure Coding System Update
Return to Table of Contents
For billing dates of service on and after January 1, 2011, all health care providers and plans must utilize the 2011 Healthcare Common Procedure Coding System (HCPCS) as released by the federal Centers for Medicare and Medicaid Services (CMS).
Notification of coding changes (replacement codes) relating to Medicaid covered services will be available on each affected provider manual homepage, provider communication link.
For additional information, please visit: http://www.emedny.org/providermanuals/index.html
Other available coding resources include:
- HCPCS Level I (CPT-4) procedure codes for practitioners and laboratories can be purchased in hard copy or electronic format through many publishing houses.
- HCPCS Level II (Alpha-Numeric) codes for other medical services are available electronically at: http://www.cms.hhs.gov/HCPCSReleaseCodeSets/
- ICD-9 Diagnosis and Procedure codes (effective 10/1/2010) are available electronically at: www.cms.hhs.gov/icd9providerdiagnosticcodes. The codes are also available through publishing houses.
HCPCS and ICD-9 codes are not Medicaid specific. Providers must use the current code set when billing any health care payer. New codes will be identified in the 2011 Fee Schedules and Procedure Codes Sections in early 2011.
Questions? Contact Provider Relations and Utilization Management at (800) 342-3005, Option 8.
Hospice Care for Children in Medicaid, Family Health Plus and Child Health Plus
Return to Table of Contents
Effective March 23, 2011, New York Medicaid including Medicaid managed care, Family Health Plus (FHPlus), and Child Health Plus (CHPlus) will cover all medically necessary curative services, in addition to palliative care, for children under age 21 who receive hospice care. This change in coverage policy complies with recent changes to Section 2302 of the federal Affordable Care Act, entitled "Concurrent Care for Children."
This new provision applies ONLY to Medicaid, Medicaid managed care, FHPlus and CHPlus recipients under age 21 and allows hospice care to be available without forgoing any other medically necessary curative services to which the child is entitled under Medicaid, or under the enrollee's FHPlus or CHPlus benefit package, for treatment of the terminal illness.
There is no change in the eligibility criteria for electing hospice care. The child must be certified by a physician as terminally ill, defined as a medical prognosis for a life expectancy of 6 months or less if the illness runs its normal course. Hospice provides palliative and supportive care that focuses on pain and symptom management related to the terminal illness and related conditions.
Prior to enactment of the new law, curative treatment of the terminal illness ceased upon election of the hospice benefit. Curative care refers to treatment with intent to cure the child's terminal illness. Palliative care does not aim to cure but rather is focused on relieving pain and symptoms related to the terminal illness with the goal of improving quality of life. The goal of this change in coverage is to provide a blended package of curative, palliative and support services for children, as needed.
FHPlus and CHPlus enrollees receive both hospice and covered curative services through their managed care plan. Hospice services are carved-out of the Medicaid managed care benefit package and billed directly to eMedNY, while covered curative services are billed to the health plan. Individuals receiving hospice services may not be newly enrolled in Medicaid managed care, but individuals already enrolled in Medicaid managed care may remain enrolled after they begin receiving hospice services.
General questions? Please call the Office of Long Term Care, Division of Home and Community Based Services at (518) 408-1638 or e-mail: homecare@health.state.ny.us.
Medicaid program questions? Please call the Office of Health Insurance Programs, Division of Financial Planning and Policy at (518) 473-2160.
Medicaid Managed Care and FHPlus questions? Please call the Office of Health Insurance Programs, Division of Managed Care at (518) 473-0122.
Child Health Plus (CHPlus) questions? Please call the Bureau of Child Health Plus Enrollment at (518) 473-0566.
Medicaid billing questions? Please call the eMedNY Call Center at (800) 343-9000.
Mandatory Certifications
Return to Table of Contents
Reminder: Effectiveness of Compliance Programs - Required During December 2010
Reminder: Compliance with the Requirements of Deficit Reduction Act (DRA) - Required on or before January 1, 2011
New York State Social Services Law (SSL) § 363-d and 18 NYCRR Part 521 (Part 521), require Medicaid providers to certify annually each December that they have an effective compliance program in place. (See October 2010 Medicaid Update). This is an annual requirement.
The federal Deficit Reduction Act of 2005 (DRA) instituted a requirement for health care entities receiving or making $5 million or more in Medicaid payments during a federal fiscal year to establish written policies and procedures informing their employees, contractors and agents regarding federal and state false claim acts and whistleblower protections. Providers meeting the DRA's $5 million requirement must certify by January 1 of each year that they have met the DRA's requirements for the federal fiscal year that ended the prior September 30th. This is an annual requirement.
Medicaid providers are reminded that they have an obligation to determine if they must certify to one, or both, of the following:
- 1. That they have an effective compliance program as required by SSL § 363-d and Part 521.
- 2. That DRA applies to them and that they have met the DRA's requirements.
These two certification requirements are separate from each other and require a review of different statutory and regulatory requirements.
If you are required to certify under both programs, two separate certifications are required.
The certification forms, FAQs and statutory and regulatory references are available on the OMIG Web site at: http://www.omig.ny.gov. Look for the "Compliance" tab on OMIG's home page and then click "Provider Compliance."
The resources for the effective compliance program certification are found under the heading: "Mandatory Provider Compliance Programs."
The resources for the DRA certification are found under the heading: "Deficit Reduction Act." If you have any questions, please contact the OMIG's Bureau of Compliance at: compliance@omig.ny.gov.
Reminder: Required by December 31, 2010
Mandatory Compliance Program Certification of Effectiveness
Return to Table of Contents
Social Services Law (SSL) §363-d and 18 NYCRR Part 521 (Part 521), requires that certain providers adopt and implement an effective compliance program. If you are a Medicaid provider that is required to certify that you have an effective compliance program in place, please remember that the certification must occur during December 2010. This is an annual requirement.
The OMIG has revised the form that will be used for 2010. It is currently available for download at www.omig.ny.gov.
If you determine that your compliance program is not effective, you should not certify, but you are required to notify the OMIG with the following:
1. Identify the provider:
- a. the name of the provider;
- b. the provider's Federal Identification Number ("FEIN") that is used to bill Medicaid;
- c. all Provider Numbers that provide services to Medicaid beneficiaries under the FEIN; and
- d. the name, telephone number and e-mail address of the person providing the communication to OMIG.
2. The subject line on your e-mail should indicate your name and "Unable to Certify;"
3. The body of your e-mail should indicate:
- a. the reasons why your compliance program is not effective;
- b. the steps you are taking to make your compliance program effective; and
- c. when you expect that you will be able to certify that your compliance program is effective.
If providers are unable to certify that their compliance program is not effective please e-mail: compliance@omig.ny.gov.
Failure to have an effective compliance program, and/or failure to certify that you have an effective compliance program, is a violation of SSL § 363-d and Part 521.
The regulation, certification form, and FAQ's are available on the OMIG Website at: http://www.omig.ny.gov.
Questions? Please e-mail the OMIG's Bureau of Compliance at: compliance@omig.ny.gov.
Attention: Transportation Providers - Effective 2011
Changes to Ambulette, Taxi and Livery Transportation Procedure Codes
Return to Table of Contents
New York Medicaid will implement new transportation procedure codes contained in the federal Healthcare Common Procedure Code System (HCPCS). Effective for dates of service on or after April 27, 2011, transportation claims will require new procedure codes and modifiers in order to be processed. Claims with dates of service on or after April 27, 2011, that list the current transportation procedure codes that begin with the prefix "NY" will be denied. Instead, the new procedure codes and modifiers, as described on the following page, must be submitted. (Claims submitted on or after April 27, 2011, for dates of service up to and including April 26, 2011, should continue to use the prior authorized "NY" codes.)
Transportation providers should consider making any changes necessary to billing systems now, in order to submit claims correctly for dates of service on or after April 27. (If you use ePACES for claims submission, you do not need to make any changes.)
The newly authorized transports may use only a solitary HCPCS code, while other transportation services will have a two letter modifier attached to the same or another HCPCS code. While a solitary HCPCS code will reimburse one amount, the same HCPCS code authorized with a modifier will reimburse a different amount.
Department staff, in collaboration with staff of the department of social services in each county, have reassigned the current procedure codes with the new HCPCS/modifier structure. The new codes/modifiers will be issued through your current prior authorization processes beginning March 27, 2011, for dates of service on or after April 27, 2011. For dates of service between March 27 and April 27, 2011, the "NY" codes will continue to be issued. Ensuing transportation and ordering provider prior authorization rosters will reflect either the new codes/modifiers, or the "NY" codes, depending on the date of service.
Orderers of New York City transportation services will be given specific ordering guidelines using these HCPCS codes and modifiers in the January 2011 Medicaid Update.
Please see following page for a listing of available national codes and modifiers, as well as the definition of each, which will be available in each county. Please note that each county may be assigned different codes based upon the county's individual transportation needs; not every HCPCS code or modifier will be used in every county. For an upstate county's specific fee schedule using the new HCPCS/modifier structure, or for questions regarding this article, please contact the Medicaid Transportation Policy Unit at (518) 473-2160 or via e-mail to MedTrans@health.state.ny.us.
| HCPCS Code | Definition |
|---|---|
| A0100 | Taxi: Local trip or trip within the common medical marketing area |
| S0215 | Taxi/Livery/Van Mileage |
| A0110 | Van transportation by county-based provider (e.g., public transit) |
| A0120 | Van transportation by private vendor |
| A0130 | Ambulette: Local trip or trip within the common medical marketing area |
| T2004 | Ambulette: One Way Trip |
| S0209 | Ambulette Mileage |
| T2005 | Ambulette Stretcher transportation |
| T2049 | Ambulette Stretcher mileage |
| A0170 | Parking Fees & Thruway/Tunnel/Bridge Tolls |
| Modifier | Definition |
|---|---|
| AX | Dialysis transportation |
| CG | Unassigned: Available for extraordinary transports |
| HA | Transport to a child/adolescent program |
| HB | Transport to a non-geriatric adult program |
| HC | Transport to adult day health care |
| HE | Transport to a mental health program |
| HF | Transport to a substance abuse program |
| HG | Transport to addiction program |
| HH | Transport to integrated mental health/substance abuse program |
| HI | Transport to integrated mental health/developmental disabilities program |
| HK | Transport to specialized mental health programs for high-risk populations |
| SC | Transportation service not otherwise defined |
| TF | Intermediate Level of Care |
| TG | Complex/High Level of Care |
| TJ | Group ride of children/adolescents |
| TK | Extra passenger |
| TN | Transport outside the common medical marketing area |
| TU | After-hours transportation |
| TV | Holiday/weekend transportation |
Managed Care Covered Services
Return to Table of Contents
The following links will assist providers in identifying services covered by various government sponsored managed care products available in New York State. These links can also be found in each provider's Medicaid Provider Manual under "Information for All Providers," "Managed Care Information."
| Plan Type Abbreviation | Plan Type - Description | Link |
|---|---|---|
| Partial LTC | Long Term Care: Partial Capitation Managed Long Term Care | http://www.nyhealth.gov/health_care/managed_care/mltc/pdf/mltc_contract.pdf. See Appendix G |
| LTC | Long Term Care: PACE (Program of All-Inclusive Care for the Elderly) | http://www.nyhealth.gov/health_care/managed_ care/mltc/pdf/pace_model_contract.pdf. No list of benefits included - the PACE benefit package includes all Medicare and Medicaid covered services, and other services determined necessary by the interdisciplinary team for the care of the PACE participant. |
| MA Adv Plus | Medicaid Advantage Plus | http://nyhealth.gov/health_care/managed_ care/mltc/pdf/map_model_contract.pdf. See Appendix K |
| PCMP | Physician Case Management Program | Available upon request by calling the Bureau of Program Planning and Implementation at: (518) 473-0122 |
| Mainstream | Medicaid Managed Care/Family Health Plus/HIV Special Needs Plan | http://nyhealth.gov/health_care/managed_care/docs/medicaid_managed_care_fhp_hiv-snp_model_contract.pdf. See Appendix K |
| MA Advantage | Medicaid Advantage | http://www.nyhealth.gov/health_care/managed_ care/docs/medicaid_advantage_model_contract.pdf. See Appendix K |
Questions concerning covered services for Medicaid managed care, HIV SNP, PCMP and Family Health Plus plans can be directed to (518) 473-0122. Questions concerning covered services for Medicaid Advantage, Medicaid Advantage Plus, Partial Capitation Long Term Care and PACE plans can be directed to (518) 474-6965.
Medicaid Coverage and Billing Requirements for Risperdal Consta, Invega Sustenna &
Zyprexa Relprevv
Return to Table of Contents
With the availability of new injectable atypical antipsychotics, and a change in FDA approved indications for Risperdal Consta, the Medicaid program, in consultation with the NYS Office of Mental Health has reviewed and revised the policy on coverage and billing of these products.
Effective for dates of service on or after January 1, 2011, Medicaid will no longer require that providers obtain prior authorization when administering Risperdal Consta. In addition, Medicaid will provide reimbursement for two additional long-acting, extended-release injectable antipsychotics, Invega Sustenna and Zyprexa Relprevv. As with Risperdal Consta, prior authorization will not be required for the use of these drugs.
Note: To allow for the necessary eMedNY system changes, claims for these drugs should be held and submitted after February 1, 2011.
INDICATIONS FOR USE:
For specific indications, dosing, adverse effects and special requirements for these drugs, see the complete FDA-approved prescribing information.
SETTINGS IN WHICH THESE DRUGS CAN BE PROVIDED and BILLED:
- Practitioner offices (physician, nurse practitioner).
- Article 28 clinics (hospital based outpatient departments and free standing diagnostic and treatment centers).
- Article 31 programs including clinic, continuing day treatment, partial hospitalization, Assertive Community Treatment (ACT) teams and Personalized Recovery Oriented Services (PROS).
DRUG ACQUISITION:
Medicaid policy requires providers and practitioners to:
- Purchase the drug;
- Administer the drug to the Medicaid enrollee/patient;
- Bill Medicaid for the drug.
Since practitioner-administered drugs typically require special care, storage and handling by a medical professional, it is not appropriate for the practitioner to write a prescription for the patient to obtain these drugs at a community pharmacy. They are, therefore, covered under the Medicaid program as physician-administered drugs ONLY, and are not included on the Medicaid Pharmacy List of Reimbursable Drugs.
These drugs are carved-out of the Medicaid Managed Care benefit package and should be billed to Medicaid Fee-for-Services (FFS). For Family Health Plus (FHP) enrollees, these drugs remain part of the FHP benefit, as a physician service, and should be billed to the health plan.
BILLING INSTRUCTIONS:
The following chart provides setting-specific guidance on how to bill for these drugs.
| Risperdal Consta | Invega Sustenna | Zyprexa Relprevv | |
|---|---|---|---|
| HCPCS code J2794 | HCPCS code J2426 | HCPCS code J2358 | |
| Practitioner Offices |
Bill J2794 (cost) AND 96372 (for administration) | Bill J2426 (cost) AND 96372 (for administration) | Bill J2358 (cost) AND 96372 (for administration) |
|
|||
| Article 28 Clinics & Article 31 OMH Licensed Programs including: Clinic Continuing Day Treatment Partial Hospitalization Assertive Community Treatment (ACT) teams Personalized Recovery Oriented Services (PROS) |
Risperdal Consta | Invega Sustenna | Zyprexa Relprevv |
| Bill J2794 (cost) AND 96372 (for administration) | Bill J2426 (cost) AND 96372 (for administration) | Bill J2358 (cost) AND 96372 (for administration) | |
|
|||
ARTICLE 31 PROGRAMS:
Please Note:
- If you are administering the drug only, bill the J-code for the drug with the administration code, 96372.
- If you are billing for Injectable Psychotropic Medication Administration with Monitoring and Education, bill H2010 (to APGs). The duration of the service must be at least 15 minutes.
- The drug administration code (96372) cannot be billed in addition to H2010.
- H2010 cannot be billed when these services are provided by an LPN.
QUESTIONS:
Please direct policy questions to the following areas:
For Article 28 and Practitioner questions, please call (518) 473-2160.
For Article 31/Office of Mental Health questions, please call (518) 474-6911.
Billing Questions? Please contact the eMedNY Call Center at (800) 343-9000.
Treatment for Recurrent Diaper Rash
Return to Table of Contents
Skin protectants such as zinc oxide are commonly used for either prevention or treatment of diaper rash or diaper dermatitis. They provide a barrier which protects the skin against external irritants and moisture and additionally provides lubrication to reduce friction which may exacerbate skin irritation.
Diaper rash is a common skin condition that affects most pediatric patients. It can be caused by but is not limited to diaper-area irritants such as soap residue, detergents, perfumes, pre-moistened baby wipes;1 and the use of unnecessary baby products such as powders, creams, lotions and oils, on the bottom2.
Recommended treatment options from the American Academy of Dermatology2 for recurrent diaper rash include some of the following measures:
- Using a warm washcloth instead of pre-moistened wipes.
- Applying a barrier cream with zinc oxide and keeping the diaper area exposed to air for as long as possible.
Zinc oxide is available through the Medicaid program.
For a complete list of medications covered by the Medicaid program, please visit the eMedNY Website at: http://www.emedny.org/info/formfile.html
References are available at the American Academy of Dermatology Website:
1http://www.aad.org/public/conditions/_doc/di_spring03.pdf.
2http://www.aad.org/media/background/factsheets/fact_mommy_skin.html
New York Medicaid Provides In-Service Education
Return to Table of Contents
Education Specialists can provide presentations on the following programs:
- Preferred Drug Program (PDP)
- Clinical Drug Review Program (CDRP)
- Mandatory Generic Drug Program (MGDP)
- Preferred Diabetic Supply Program (PDSP)
Call (518) 951-2051 or e-mail NYPDPNotices@magellanhealth.com today to set up an in-service at your facility.
For questions on the Preferred Drug Program, please call: (877) 309-9493.
For questions on billing, please call: (800) 343-9000.
Providers should visit www.emedny.org (click on Training) to register for a 5010 seminar.
For questions on Medicaid pharmacy policy and operations, please call:
(518) 486-3209 or e-mail: ppno@health.state.ny.us
X12 Version 5010 Medicaid Update Special Edition Soon Available
Return to Table of Contents
In January 2011 the Department will publish a X12 Version 5010 Special Edition Medicaid Update. The Special Edition will provide extensive information that will assist providers and vendors in developing their 5010 implementation strategies. The transition to the 5010 transaction standards will require significant changes to billing software and providers' business processes. Providers are encouraged to begin communication with their software vendor or billing service to ensure their systems will be 5010 compliant by January 1, 2012.
In addition to the Special Edition Medicaid Update the Department and Computer Sciences Corporation (CSC) have developed a comprehensive 5010 communication plan that will include Webinars, regional training seminars, vendor presentations and a host of other communication/education methods.
Please visit the eMedNY Website at: www.emedny.org for a listing of 5010 FAQs, billing requirements, and companion guides.
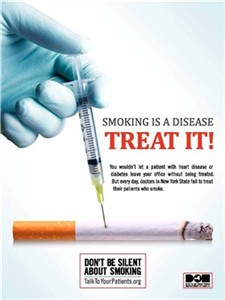
By providing counseling, pharmacotherapy, and referrals, you can double your patients' chances of successfully quitting. For more information, please visit www.talktoyourpatients.org or call the NY State Smokers' Quitline at 1-866-NY-QUITS (1-866-697-8487).
Do you suspect that a Medicaid provider or an enrollee has engaged in fraudulent activities?
Return to Table of Contents
Please Call: 1-877-87FRAUD or (212 417-4570)
Your call will remain confidential.
You can also complete a Complaint Form online at:
www.omig.state.ny.us

Provider Directory
Return to Table of Contents
Office of the Medicaid Inspector General:
http://www.omig.state.ny.us or call (518) 473-3782 with general
inquiries or 1-877-87FRAUD with suspected fraud complaints or allegations.
This contact information can also be used for Provider Self-Disclosures.
Questions about billing and performing MEVS transactions?
Please contact eMedNY Call Center at: (800) 343-9000.
Provider Training
To sign up for a provider seminar in your area, please enroll online at:
http://www.emedny.org/training/index.aspx
For individual training requests, call (800) 343-9000 or email: emednyproviderrelations@csc.com
Enrollee Eligibility
Call the Touchtone Telephone Verification System at any of the numbers below:
(800) 997-1111 (800) 225-3040 (800) 394-1234.
Address Change?
Questions should be directed to the eMedNY Call Center at: (800) 343-9000.
Fee-for-Service Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Rate-Based/Institutional Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Does your enrollment file need to be updated because you've experienced a change in ownership?
Fee-for-Service Providers please call (518) 402-7032
Rate-Based/Institutional Providers please call (518) 474-3575
Comments and Suggestions Regarding This Publication?
Please contact the editor, Kelli Kudlack, at:
medicaidupdate@health.state.ny.us
Medicaid Update is a monthly publication of the New York State Department of Health containing information regarding the care of those enrolled in the Medicaid Program.