October 2010 Volume 26, Number 12
New York State Medicaid Update
The official newsletter of the New York Medicaid Program
David A. Paterson, Governor
State of New York
Richard F. Daines, M.D. Commissioner
New York State DOH
Donna J. Frescatore, Medicaid Director & Deputy Commissioner
Office of Health Insurance Programs

In this issue....
POLICY AND BILLING GUIDANCE
Mandatory Compliance Program Certification Required by 12/31/10
Mandatory Medicaid Managed Care Expanding To Additional Counties
Medicaid Managed Care Now Available in Lewis and Wyoming Counties
Providers of Family Planning Services to Enrollees in the Family Planning Benefit Program (FPBP
No Additional Compensation Allowed for Nursing Home Residents Receiving Transportation Services
Bariatric Surgery Reimbursement for Fee-For-Service Beneficiaries
Medicaid Fee-For-Service Coverage of Seasonal Flu and Pneumococcal Immunizations
PHARMACY UDATES
UPDATE: Prescriber's National Provider Identifier (NPI)
Pharmacists as Immunizers
Use of NCPDP (408-D8) Dispense as Written/Product Selection Code '5' Substitution Allowed
2011 New York State Medicare Part D Prescription Drug Plans
ALL PROVIDERS
Smoking Cessation Advertisement
Provider Directory
Mandatory Compliance Program
Certification Required by 12/31/10
Return to Table of Contents
Social Services Law (SSL) §363-d and Part 521, of Title 18 of the New York State Codes, Rules, and Regulations, both entitled Provider Compliance Programs, is being actively enforced by the Office of the Medicaid Inspector General (OMIG) in 2010. This regulation requires that all Medicaid providers who fall under the following categories, certify that they have adopted and implemented an effective compliance program by December 31, 2010:
- persons subject to the provisions of Articles 28 or 36 of the New York State Public Health Law;
- persons subject to the provisions of Articles 16 or 31 of the New York State Mental Hygiene Law; or
- other persons, providers, or affiliates who provide care, services or supplies under the Medicaid program, or persons who submit claims for care, services or supplies for or on behalf of another person or provider for which the Medicaid program is or should be reasonably expected by a provider to be a substantial portion of their business operations.
Under 18 NYCRR §521.2(b), "substantial portion" of business operations is defined as any of the following:
- when a person, provider, or affiliate claims or orders, or has claimed or has ordered, or should be reasonably expected to claim or order at least $500,000 in any consecutive 12-month period from the medical assistance program;
- when a person, provider, or affiliate receives or has received, or should be reasonably expected to receive at least $500,000 in any consecutive 12-month period directly or indirectly from the medical assistance program; or
- when a person, provider, or affiliate who submits or has submitted claims for care, services, or supplies to the medical assistance program on behalf of another person or persons in the aggregate of at least $500,000 in any consecutive 12-month period.
Each compliance program must contain the eight elements required under SSL §363-d and 18 NYCRR §521.3(c). When applying for enrollment in the medical assistance program, and during the month of December each year thereafter, 18 NYCRR §521.3(b) requires that providers certify to the Department of Health and OMIG that a compliance program meeting the requirements of the regulation is in place. The annual deadline each year for providers to certify that they have an effective compliance program is December 31.
The regulation, certification form, and FAQ's are available on the OMIG Website at: http://www.omig.ny.gov. Under the "Compliance" tab on OMIG's home page click on "Provider Compliance" to access this information. Questions? Please contact the Bureau of Compliance at (518) 402-1116.
Mandatory Medicaid Managed Care
Expanding To Additional Counties
Return to Table of Contents
Effective October 1, 2010, managed care enrollment will be required for most Medicaid beneficiaries residing in Cayuga, Essex, Hamilton, Madison, Schoharie, Tompkins, and Wayne Counties. Once a mandatory managed care program is implemented in a county, it is expected that the enrollment of all eligible Medicaid beneficiaries will take up to 18 months to complete.
Providers should check the Medicaid Eligibility Verification System (MEVS) prior to rendering services to determine Medicaid eligibility and the conditions of Medicaid coverage. Providers are strongly encouraged to check eligibility at each visit as eligibility and enrollment status may change at any time. If the Medicaid beneficiary is enrolled in a Medicaid managed care plan, the first coverage message will indicate "Managed Care Coordinator" or "Eligible PCP" (depending on the device used).
MEVS will identify the scope of benefits a Medicaid beneficiary's Medicaid managed care organization provides through specific coverage codes. When using a touch-tone telephone you will hear the "Description" of each covered service. When using either the Point of Service (POS) or ePACES the "coverage codes" will be displayed. If the message "All" appears, all services will be covered.
Medicaid will not reimburse a provider on a fee-for-service basis if MEVS indicates that the service is covered by the plan.
Providers may call the eMedNY Call Center at (800) 343-9000 with any Medicaid billing issues. Medicaid beneficiaries may contact their local department of social services to learn more about managed care.
Questions? Please contact the Division of Managed Care, Bureau of Program Planning & Implementation at (518) 473-1134.
Medicaid Managed Care Now
Available in Lewis and Wyoming
Counties
Return to Table of Contents
Most Medicaid beneficiaries residing in Lewis and Wyoming counties now have the option to enroll in Medicaid Managed Care. New York State Catholic Health Plan (Fidelis) is now available in these counties for both Medicaid Managed Care and Family Health Plus.
Providers should check the Medicaid Eligibility Verification System (MEVS) prior to rendering services to determine Medicaid eligibility and the conditions of Medicaid coverage. Providers are strongly encouraged to check eligibility at each visit as eligibility and enrollment status may change at any time. If the Medicaid beneficiary is enrolled in a Medicaid managed care plan, the first coverage message will indicate "Managed Care Coordinator" or "Eligible PCP" (depending on the device used). If they are enrolled in a Family Health Plus (FHP) plan, the first coverage message will indicate "Family Health Plus."
MEVS will identify the scope of benefits a Medicaid beneficiary's Medicaid Managed Care Organization provides through specific coverage codes. When using a touch-tone telephone you will hear the "Description" of each covered service. When using either the Point of Service (POS) or ePACES the "Coverage Codes" will be displayed. If the message "All" appears, all services will be covered.
Medicaid will not reimburse a provider on a fee-for-service basis if MEVS indicates that the service is covered by the plan.
Providers may call the eMedNY Call Center at (800) 343-9000 with any Medicaid billing issues. Medicaid beneficiaries should contact their local department of social services to learn more about managed care.
Questions? Please contact the Division of Managed Care, Bureau of Program Planning & Implementation at (518) 473-1134.
Providers of Family Planning Services to Enrollees in the Family Planning Benefit Program (FPBP)
Return to Table of Contents
The Centers for Medicare and Medicaid Services (CMS), recently approved additional procedures considered to be family planning related and are covered for enrollees in FPBP. These procedures are considered family planning when provided during a family planning visit or during a follow-up visit when the procedure is related to the initial family planning visit.
The CPT codes for the additional procedures include:
- 00851 Anesthesia for intraperitoneal procedures in lower abdomen including tubal ligation/transaction.
- 00952 Anesthesia for vaginal procedures(including biopsy of labia, vagina, cervix, or endometrium); hysteroscopy and/or hysterosalpingography.
- 17110 Destruction of flat warts, molluscum contagiosum, or milia; up to 14 lesions.
- 17111 Destruction of flat warts, molluscum contagiosum, or milia; up to 15 or more lesions.
- 85048 Blood count; leukocyte (WBC), automated.
- 87340 Infectious agent antigen detection by enzyme immunoassay technique, qualitative or semiquantitative multiple step method; HIV-1.
- 87510 Infectious agent detection by nucleic acid (DNA or RNA); Gardnerella vaginalis, amplified probe technique.
- 87536 Infectious agent detection by nucleic acid (DNA or RNA); HIV-1, quantification.
- 87798 Infectious agent detection by nucleic acid (DNA or RNA), not otherwise specified; amplified probe technique, each organism.
- 87808 Infectious agent antigen detection by immunoassay with direct optical observation; trichomonas vaginalis.
- 96372 Therapeutic, prophylactic or diagnostic injection (specify substance or drug); subcutaneous or intramuscular.
- 99050 Services provided in the office at times other than regularly scheduled office hours, or days when the office is normally closed (e.g., holidays, Saturday or Sunday), in addition to basic service.
- 99051 Service(s) provided in the office during regularly scheduled evening, weekend, or holiday office hours, in addition to basic service.
A complete list of all approved procedures under the FPBP is available online at: http://www.emedny.org/ProviderManuals/communications/List_CMS_Approved_FP_Procedures_FPBP_Sept_2010_MA%20Update10-06-10.pdf.
Billing procedure guidelines under the FPBP are available for viewing online at:
- http://www.nyhealth.gov//health_care/medicaid/program/update/2008/2008-02.htm.
- http://www.nyhealth.gov//health_care/medicaid/program/update/2008/2008-05.htm#pha.
- http://www.nyhealth.gov//health_care/medicaid/program/update/2008/2008-09.htm#rei.
Questions? Please contact the Bureau of Policy Development and Coverage at (518) 473-2160 or via e-mail to: pffs@health.state.ny.us.
No Additional Compensation Allowed for Nursing Home Residents Receiving Transportation Services
Return to Table of Contents
A number of nursing home administrators have inquired as to whether Medicaid residents or their families may be charged a fee when a nursing home staff member accompanies a resident to and from medical appointments outside the facility. Example: Nursing home personnel travel with a resident to a medical appointment to provide necessary personal care services or ensure effective communication between residents and practitioners. Nursing homes are prohibited from seeking monetary compensation from Medicaid residents or their family members.
The fee-for-service reimbursement paid by Medicaid to transportation and medical providers is considered payment in full for all services rendered to the beneficiary both during transit and at the medical appointment. No additional compensation should be sought or accepted.
Questions? Please contact the Medicaid Transportation Policy Unit at (518) 473-2160, or via e-mail to MedTrans@health.state.ny.us.
Bariatric Surgery Reimbursement
for Fee-For-Service Beneficiaries
Return to Table of Contents
Effective December 1, 2010, only certain hospitals will be permitted to provide surgical services to Medicaid fee-for-service beneficiaries requiring bariatric surgery. Section 21, Part E, Chapter 63 of the Laws of 2005 gives the Commissioner of Health the authority to negotiate rates of payment for specialty inpatient services provided to Medicaid fee-for-service beneficiaries in designated areas of the State. Bariatric surgery was selected as one of the specialty services and New York City as one of the service areas. The following five hospitals were selected and will be designated by the NYS Department of Health as Bariatric Specialty Centers:
New York City Hospitals:
- Harlem Hospital Center (Manhattan)
- St. Luke's Roosevelt (Manhattan)
- Brookdale Medical Center (Brooklyn)
- Lutheran Medical Center (Brooklyn)
- Montefiore Medical Center (Bronx)
Effective December 1, 2010, only these NYC hospitals will be reimbursed for bariatric surgical services for Medicaid fee-for-service recipients.
Also effective December 1, 2010, only non-NYC hospitals that meet Center for Medicare and Medicaid Services' (CMS) minimum facility standards and are designated either by the American College of Surgeons and/or the American Society for Metabolic and Bariatric Surgery as a Medicare Approved Facility for Bariatric Surgery, will be reimbursed for bariatric surgical services for Medicaid fee-for-service beneficiaries. As of October 2010, the following hospitals have this designation:
Rest of the State Hospitals:
- Adirondack Medical Center (Saranac Lake)
- Albany Medical Center (Albany)
- Arnot Ogden Medical Center (Elmira)
- Bon Secours Community Hospital (Port Jervis)
- Ellis Hospital (Schenectady)
- Faxton -St. Lukes Healthcare (Utica)
- Good Samaritan Hospital (Suffern)
- Good Samaritan Hospital Medical Center (West Islip)
- Highland Hospital (Rochester)
- John T. Mather Memorial Hospital (Port Jefferson)
- Kaleida Health, Buffalo General (Buffalo)
- Lawrence Hospital Center (Bronxville)
- Mary Imogene Bassett Hospital (Cooperstown)
- Mercy Medical Center (Rockville Centre)
- North Shore University Hospital at Manhasset
- Peconic Bay Medical Center (Riverhead)
- Sisters of Charity Hospital (Buffalo)
- Sound Shore Medical Center of Westchester (New Rochelle)
- South Nassau Communities Hospital (Oceanside)
- St. Catherine of Siena Medical Center (Smithtown)
- SUNY Upstate Medical University (Syracuse)
- Syosset Hospital (Syosset)
- Westchester Medical Center (Valhalla)
- Winthrop University Hospital (Mineola)
The listing of designated approved facilities should be checked prior to scheduling bariatric surgery for any Medicaid fee-for-service beneficiary. Please see: www.cms.hhs.gov/MedicareApprovedFacilitie/bsf/list.asp.
Questions? Please contact the Bureau of Outcomes Research, Division of Quality and Evaluation at (518) 486-9012.
Medicaid Fee-For-Service Coverage of Seasonal Flu and Pneumococcal Immunizations
Return to Table of Contents
New York Medicaid will reimburse enrolled office-based practitioners, pharmacies, and Article 28 clinic providers for the cost of the seasonal flu and pneumococcal vaccines and for the administration of these vaccines. The fee-for-service coverage policies and billing rules for seasonal flu and pneumococcal vaccines have been specifically designed to facilitate improved access to these vaccines and are outlined as follows:
- Medicaid will cover the cost of seasonal flu and pneumococcal vaccines and the administration of these vaccines.
- Medicaid continues to reimburse clinics, physicians and pharmacies $13.23 for vaccine administration. Nurse practitioners and licensed midwifes continue to be reimbursed $11.25 for vaccine administration.
- Administration of seasonal flu and pneumococcal vaccines may be provided in Article 28 clinic settings; in a practitioner's office by a physician, physician's assistant, nurse practitioner, licensed midwife, registered nurse or licensed practical nurse; or, for ages 18 and older, in a pharmacy by certified pharmacists (within their respective scopes of practice under the State Education Law).
Fee-For-Service Billing Instructions for Article 28 Clinics
When provided in an Article 28 hospital outpatient department or free-standing diagnostic and treatment center clinics (including school based health centers, county health department clinics, Federally Qualified Health Centers and part time clinics), seasonal flu and pneumococcal vaccine administration charges and vaccine charges, if applicable, must be billed as an ordered ambulatory service. These services should NOT be billed as a clinic visit or as part of a clinic visit. Hospital-based clinics are category of service code 0282 and free-standing diagnostic and treatment clinics are category of service code 0163 to denote an ordered ambulatory service other than lab when submitting claims for vaccine administration and vaccine. If these services can be covered by Medicare or another third party insurance coverage, such benefits must be exhausted prior to billing Medicaid.
Seasonal flu and pneumococcal vaccines are billable to Medicaid at their actual acquisition costs for persons aged 19 and older. These vaccines are not billable to Medicaid for those under age 19 as they are provided free of charge through the Vaccines for Children Program. Fees for administration of the seasonal flu and pneumococcal vaccine for each age group and instructions for billing are provided in the chart below.
Medicaid Article 28 Clinic FFS Billing Chart
| Immunization Type | Code For Vaccine | Code for Administration | Medicaid Reimbursement for Vaccine | Medicaid Reimbursement for Administration | Vaccine for Children Program (VFC) |
|---|---|---|---|---|---|
| Age 19 and older | Up to Age 19 | ||||
| Seasonal Flu | 90655 90656 90657 90658 90660 |
G0008 for intramuscular administration 90473 for intranasal or oral administration |
Actual Acquisition Cost | $13.23 $8.57 |
Enhanced administration fee of $17.85 Bill vaccine procedure code as an ordered ambulatory service and append with "SL" modifier (do not bill an administration code) |
| Pneumococcal | 90669 90732 |
G0009 for intramuscular administration | Same as Above | $13.23 | Same as Above |
Fee-For-Service Billing Instructions for Office-Based Practitioners
When provided in a practitioner's office as a standalone service or as part of an evaluation and management visit, vaccine administration charges and vaccine charges, if applicable, must be billed using the Medicaid fee schedule. Seasonal flu and pneumococcal vaccines are billable to Medicaid at their actual acquisition costs for persons aged 19 and older. If these services can be covered by Medicare or another third party insurance coverage, such benefits must be exhausted prior to billing Medicaid.
These vaccines are not billable to Medicaid for those under age 19 as they are provided free of charge through the Vaccines for Children Program. Fees for administration of the seasonal flu and pneumococcal vaccines for those 19 and older and those under age 19 are provided in the chart below. The chart also outlines vaccine procedure codes, vaccine specific administration codes, and Medicaid reimbursement for the vaccines and their administration.
Medicaid Office-Based Practitioner FFS Billing Chart
| Immunization Type | Code For Vaccine | Code for Administration | Medicaid Reimbursement for Vaccine | Medicaid Reimbursement for Administration (Amount varies based on billing provider) | Vaccine for Children Program (VFC) |
|---|---|---|---|---|---|
| Age 19 and older | Up to Age 19 | ||||
| Seasonal Flu | 90655 90656 90657 90658 90660 |
G0008 for intramuscular administration 90473 for intranasal or oral administration |
Actual Acquisition Cost | $13.23 - physician $11.25 - nurse practitioner or licensed midwife $8.57 - physician $7.28 - nurse practitioner or licensed midwife |
Enhanced administration fee of $17.85 Bill vaccine procedure code as an ordered ambulatory service and append with "SL" modifier (do not bill an administration code) |
| Pneumococcal | 90669 90732 |
G0009 for intramuscular administration | Same as Above | $13.23 - physician $11.25 - nurse practitioner or licensed midwife |
Same as Above |
Billing questions? Please call (800) 343-9000. For policy questions, please call (518) 473-2160.
UPDATE: Prescriber's National
Provider Identifier (NPI)
Return to Table of Contents
Attention Prescribers and Pharmacists:
Since September 1, 2008, New York Medicaid has required the submission of the Prescriber National Provider Identifier (NPI). Effective December 2, 2010, New York Medicaid will implement claims editing to enforce the submission of the Prescriber's NPI with pharmacy claims.
Pharmacists:
Beginning December 2, 2010, all pharmacy claims should include the Prescriber NPI in the Prescriber ID field (411-DB) and a "01" in the Provider ID Qualifier field (465-EY). Pharmacy claims submitted with a prescriber's MMIS Provider ID number or profession code and license number will be denied for edit 02029 - "Missing Prescribing NPI."
Prescribers:
The NPI number is currently being imprinted on prescription pads for practitioners who have provided their NPI number to the New York State Official Prescription Program. If the number has already been provided, it will be listed in the online 'profile.'
- Practitioners may send an e-mail to: narcotic@health.state.ny.us and provide their NPI number to the New York State Official Prescription Program. Please include the name, state license number and NPI number in the e-mail. The NPI number will also be requested during the registration process.
NOTE: While providing a NPI to the prescription program is optional, doing so will ensure that the dispensing pharmacy can efficiently meet claims submission requirements.
Alternatively, a practitioner may write or stamp their NPI number on the official prescription.
For practitioners who wish to obtain a NPI number, please contact the NPI registry at (800) 465-3203 or visit:
https://nppes.cms.hhs.gov/NPPES/StaticForward.do?forward=static.npistart
For questions relating to the New York State Official Prescription Program, please call (866) 772-4683. For pharmacy billing questions, please call (800) 343-9000.
Pharmacists as Immunizers
Return to Table of Contents
The administration of select vaccines by qualified pharmacists employed by, or under contract with, Medicaid enrolled pharmacies is reimbursable under the New York Medicaid program. Administration of vaccines is conducted pursuant to NYS Education Law and regulations (8NYCRR63.9) which permits licensed pharmacists who obtain additional certification to administer influenza and pneumococcal vaccinations to adults 18 years of age and older.
The following conditions apply:
- Only Medicaid enrolled pharmacies that employ or contract with NYS certified pharmacists to administer vaccines will receive reimbursement for immunization services and products. Each pharmacist certified to administer immunizations will receive a new registration certificate that will contain the prefix "I". Pharmacy interns cannot administer immunizations in New York State.
- Services must be provided and documented in accordance with NYS Department of Education laws and regulations. Please visit: http://nyhealth.gov/health_care/medicaid/program/pharmacists_as_immunizers/fact_sheet_10-14-10.htm for additional information.
- This information only applies to Medicaid fee-for-service beneficiaries. Medicaid Managed Care and Family Health Plus beneficiaries continue to access immunization services through their health plans. Pharmacists should check with the beneficiary's health plan before immunizing to determine the health plan's coverage policy regarding immunizations provided by pharmacists.
- Reimbursement is based on a patient specific or non-patient specific order. These orders must be kept on file at the pharmacy. The ordering prescriber's NPI is required on the claim for the claim to be paid.
- Consistent with Medicaid immunization policy for practitioners, pharmacies bill the administration and cost of the vaccine using the following procedure codes. Please note that NDCs are not to be used for billing the vaccine product. Reimbursement for the product will be made at no more than the actual acquisition cost to the pharmacy. No dispensing fee or enrollee co-payment applies. Pharmacies will bill with a quantity of "1" and a day supply of "1".
| Procedure Code | Procedure Description |
|---|---|
| 90656 | Seasonal Influenza virus vaccine, preservative free, for intramuscular use |
| 90658 | Seasonal Influenza virus vaccine, for intramuscular use |
| 90660 | Seasonal Influenza, live, for intranasal use |
| 90732 | Pneumococcal vaccine, for intramuscular use |
| G0008 | Administration of seasonal influenza virus vaccine, intramuscular use |
| 90473 | Administration of seasonal influenza intranasal vaccine |
| G0009 | Administration of pneumococcal vaccine |
- The Seasonal Flu vaccine and Pneumococcal vaccine for individuals under the age of 19 are provided free of charge by the Vaccines for Children (VFC) program. Therefore, Medicaid will not reimburse providers for these vaccines for individuals under the age of 19. For VFC enrollment information, please visit: http://nyhealth.gov/prevention/immunization/vaccines_for_children.htm.
The following chart describes the codes and fees that are reimbursable to pharmacies.
| Immunization Type | Code For Vaccine | Code for Administration | Medicaid Reimbursement for Vaccine | Medicaid Reimbursement for Administration (Amount varies based on billing provider) | Vaccine for Children Program (VFC) |
|---|---|---|---|---|---|
| Age 19 and older | Up to Age 19 | ||||
| Seasonal Flu | 90656 90658 90660 |
G0008 for intramuscular administration 90473 for intranasal or oral administration |
Actual Acquisition Cost | $13.23 $8.57 |
$13.23 Bill vaccine administration code only (do not bill vaccine procedure code) $8.57 Bill vaccine administration code only (do not bill vaccine procedure code) |
| Pneumococcal | 90732 | G0009 for intramuscular administration | Same as Above | $13.23 | $13.23 Bill vaccine administration code only (do not bill vaccine procedure code) |
The maximum fees for these drugs are adjusted periodically by the State to reflect the estimated acquisition cost. Insert acquisition cost per dose in amount charged field on claim form.
Questions? Please contact the Medicaid Pharmacy Program at (518) 486-3209 or via e-mail to: PPNO@health.state.ny.us. Additional information on influenza is available online at: http://nyhealth.gov/diseases/communicable/influenza/. For billing questions, please call (800) 343-9000.
Use of NCPDP (408-D8) Dispense as Written/Product Selection Code '5' Substitution Allowed - Brand Dispensed as Generic
Return to Table of Contents
340B Pharmacy Providers
Claims submitted by 340B providers with a "5" in the NCPDP Dispense as Written/Product Selection Code Field (408-D8) AND a "9" in the NCPDP Basis of Cost Determination Field (423-DN) will bypass any of the prior authorization requirements associated with the Preferred Drug and Mandatory Generic Drug Programs. When using these options, the 340B price must be billed to the
Effective October 21, 2010, pharmacies that use a multi-source brand name drug as their most cost-effective option will be able to use a "5" in the NCPDP Dispense as Written/Product Selection Code Field (408-D8) to receive generic drug reimbursement, including the application of generic drug dispensing fee and copayment.
Note: When dispensing a multi-source brand name drug included in the Brand Less Expensive than Generic Program, the claim does not require a "5" in the NCPDP Dispense as Written/Product Selection Code Field (408-D8). Reimbursement for these drugs does not require submission of a particular "DAW" code. However, the appropriate "DAW" code should be used to accurately denote whether the prescriber indicated "Dispense as Written" on the prescription.
The current list of multi-source brand name drugs included in the Brand Less Expensive than Generic Program is available online at: http://www.nyhealth.gov/health_care/medicaid/program/docs/bltg.pdf.
Information regarding Medicaid pharmacy reimbursement is available online at: http://www.nyhealth.gov/health_care/medicaid/program/docs/pharmacy_reimbursement.pdf.
Information regarding the Preferred Drug and Mandatory Generic Drug Programs is available online at: https://newyork.fhsc.com/ or by calling (877) 309-9493.
For billing questions, please call (800) 343-9000.
2011 New York State Medicare Part D Prescription Drug Plans for People with both Medicare and NYS Medicaid
Return to Table of Contents
The following is a list of the 2011 Medicare Prescription Drug Plans available at no cost to individuals with both Medicare and New York State Medicaid. Other plans offered by these companies may require an additional monthly premium payment. Enrollment for the 2011 benefit year begins November 15, 2010. Contact information was updated in October 2010.
- Bravo Health
Bravo Rx - S5998-001
Customer Service (877) 504-7252
www.mybravohealth.com - CIGNA Medicare Rx
Cigna Medicare Rx Plan One S5617-013
Customer Service (800)-735-1459
www.cignamedicarerx.com - EnvisionRx Plus
EnvisionRx Plus Silver - S7694-003
Customer Service (866)-250-2005
www.envisionrxplus.com - HealthSpring Prescription Drug Plan
HealthSpring Prescription Drug Plan Reg 3
S5932-004
Customer Service (800) 331-6293
www.healthspring.com - Humana Ins. Co. of New York
Humana Walmart - Preferred Rx Plan
S5552-004
Customer Service (800) 645-7322
www.humana-medicare.com - Medco Medicare Prescription Plan
Medco Medicare Prescription Plan - Value
S5983-004
Customer Service (800) 758-4531
www.medcomedicare.com - RxAmerica
Advantage Star Plan by RxAmerica
S5644-004
Customer Service (800) 429-6686
www.Meds4Medicare.com - SilverScript Insurance Company
CVS Caremark Value
S5601-006
Customer Service (866) 235-5660
www.silverscript.com - UnitedHealthcare
AARP MedicareRx Preferred
S5805-001
Customer Service (888) 867-5575
www.AARPMedicareRx.com - Universal American
Community CCRx Basic
S5825-045
Customer Service (866) 249-8668
www.universal-american-medicare.com - Wellcare
Wellcare Classic
S5967-140
Customer Service (888) 550-5252
www.wellcarepdp.com
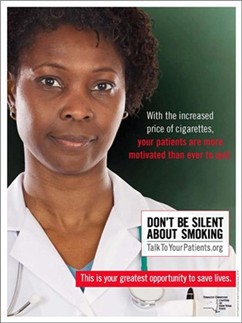
By providing counseling, pharmacotherapy, and referrals, you can double your patients' chances of successfully quitting. For more information, please visit www.talktoyourpatients.org or call the NY State Smokers' Quitline at 1-866-NY-QUITS (1-866-697-8487).
Do you suspect that a Medicaid provider or an enrollee has engaged in fraudulent activities?
Return to Table of Contents
Please Call: 1-877-87FRAUD or (212 417-4570)
Your call will remain confidential.
You can also complete a Complaint Form online at:
www.omig.state.ny.us

Provider Directory
Return to Table of Contents
Office of the Medicaid Inspector General:
http://www.omig.state.ny.us or call (518) 473-3782 with general
inquiries or 1-877-87FRAUD with suspected fraud complaints or allegations.
This contact information can also be used for Provider Self-Disclosures.
Questions about billing and performing MEVS transactions?
Please contact eMedNY Call Center at: (800) 343-9000.
Provider Training
To sign up for a provider seminar in your area, please enroll online at:
http://www.emedny.org/training/index.aspx
For individual training requests, call (800) 343-9000 or email: emednyproviderrelations@csc.com
Enrollee Eligibility
Call the Touchtone Telephone Verification System at any of the numbers below:
(800) 997-1111 (800) 225-3040 (800) 394-1234.
Address Change?
Questions should be directed to the eMedNY Call Center at: (800) 343-9000.
Fee-for-Service Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Rate-Based/Institutional Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Does your enrollment file need to be updated because you've experienced a change in ownership?
Fee-for-Service Providers please call (518) 402-7032
Rate-Based/Institutional Providers please call (518) 474-3575
Comments and Suggestions Regarding This Publication?
Please contact the editor, Kelli Kudlack, at:
medicaidupdate@health.state.ny.us
Medicaid Update is a monthly publication of the New York State Department of Health containing information regarding the care of those enrolled in the Medicaid Program.