August 2010 Volume 26, Number 10
New York State Medicaid Update
The official newsletter of the New York Medicaid Program
David A. Paterson, Governor
State of New York
Richard F. Daines, M.D. Commissioner
New York State DOH
Donna J. Frescatore, Medicaid Director & Deputy Commissioner
Office of Health Insurance Programs

In this issue....
POLICY AND BILLING GUIDANCE
New York State Medicaid Quality Wise Program
Trip Documentation Required of Transportation Providers
Utilization Threshold (UT) Program Update
Attention: Hospitals and Clinics
Office-Based Surgery Practices Update
Preventive Medicine Services Now Billable Under Primary Care Exception
Dialysis Clinics Prescribing Feraheme (Ferumoxytol)
Medicaid Coverage of Mental Health Counseling by LCSWs and LMSWs
Physical and Occupational Therapy Service Providers
Reminder: Gifts, Inducements, and Remuneration Policy
PHARMACY UDATES
Billing Instructions for Physician Administered Drugs (J-codes)
Attention: Prescribers and Pharmacies
Attention: Nursing Homes and Community Pharmacies
Mandatory Generic Drug Program Update
Dispense Brand Name Drugs When Less Expensive Initiative
Attention: Medicaid and Family Health Plus Prescribers
Reminder: Smoking Cessation Policy NYS Medicaid Pharmacy Benefit
Diagnosis Code Requirement
Medicaid & Family Health Plus Prescribers
ALL PROVIDERS
Smoking Cessation Advertisement
New York State Medicaid Quality Wise Program
Return to Table of Contents
In 2009 the New York State Department of Health, Office of Health Insurance Programs, awarded APS Healthcare with a contract to conduct an extensive utilization review of Medicaid fee-for-service payments. The New York State Medicaid Quality Wise Program is focused on promoting quality healthcare and improved outcomes for beneficiaries enrolled in the New York State Medicaid fee-for-service program through retrospective claims analysis and collaboration with the provider community.
Program Goals:
- Increase the use of best practices supported by evidence-based guidelines;
- Enhance patient safety and quality of care;
- Promote appropriate coordination and integration of care for beneficiaries accessing multiple providers;
- Share informed, actionable feedback with providers to improve the health outcomes of their patients;
- Identify under-utilization and over-utilization of services.
Methodology:
Through the use of decision-support analytical tools with imbedded clinical algorithms to extract and identify opportunities for improvement in patterns of care, the New York State Medicaid Quality Wise Program:
- Incorporates measures such as episode groupings, evidence-based measures, predictive models, benchmarking;
- Identifies opportunities for best practice discussions and education with providers;
- Engages providers with key information (clinical and operational) to support patient care.
Current Activities:
- Three chronic disease focused campaigns: diabetes, asthma, and heart failure;
- Campaign outreach includes provider letters, educational calls, and face-to-face educational meetings on provider data reports;
- Provider data reports include: Medicaid fee-for-service patient lists and clinical alerts, patient level report on clinical standards, and patient level report on safety alerts;
- Outreach materials including provider and patient diabetes and asthma care kits.
Program Contact Information:
APS Healthcare, 44 South Broadway, White Plains, New York 10601, 1-866-269-7412 www.nysqualitywise.com
Trip Documentation Required of Transportation Providers
Return to Table of Contents
Transportation providers will only be reimbursed when acceptable records verifying a trip's occurrence are complete and available to auditors upon request.
Ambulance Providers: Ambulance providers are responsible for completing the Pre-Hospital Care Report, which is a complete record of the ambulance trip and satisfies Medicaid's trip documentation requirements.
Ambulette, Taxi, Livery, and Group Ride Providers: For each leg of the trip, verification should be completed at the time of the trip and must include, at a minimum:
- The Medicaid beneficiary's name and Medicaid identification number;
- The date of the transport;
- Both the origination of the trip and time of pickup;
- Both the destination of the trip and time of drop off;
- The vehicle license plate number; and
- The full printed name of the driver providing the transportation.
The new documentation requirements include the time of drop off and the vehicle license plate number. Providers are expected to comply with these two new requirements for dates of service on or after September 1, 2010. This documentation is required for every leg of a trip. A round trip is considered two separate services, with correlating documentation. Although the driver's signature is not required at this time, it is advised that providers include an attestation in the trip documentation that states, "I provided the indicated transportation services," and request the driver's signature.
Providers are urged to maintain a record with all information listed above in case of a Medicaid audit. If any of the information above is lacking, illegible, or false, a claim will be denied. Additionally, the weekly eMedNY issued prior approval roster listing all authorized trips should be reserved.
Note: The following items presented as the only evidence of a trip are not considered acceptable documentation. However, these documents may be considered supplemental to additional required documentation:
- A driver or vehicle manifest, or dispatch sheet;
- An issuance of a prior authorization by the authorizing agent with subsequent checkmarks on a prior authorization roster;
- An attendance log from a day program.
Questions? Please e-mail the Medicaid Transportation Policy Unit at: medtrans@health.state.ny.us.
Utilization Threshold (UT) Program Update
Return to Table of Contents
Effective August 1, 2010, in collaboration with research and clinical experts at the State University of New York (SUNY), another important change took effect in the Medicaid UT program:
- Aligning with the 2009 changes to Physician/Clinic, Pharmacy and Laboratory services, each Medicaid beneficiary is now assigned specific service limits for Mental Health Clinic and Dental Clinic Services.
Refreshed quarterly, the service units are scientifically established based on each beneficiary's clinical information, including diagnoses, procedures, prescription drugs, age and gender. As of October 1, 2010 this data refresh will occur on a monthly basis.
Beneficiary-specific service limits have significantly reduced the need for override requests. TOA requests received without the appropriate medical documentation will be returned to the originating provider for further clarification. A written medical assessment must be provided when additional services are requested. The medical assessment should include a description of the Medicaid beneficiary's medical condition. Without this medical assessment, the request will be returned to the originating provider for the appropriate documentation to justify the increase.
TOA Form Reminders:
- Check eligibility to verify the beneficiary's most up-to-date status;
- Submit requests on eMedNY Form 00104;
- Provider ID - Enter the 10-digit NPI Provider ID number if enrolled in the Medicaid Program. If the Provider is not enrolled, they should leave this field blank;
- Signature - The TOA form must have an original requesting provider signature and date. Rubber stamps, photocopies and carbon-copied signatures will not be accepted. Please print name under signature to assist with any follow-up contact;
- Provider Information: Area Code/Phone/Extension - Please record the Provider's phone number with the area code and any applicable extension. This information is essential to any follow-up contact that may be necessary;
- Providers should contact the eMedNY Call Center at (800) 343-9000 for assistance in obtaining SAs, requesting TOA forms, submitting TOAs or other UT related questions;
- Completed paper TOA forms (eMedNY 000104) should be sent to CSC for processing: Computer Sciences Corporation, PO Box 4602, Rensselaer, New York 12144-4602 ;
- The UT Program Guide is available online at: http://www.emedny.org/HIPAA/Provider_Training/Training.html.
- To obtain SAs, please see the Medicaid Eligibility Verification System Manual at: http://www.emedny.org/providermanuals/index.html.
Attention: Hospitals and Clinics
Return to Table of Contents
Effective July 8, 2010, New York State Medicaid began denying claims if the attending provider's National Provider Identifier (NPI) is not affiliated with the facility. The denial code for these claims is Edit 02067- Attending Provider Not Linked to Billing Provider, which will be reported in the 835 Supplemental File and paper remittances. The HIPAA X12 denial code will be defined as 208/N55.
New York State Medicaid provides two methods for registering NPIs:
Online at: https://npi.emedny.org/Facility/, or via batch by following the instructions on the NYHIPAADESK tab, click on NPI and then Facilities Practitioner's NPI Reporting (Batch Instructions).
Facilities that have a large number of practitioners are encouraged to maintain a "roster" of all their attending providers' NPIs. As updates are made to the roster, please forward them to New York State Medicaid using the batch facilities method (above).
Note: Whenever a facility hires a new practitioner or if a practitioner leaves the facility, they must make certain that the affiliation registration status has been updated or added to the facility's file so that claims will not deny for the edit mentioned above.
Questions? Please contact the eMedNY Call Center at (800) 343-9000.
Office-Based Surgery Practices Update
Return to Table of Contents
Effective July 14, 2009, New York State Medicaid mandated that all office-based surgery practices requiring moderate, deep sedation, or general anesthesia be accredited by one of three approved accrediting bodies designated by the New York State Department of Health. Additional information is available online at: www.nyhealth.gov.
In accordance with this requirement New York Medicaid enrollment applications for physicians, physician assistants, and groups have been updated so that providers can report their office-based surgery accreditation and submit the required documentation. A new form EMEDNY-432501 is now available on the eMedNY Website at www.eMedny.org for new office-based surgery certifications or renewals. It is imperative that office-based surgery practices maintain a current accreditation certificate on file with the New York Medicaid Fee-for-Service Provider Enrollment Bureau.
Please contact the Fee-for-Service Provider Enrollment Bureau at (518) 402-7032 with any questions regarding Office-Based Surgery.
Preventive Medicine Services Now Billable Under Primary Care Exception
Return to Table of Contents
Effective July 1, 2010, New York State Medicaid began reimbursing supervising/teaching physicians for certain preventive medicine services performed by residents under the Primary Care Exception guidelines. The Primary Care Exception is a term used to describe an exception to the requirement that the teaching physician be present during the critical or key portion of a service provided by a resident. This exception currently allows residents in an approved Graduate Medical Education (GME) Program to perform lower and mid-level Evaluation and Management (E/M) services when the teaching physician is not present.
The following is a list of the Preventive Medicine visit codes that will be included for reimbursement under the guidelines of the Primary Care Exception:
| New Patient Preventive Medicine Codes | Established Patient Preventive Medicine Codes |
|---|---|
| 99381 | 99391 |
| 99382 | 99392 |
| 99383 | 99393 |
| 99384 | 99394 |
| 99385 | 99395 |
| 99386 | 99396 |
The supervising physician may bill for these visits when the following Primary Care Exception criteria are met:
- The service must be furnished in a primary care center located in the outpatient department of a hospital or other ambulatory care entity affiliated with an approved GME program.
- The resident, who furnished the billable patient care without the physical presence of the teaching physician, must have completed more than six months of an approved residency program.
In addition, the supervising/teaching physician, who submits claims under the exception, must:
- Supervise no more than four residents/interns at a time;
- Be immediately available and have no other responsibilities at the time the patient is being seen;
- Assume management responsibility for the patient and ensure that the services rendered are reasonable and necessary;
- Review with the resident/intern, during or immediately following each visit, the key elements of the services provided;
- Document the extent of their participation in the review and direction of services.
Note: Medicaid's Primary Care Exception criteria and policy requirements mirror those of Medicare.
For more information on meeting Medicare's Primary Care Exception requirements, please see the Centers for Medicare and Medicaid Services (CMS) Guidelines for Teaching Physicians, Interns and Residents at: http://www.cms.hhs.gov/MLNProducts/downloads/gdelinesteachgresfctsht.pdf.
Billing questions should be directed to the eMedNY Call Center at (800) 343-9000.
Policy questions may be directed to the Bureau of Policy Development and Coverage at (518) 473-2160 or via e-mail to: PFFS@health.state.ny.us.
Dialysis Clinics Prescribing Feraheme (Ferumoxytol)
Return to Table of Contents
The following information clarifies New York Medicaid's policy regarding reimbursement to Article 28 free-standing dialysis clinics and hospital outpatient departments for Feraheme (Ferumoxytol). Feraheme is an injected intravenous iron replacement therapy used in the treatment of iron deficiency anemia in adult patients with chronic kidney disease.
The January 1, 2010 release of a unique Q-code (Q0139) for the reporting and billing of Feraheme (ferumoxytol), for use in patients with end-stage renal disease (ESRD) who are on dialysis, has resulted in inquiries from dialysis providers/clinics regarding New York Medicaid's reimbursement policy for this drug.
Hospital outpatient departments (HOPDs) and free-standing diagnosis and treatment centers (D&TCs) are reimbursed under Ambulatory Patient Groups (APGs). In these settings, Feraheme (Q0139) groups to and is reimbursed under APG 436 (Class II Pharmacotherapy). APG 436 is on the "If Stand Alone, Do Not Pay" list. Feraheme, therefore, will not generate payment under APGs if it is the only service/procedure provided on a given date of service, but will reimburse if other services or procedures are provided.
Prior to APG implementation in hospital OPDs and free-standing D&TCs, NYS Medicaid reimbursed dialysis providers/D&TCs an all-inclusive dialysis clinic rate. All drug costs, including Feraheme, were included in this rate (with the exception of Epogen).
Billing questions? Please contact the eMedNY Call Center at (800) 343-9000.
Medicaid Coverage of Mental Health Counseling by LCSWs and LMSWs Approved for Article 28 Outpatient Hospital Clinics and Free-Standing Diagnostic and Treatment Centers
Return to Table of Contents
Mental health counseling, provided by a licensed clinical social worker (LCSW) or a licensed master social worker (LMSW) in Article 28 outpatient hospital clinics (OPD) and free- standing diagnostic and treatment centers (D&TCs), has been approved by CMS retroactive to September 1, 2009.
Recipient Eligibility:
Medicaid will reimburse for mental health counseling provided by LCSWs/LMSWs to children and adolescents up to 21 years of age and pregnant women up to 60 days post-partum (based on the date of delivery or end of pregnancy).
LMSW Supervision Requirements:
According to Education Law, Article 154 and Regulations of the Commissioner, Part 74, supervision of a licensed master social worker shall be provided by a licensed clinical social worker, a psychologist, or a psychiatrist.
Reimbursement Requirements for LCSW/LMSW:
- A facility must have a psychiatry or psychology certification on its operating certificate;
- Fee-for-service enrollees who are up to the age of 21 are eligible;
- Fee-for-service pregnant women are eligible. There must be a primary or secondary diagnosis of pregnancy (ICD-9 codes: 630-677, V22, V23, and V28) on the claim. Mental health services are also available up to 60 days post-partum with a primary or secondary diagnosis of post-partum depression (ICD-9 codes 648.40 - 648.44);
- Mental health counseling by LCSWs and LMSWs is only available on an individual basis or with family.
Ordering/Documentation Requirements:
Mental health counseling by a LCSW/LMSW must be supported by a written referral from:
- The beneficiary's personal physician, other licensed medical practitioner, or a medical resource, such as a clinic, acting as the beneficiary's physician;
- An appropriate school official;
- An official or voluntary health or social agency.
Children, pregnant women, and families treated via counseling in Article 28 clinics require assessment and treatment for less complex emotional disturbances. As such, the typical course of treatment would be expected to be solution-focused and short term. Children, pregnant women, and families presenting with more complex needs or severe emotional disturbance should be referred to a specialist (i.e., child psychiatrist, licensed psychologist, primary care physician with specialty training/consultation or a clinic licensed by the Office of Mental Health under Article 31 of the Mental Hygiene Law).
In addition to the items that must be maintained in the beneficiary case record as specified in the Clinic Provider Manual, case records must also include at a minimum the following information:
- A treatment plan developed, signed and dated by the social worker that includes, but is not limited to, the beneficiary's diagnosis (only a LCSW can diagnose), the beneficiary's treatment goals, and the number of sessions planned;
- Documentation of the integration of health and behavioral health services;
- Progress notes signed and dated by the social worker for each visit/contact identifying the session content and duration, as well as changes in goals, objectives, and services;
- Periodic assessment signed and dated by the social worker documenting the beneficiary's progress towards goal;
- Documentation of referral for specialty behavioral health care.
Rate Codes:
New rate codes have been established for Hospital Outpatient Department and Diagnostic and Treatment Center reimbursement for mental health counseling when provided by a LCSW/LMSW.
| 4257 | Individual Brief Counseling (psychotherapy which is insight oriented, behavior modifying and/or supportive, approximately 20-30 minutes face-to-face visit with the patient) | $41 |
| 4258 | Individual Comprehensive Counseling (psychotherapy which is insight oriented, behavior modifying and/or supportive, approximately 45-50 minutes face-to-face visit with patient) | $62 |
| 4259 | Family Counseling (psychotherapy with or without patient) | $70 |
New rate codes have been established for School Based Health Center reimbursement for mental health counseling when provided by a LCSW/LMSW.
| 3257 | Individual Brief Counseling (psychotherapy which is insight oriented, behavior modifying and/or supportive, approximately 20-30 minutes face-to-face visit with the patient) | $41 |
| 3258 | Individual Comprehensive Counseling (psychotherapy which is insight oriented, behavior modifying and/or supportive, approximately 45-50 minutes face-to-face visit with patient) | $62 |
| 3259 | Family Counseling (psychotherapy with or without patient) | $70 |
Note: Per State statute, free-standing diagnostic and treatment centers that billed and received Medicaid payment for mental health counseling services provided by licensed social workers in calendar year 2007 may continue to bill Medicaid for such services. Mental Health counseling provided by such clinics is available to all eligible Medicaid enrollees regardless of age or pregnancy status.
Questions? Please contact the Division of Financial Planning and Policy at (518) 473-2160 or via e-mail at: PFFS@health.state.ny.us.
Physical and Occupational Therapy Service Providers
Return to Table of Contents
The Rehabilitation Services manual available online at eMedNY.org has been updated to reflect Rehabilitation Services Policy Guidelines specific to Physical and Occupational Therapy (PT/OT) Services.
These guidelines were established to ensure that PT/OT services provided are consistent with nationally recognized standards, are medically necessary, and are not duplicative in nature. Included in these guidelines are definitions related to PT/OT service provision, coverage criteria, and documentation requirements.
Questions related to any of the above referenced information should be directed to the OHIP Prior Approval Unit at (518) 474-8161 or via e-mail at: OHIPMedPA@health.state.ny.us.
Reminder: Gifts, Inducements, and Remuneration Policy
Return to Table of Contents
The following article is a reprint of information that appeared in the May 2007 Medicaid Update concerning Gifts, Inducements, and Remunerations (any remuneration).
Pharmacies: Under New York State regulations and Board of Regents rules (Part 29) involving pharmacy unprofessional conduct, owners of pharmacies, pharmacists or their employees cannot offer or provide any remuneration to a Medicaid beneficiary if the person knows or should know that the offer or transfer is likely to influence the beneficiary's selection of a provider of Medicaid items or services.
Remuneration can include advertised waiver of co-payments/coinsurance, cash or cash equivalents, gifts such as cell phones, pagers and the transfer of items for free or for other than fair market value. The only potential exception to this policy for pharmacy providers is the provision of an item or device offered or provided to a beneficiary which is directly related to the administration of medication for that person, or waiver of Medicaid co-payments based on the beneficiary's inability to pay. There are no monetary exemptions permitted under the Board of Regent's rules concerning unprofessional conduct.
Other Providers: Other providers should review the rules and regulations for their particular professions regarding the prohibition/regulation of inducements. The failure to adhere to these regulations could result in termination as a Medicaid provider. You should be advised that state policy under 18 NYCRR Part 515, prohibits the furnishing of inducements by a Medicaid provider.
Action: If you suspect that a provider has engaged in any of the activities listed above or any other questionable activity, please call the Medicaid Fraud Hotline at (877) 87FRAUD, (877-873-7283). Your call will remain confidential. OMIG can exclude or terminate the enrollment of any provider that is in violation of this policy.
Questions concerning potential unprofessional conduct by pharmacies? Contact the State Board of Pharmacy at (518) 474-3817.
Are you concerned whether an item or device provided to a Medicaid beneficiary is in support of the administration of medication? Contact the Medicaid Pharmacy Policy and Operations Unit at (518) 486-3209.
Questions concerning the prohibition of inducements and gifts in the Medicaid program? Contact the Office of the State Medicaid Inspector General at (877) 873-7283.
Billing Instructions for Physician Administered Drugs (J-codes) Submitted on Paper Claims
Return to Table of Contents
Effective September 23, 2010, all paper claims (eMedNY 150002) that lack the NDC for physician administered drugs will be denied for edit 02066 Drug Code Missing. New York Medicaid is required to collect federal rebates on physician administered drugs (J-codes). To identify the drug for rebate purposes, the National Drug Code (NDC) information must be identified on the claim.
The eMedNY form includes the following fields in addition to the CPT/HCPCS fields which must be completed:
- Field 20: NDC (found on the drug invoice or product package)
- Field 20A: NDC Unit (of measure)
- Field 20B: NDC Quantity
- Field 20C: Total Cost
Billing Instructions:
The Health Insurance Portability and Accountability Act (HIPAA) standard code set for NDCs is 11digits as a 5-4-2 configuration. Therefore, when entering the NDC on the claim, a leading zero must be added. Where the zero is added depends upon the configuration of the NDC. NEVER ENTER HYPHENS.
| Examples of the NDC and leading zero placements follow: | |
|---|---|
| NDC# Configuration | Correct Leading Zero placement for 5 + 4 + 2 = 11 |
| XXXX XXXX XX 4 + 4 + 2 = 10 | 0XXXX XXXX XX 5 + 4 + 2 = 11 |
| XXXX XXXX XX 5 + 3 + 2 = 10 | XXXXX 0XXX XX 5 + 4 + 2 = 11 |
| XXXX XXXX XX 5 + 4 + 1 = 10 | XXXXX XXXX 0X 5 + 4 + 2 = 11 |
Billing instructions for physician administered drugs
Existing physician administered drug reporting requirements (using the Healthcare Common Procedure Coding System - HCPCS) remain the same. Payment will continue to be based on HCPCS reporting information.
In order to be reimbursed, the physician administered drug (J-code) MUST be on the first line, and only the first line, of Field 24C (Procedure CD). If the drug procedure code is reported on subsequent lines of the claim form, the required NDC code information will not be associated with the drug procedure code and the claim will be denied. Other "non-drug" procedure codes must be entered on line two and below. Multiple drug procedure codes reported for the same date of service must be submitted on separate forms so that the J-code is reported on the first claim line of each claim.
When entering information in Field 20B (NDC Quantity) and 20C (Total Cost), you must overwrite the red decimals (already appearing in the field) with black or blue ink.
In order for Medicaid to reimburse, the labeler/vendor must be a participating rebate signer. A listing of the drug labeler/vendors that participate in the Medicaid Drug Rebate Program is available online at: www.cms.hhs.gov/MedicaidDrugRebateProgram/10_DrugComContactInfo.asp.
Please note that the first five digits of the NDC code represent the labeler/vendor. If the labeler code is not on this list, the labeler's drug is not reimbursable by Medicaid.
Reimbursement will continue to be based on HCPCS reporting information. Ordered ambulatory providers billing Medicaid at 340B prices: Enter a value of UD in fields 24D,E,F or G. When using this option the 340B price must be billed to Medicaid. It is not necessary to enter the NDC information.
If additional eMedNY 150002 forms are needed, please contact the eMedNY Call Center at (800) 343-9000
Attention: Prescribers and Pharmacies
Did you know the list of Medicaid Reimbursable Drugs is available online?
Return to Table of Contents
The list of outpatient drugs available to Medicaid beneficiaries through pharmacies is available online at http://www.emedny.org/info/formfile.html. For more information, please contact the eMedNY Call Center at (800) 343-9000.
This page contains drug information, extracted from the formulary file, which is searchable by a number of fields including description, NDC, and labeler. In addition, the full list may be viewed or downloaded as a PDF file.
Search Tips:
Select the field you wish to use, and then enter your search term in the "Value" field. Enter only one value at a time, using letters and/or numbers. You can use the beginning letters of the name of the drug or value you are searching for but do not use an asterisk ("*") character as a wildcard to search for multiple values. Finally, select the field you would like to use when sorting your matches and click "Search" to begin searching.
PA Code Values:
- PA code "0" = PA not required
- PA code "8" = PA required - Mandatory Generic Drug Program
- PA code "A" = PA required -Non Preferred Drug
- PA code "B" = PA required -Clinical Drug Review Program
- PA code "C" = PA required -Brand Required Instead of Generic
- PA code "D" = PA required -Respiratory Syncytial Virus Clinical Drug Review Program
For example, to view an alphabetically arranged list of all drugs included in the Mandatory Generic Program, start by selecting "PA Code" as the "Field", enter "8" as the "Value", and select "Description" as the "Sort By". When you click on "Search", your matches are displayed, and sorted by description.
Attention: Nursing Homes and Community Pharmacies
Return to Table of Contents
Pending Federal approval, effective on or about October 1, 2010, prescription drugs for Medicaid beneficiaries residing in nursing homes will be carved-out of the nursing home reimbursement rate and covered on a fee-for-service basis. Over the Counter (OTC) drugs and supplies will continue to be included in the nursing home reimbursement rate. Additional details will be published in the September 2010 Medicaid Update.
Mandatory Generic Drug Program Update
Return to Table of Contents
The New York State Medicaid Mandatory Generic Drug Program requires prior authorization for most brand-name prescription drugs with an A-rated generic equivalent. The list of Medicaid reimbursable drugs may be used to determine if a drug is included in the Mandatory Generic Drug Program. Drugs included in the Mandatory Generic Program are identified by a Prior Authorization code of 8 on the list of Medicaid reimbursable drugs. The list of Medicaid reimbursable drugs is available online at: http://www.emedny.org/info/formfile.html. This site can be checked for changes in prior authorization status, as the Department of Health will no longer publish a separate notification of changes in the Mandatory Generic Program.
PLEASE NOTE: Brand-name drugs that are on the Medicaid Preferred Drug List do not require prior authorization and are not subject to the Medicaid Mandatory Generic Program prior authorization requirements.
For pharmacy billing questions, please call (800) 343-9000.
Information regarding the Mandatory Generic Program is available online at: https://newyork.fhsc.com and www.nyhealth.gov, or by calling (877) 309-9493.
Policy Update: Dispense Brand Name
Drugs When Less Expensive Initiative
Return to Table of Contents
Effective April 26, 2010, New York Medicaid implemented a new cost containment initiative to promote the use of certain multi-source brand name drugs when the cost of the brand name drug is less expensive than the generic equivalent.
BRAND NAME DRUGS INCLUDED IN THIS PROGRAM:
- Will not require 'Dispense as Written' (DAW) or 'Brand Medically Necessary' on the prescription; and do not need to be billed using the NCPDP (408-D8) Dispense As Written/Product Selection Code of '1';
- Have a generic copayment; and are therefore in conformance with State Education Law which intends that patients receive the lower cost alternative;
- Have an enhanced dispensing fee (equal to generic dispensing fee);
- Will be paid at the Brand Name Drug reimbursement rate or usual and customary price, whichever is lower (neither the SMAC nor FUL will be applied);
- Will not require prior authorization.
Please keep in mind that drugs removed from this program may be subject to prior authorization requirements of other pharmacy programs; again promoting the use of the most cost-effective product.
FREQUENTLY ASKED QUESTIONS (FAQ):
QUESTION: What DAW code do I need to use when submitting a claim for a drug that is included in this program?
ANSWER: Reimbursement does not require the submission of a particular DAW code. Acceptable values for the Dispense As Written/Product Selection code are as follows:
- 0 = No product selection
- 1 = Substitution not allowed by prescriber*
- 4 = Substitution allowed - Generic Drug not in stock
- 5 = Substitution allowed - Brand Drug dispensed as a Generic
- 7 = Substitution not allowed - Brand Drug mandated by Law
- 8 = Substitution allowed - Generic Drug not available in the Marketplace
*Claims should only be submitted with a DAW code of '1' when the prescriber indicates in handwriting or by electronic means 'Dispense as Written' (DAW) and 'Brand Medically Necessary' on the prescription.
QUESTION: Will I need to obtain a new prescription if the drug is removed from the Dispense Brand Drugs When Less Expensive Program?
ANSWER: No. You will not need to obtain a new prescription if the generic alternative becomes the more cost effective option.
The current list of drugs included in this program may be viewed online at: http://www.nyhealth.gov/health_care/medicaid/program/pharmacy.htm or http://www.emedny.org/ under featured links, as well as in the Medicaid Pharmacy Provider Manual under the Provider Communication Link.
Attention: Medicaid and Family Health Plus Prescribers
Return to Table of Contents
Clinical Drug Review Program (CDRP) worksheets can help providers prepare their response to the information that is requested by call center representatives when obtaining a prior authorization for a CDRP drug. Please visit https://newyork.fhsc.com/ to access worksheets for the following drugs:
- Actiq/fentanyl citrate®
- Adcirca®*
- Fentora®
- Growth Hormones for enrollees 21 years of age and older*
- Lidoderm®
- Onsolis®
- Revatio®*
- Serostim®*
- Synagis®*
- Topical Immunomodulators (Protopic® and Elidel®)
- Zyvox®*
Please note: CDRP worksheets are for preparation purposes only and cannot be faxed. For drugs indicated above by an asterisk (*), only prescribers, not their authorized agents, can initiate prior authorization.
To obtain a prior authorization for one of the CDRP drugs listed above, please call (877) 309-9493 and select option #1 to speak with a clinical call center representative.
A complete list of preferred and non-preferred drugs subject to the Preferred Drug Program (PDP), is available online at: https://newyork.fhsc.com/. Click on the Preferred Drug List.
Questions related to Medicaid Pharmacy prior authorization programs should be directed to (877) 309-9493.
For billing questions, contact (800) 343-9000.
Reminder: Smoking Cessation Policy NYS Medicaid Pharmacy Benefit
Return to Table of Contents
- Smoking cessation therapy consists of prescription and nonprescription agents. Covered agents include nasal sprays, inhalers, Zyban (bupropion), Chantix (varenicline), over-thecounter nicotine patches and gum.
- Two courses of smoking cessation therapy per beneficiary, per year are allowed. A course of therapy is defined as no more than a 90-day supply (an original order and two refills, even if less than a 30-day supply is dispensed in any fill).
- If a course of smoking cessation therapy is interrupted, it will be considered one complete course of therapy. Any subsequent prescriptions would then be considered the second course of therapy.
- Some smoking cessation therapies may be used together. Professional judgment should be exercised when dispensing multiple smoking cessation products.
- Duplicative use of any one agent is not allowed (i.e., same drug and same dosage form and same strength).
- For all smoking cessation products, the beneficiary must have an order. A prescription is the terminology for an order of a prescription product. A fiscal order refers to an order, which looks just like a prescription written on a prescription blank, for an over-the-counter product.
- NYS Medicaid reimburses for over-the-counter nicotine patches. Prescription nicotine patches are no longer covered.
- Prescription smoking cessation agents are subject to the Mandatory Generic Drug Program. For example, brand name Zyban requires a prior authorization.
- Family Health Plus beneficiaries are eligible to receive prescription smoking cessation agents and over-the-counter smoking cessation agents by a fiscal order as of October 1, 2008.
RESOURCES:
- NYS Smokers' Quitline: (866) NY-Quits (866-697-8487)
- American Cancer Society: (800) 227-2345
- American Lung Association: (800) 585-4872
- Centers for Disease Control and Prevention: 1-800-CDC-4636 (800-232-4636)
- National Cancer Institute: 1-800-4-Cancer (800) 422-6237
For more information on the New York State Medicaid Smoking Cessation policy, please contact the Bureau of Pharmacy Policy and Operations at (518) 486-3209.
Diagnosis Code Requirement
Return to Table of Contents
As published in the June 2010 Medicaid Update, pharmacies are required to submit a diagnosis code on all claims for all durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) claims.
New York Medicaid policy requires the prescriber to provide a valid diagnosis code on all fiscal orders for durable medical equipments, prosthetics, orthotics, and supplies (DMEPOS).
In September 2010, New York Medicaid will begin implementation of claims editing to validate that the diagnosis code is appropriate for the DMEPOS item reported. For example, claims for diabetic test strips must include the prescriber's diagnosis of diabetes.
For billing questions, please call Computer Sciences Corporation at (800) 343-9000.
Medicaid & Family Health Plus Prescribers
Return to Table of Contents
Effective September 25, 2010, when providers call to request a prior authorization for the Preferred Drug Program (PDP) or the Clinical Drug Review Program (CDRP) they will be prompted to enter the following information, using their telephone key pad. Providers will then be transferred to a live call center representative:
- Prescriber NPI number
- Prescriber phone number
This change is intended to reduce the amount of time spent obtaining a prior authorization.
Please visit https://newyork.fhsc.com/ to obtain a Medicaid Pharmacy Prior Authorization Quick Punch guide that assists the providers in choosing the correct touchtone sequence for the appropriate situation.
For Medicaid Pharmacy prior authorization program questions, please call (877) 309-9493.
For billing questions, please contact the eMedNY Call Center at (800) 343-9000
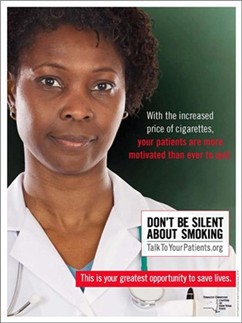
By providing counseling, pharmacotherapy, and referrals, you can double your patients' chances of successfully quitting. For more information, please visit www.talktoyourpatients.org or call the NY State Smokers' Quitline at 1-866-NY-QUITS (1-866-697-8487).
Do you suspect that a Medicaid provider or an enrollee has engaged in fraudulent activities?
Return to Table of Contents
Please Call: 1-877-87FRAUD or (212 417-4570)
Your call will remain confidential.
You can also complete a Complaint Form online at:
www.omig.state.ny.us

Provider Directory
Return to Table of Contents
Office of the Medicaid Inspector General:
http://www.omig.state.ny.us or call (518) 473-3782 with general
inquiries or 1-877-87FRAUD with suspected fraud complaints or allegations.
This contact information can also be used for Provider Self-Disclosures.
Questions about billing and performing MEVS transactions?
Please contact eMedNY Call Center at: (800) 343-9000.
Provider Training
To sign up for a provider seminar in your area, please enroll online at:
http://www.emedny.org/training/index.aspx
For individual training requests, call (800) 343-9000 or email: emednyproviderrelations@csc.com
Enrollee Eligibility
Call the Touchtone Telephone Verification System at any of the numbers below:
(800) 997-1111 (800) 225-3040 (800) 394-1234.
Address Change?
Questions should be directed to the eMedNY Call Center at: (800) 343-9000.
Fee-for-Service Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Rate-Based/Institutional Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Does your enrollment file need to be updated because you've experienced a change in ownership?
Fee-for-Service Providers please call (518) 402-7032
Rate-Based/Institutional Providers please call (518) 474-3575
Comments and Suggestions Regarding This Publication?
Please contact the editor, Kelli Kudlack, at:
medicaidupdate@health.state.ny.us
Medicaid Update is a monthly publication of the New York State Department of Health containing information regarding the care of those enrolled in the Medicaid Program.